Abstract
Undifferentiated embryonal sarcoma of the liver is a rare entity. It is a malignant primitive mesenchymal tumor seen in the pediatric age group often between 6 to 10 years of age. It involves the right lobe of the liver commonly and is usually asymptomatic. Acute presentation in these cases is secondary to its rupture/ wall dehiscence. Alfa fetoprotein, a tumor marker elevated in most of the hepatic malignant tumors is however normal in undifferentiated embryonal sarcoma. Imaging wise it is a large encapsulated multiseptated lesion. It shows a “paradoxical appearance” with a predominantly solid appearance on ultrasonography and cystic appearance on CT/MRI. This is a peculiar feature that can help in the early diagnosis of this entity. Besides, normal serum alfa fetoprotein levels favor its diagnosis. Hereby we present a case of a 5-year-old female child, presented with complaints of acute onset abdominal pain and distension which on imaging investigation showed a liver mass with typical paradoxical appearance on ultrasonography, CT and MRI as described.
Keywords: Undiffferentiated embryonal sarcoma of liver, Paradoxical imaging appearance, Computed tomography, Magnetic resonance imaging, Normal serum alpha-fetoprotein
Introduction
Undifferentiated embryonal sarcoma of the liver is a rare entity. It is a malignant primitive mesenchymal tumor seen in the pediatric age group often between 6 and 10 years. It shows a “paradoxical appearance” with a predominantly solid appearance on ultrasonography and cystic on computed tomography (CT)/magnetic resonance imaging (MRI). This is a peculiar feature that can help in the early diagnosis of this entity. Besides, normal serum alfa fetoprotein levels favor its diagnosis. Hereby we present a rare case of a 5-year-old female child, presented with complaints of abdominal pain and distension which on imaging investigation showed typical paradoxical appearance as described.
Case
A 5-year-old female child, presented with complaints of abdominal distension, pain for 7 days with prior history of constipation. There was no fever and vomiting.
On clinical examination, the patient was afebrile with a pulse rate of 130/min and respiratory rate of 45/min. CRT 3 seconds, blood pressure of 100/60 mmHg. SPO2 98% on room air. The patient was pale. On per abdominal examination, a hard mass was felt in the right upper quadrant (right hypochondriac region) with its lower border reaching up to iliac fossa. This area was tender on palpation. Neurologically patient was conscious, alert, and oriented. Respiratory and cardiovascular examination was within normal limits.
Ultrasonography done outside was suggestive of a large heterogeneous mass lesion, showing minimal vascularity on the Doppler study. This mass was predominantly solid with cystic areas within. However organ of origin could not be commented well, the possibility of origin from the liver was given.
The patient underwent contrast-enhanced CT, which showed, as large hypodense predominantly complex cystic mass lesion arising from the right lobe of the liver. This lesion showed predominantly peripheral progressive enhancement. There was a mass effect on the adjacent organs. Hyperdense content within the cystic component was suggestive of intralesional hemorrhage. A possible diagnosis of malignant space-occupying lesion was considered. Pet-Positron Emission Tomography (PET/CT) done for the patient showed predominant uptake in the peripheral portion of the lesion (Fig. 1).
Fig. 1.
A. Ultrasonography showing predominant solid appearance of the lesion with cystic spaces within. B. Axial Maximum Intensity Projection (MIP) image showing blood supply to the lesion from branch of hepatic artery. C, D, E. Axial Contrast enhanced computed tomography image showing cystic appearance of the lesion with predominant peripheral enhancement in arterial, venous and portal venous phases. F. Axial18-Fluro-Deoxy glucose PET/CT scan image showing predominant peripheral uptake within the solid component of the lesion.
Laboratory investigations revealed, Hemoglobin of 9.2 gm/dl, Packed Cell Volume (PCV) – 27.8, Total Leucocyte Count (TLC) 10,440, platelets – 43,600, creatinine 0.28, Prothrombin Time (PT) 14.5, International Normalised Ratio (INR) 1.28 and PT 23.8. Liver function tests were deranged with raised SGPT (74) and SGPT (84). Albumin 3.6 (3.8-5.4), Gamma Glutamyl Transpeptidase (GGTP) 106, total albumin 0.15, LDH 418 (135-250). Tumor markers including Alfa fetoprotein, Beta Human Chorionic Gonadotropin (b-HCG), and Carbohydrate Antigen (CA) 19-9 were normal.
For further characterization of the lesion, contrast-enhanced MRI was done. A fairly large, well-defined complex multiseptated mass lesion was identified occupying almost the entire right lobe of the liver. On T2 weighted images, this mass lesion appears heterogeneously hyperintense and shows multiple thick hypointense septae within. On T1-weighted images, this lesion appears predominantly isointense. Few areas of hemorrhage with blood-fluid levels were seen within. Patchy areas of restricted diffusion seen within this lesion showed heterogeneous, progressive enhancement on late arterial and venous phases. These areas were predominantly along its periphery. The lesion was supplied by a few twigs from the right hepatic artery. The capsular breach was seen along its inferior aspect. This lesion measured approximately 14.0 × 12.5 × 9.8 cm in maximum craniocaudal, transverse, and anteroposterior dimensions. There was compression of intrahepatic IVC and splaying of hepatic veins. There was compression of the right kidney, right renal artery, and renal vein with the mild displacement of the right adrenal gland and pancreas. A mild perihepatic collection representing hemoperitoneum was seen. Imaging morphology of this lesion was concerning for a neoplastic etiology, possibly undifferentiated embryonal cell sarcoma given paradoxical appearance on CT/MRI and ultrasonography along with normal AFP levels (Fig. 2).
Fig. 2.
A. Axial T2 weighted image showing a well-defined lesion in right lobe of liver appearing hyperintense with hypointense septations within. B. Axial T1W image showing hypointense lesion with fluid-fluid levels within suggestive of intralesional haemorrhage. C. Axial Diffusion weighted images showing restricted diffusion in periphery of lesion. D. Axial Apparent Diffusion Coefficient (ADC) images showing corresponding low values in periphery of lesion. E, F, G. Axial and coronal post contrast T1 weighted images showing progressive enhancement in arterial, portal venous and delayed phases.
Exploratory laparotomy was done. There was evidence of ruptured necrotic liver mass lesions with diffuse bleeding. It was seen displacing adjacent organs to left with compression of the right kidney. Hepatectomy could not be performed given profuse bleeding and poor access to porta. Hepatic artery ligation was done. A biopsy was taken and sent for histopathologic evaluation.
Following surgery, on day 3 liver function tests were repeated. SGOT and SGPT levels become normal (SGOT – 52 units/L, SGPT – 202 units/L).
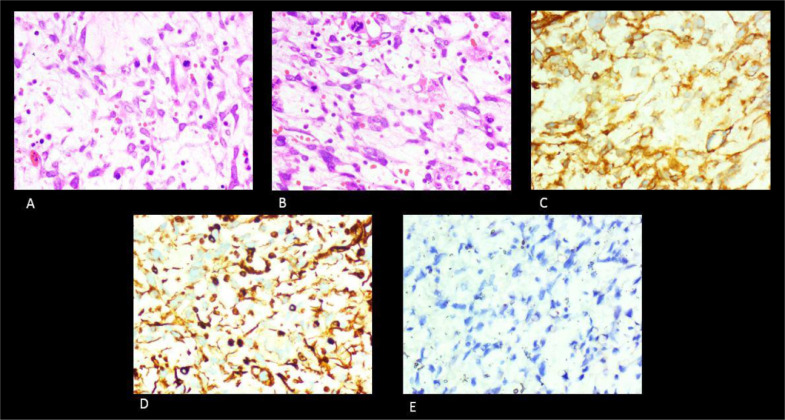
On histopathology, the tumor was composed of sheets of spindle cells having hyperchromatic nuclei, indistinct cytoplasm, and marked pleomorphism. Many cells were showing intracytoplasmic eosinophilic nuclei. Multinucleated and bizarre forms were noted. On histopathology, the tumor was composed of sheets of spindle cells having hyperchromatic nuclei, indistinct cytoplasm, and marked pleomorphism. Many cells were showing intracytoplasmic eosinophilic nuclei. Multinucleated and bizarre forms were noted. Immunohistochemistry showed strong membranous staining of tumor cells with CD10, Diffuse reactivity for vimentin in spindle cells. Staining for Myo D1 was negative. This was suggestive of undifferentiated embryonal sarcoma (Fig. 3).
Fig. 3.
A. 100X H& E stain, High power view shows marked pleomorphic tumor cells, bizarre cells with prominent Eosinophilic cytoplasm and few mitotic figures. Interspersed myxoid stroma with thin walled blood vessels are also seen.B. High power view (100X) showing typical presence of cytoplasmic Eosinophilic hyaline globules which are PAS positive and diastase resistant. C. Immunohistochemistry – Strong membranous staining of tumor cells with CD10 is seen. D. Immunohistochemistry – Diffuse reactivity for vimentin is seen in spindle cells. E. Immunohistochemistry – Negative staining for Myo D1 is seen.
Discussion
Undifferentiated embryonal sarcoma of the liver is a rare malignant primitive mesenchymal tumor. It was first described by the Stocker and Ishak in 1978. Incidence wise it is the third most common tumor in the pediatric age group accounting for 9%-15% of cases. It is predominantly seen in older children between 6 and 10 years of age, however, occasionally adults are also affected. No significant gender-wise affliction is seen. The right lobe of the liver is involved most commonly as seen in our case also. [1], [2], [3]
It is generally asymptomatic in children. However, it can present as an abdominal mass. Abdominal pain and discomfort can also be other presentations. Acute presentation in these cases is secondary to its rupture/wall dehiscence. Tumor markers such as alpha-fetoprotein are within normal limits. [3,4]
On radiographs, a large soft tissue density can be seen in the right upper quadrant. Lateral displacement of the adjacent bowel loops can be seen [3].
Ultrasonography is a readily available modality. It shows a large encapsulated tumor, many a time it measures more than 10 cm at presentation. It can be seen as a mixed echogenicity mass lesion. A solid and cystic component is often seen within. Other presentations can be as isolated large cystic mass. In our case, the lesion was predominantly solid with cystic components within with minimal vascularity on the Doppler study and a size of more than 10 cm. Echogenic mural nodules can be seen within which are predominantly hyperechoic [1,3].
The peculiar feature of this lesion is the different internal architecture seen on CT and ultrasonography images. It was described by Moor et al on ultrasonography these lesions appear solid with a cystic appearance on computed tomography images. It was also found that there is a correlation between the solid appearance of the tumor on ultrasonography and the pathological findings [2]. On MR imaging, these appear hypointense on T1W, hyperintense on T2W images following cystic intensity. As the tumor is capsulated, this capsule appears hypointense on both T1W and T2W images. If intralesional hemorrhage is present it can appear as a hyperintense component on T1W images with different signal intensity depending on the stage of hemorrhage. The fluid-fluid level can be seen within. As is seen with the CT scan, on postcontrast images peripheral and septal enhancement is seen within the solid component these features were corresponding with our case [4]. On postcontrast images no obvious enhancement is seen within the mass, however peripheral enhancement within the solid component as well as within the septae can be seen [3]. These features were matching with our case.
Similarly, it shows the corresponding T2W hyperintense signal on T2W on MRI. In our case, the lesion was predominantly hypodense with cystic in appearance. The scanty solid component was also seen peripherally which was showing postcontrast enhancement. Among the various imaging presentations, it presents as a hypodense mass lesion. Sometimes hemorrhagic or necrotic components can be seen within [2,3].
Buetow et al studied the details in imaging and Histopathological evaluation. These tumors showed similar solid appearance on gross specimen as that of the ultrasonography and however these are cystic in appearance on CT/MRI, proving the discordance in imaging findings. This cystic appearance on CT and MRI is predominantly due the abundant myxoid stroma resulting in increased water content [2].
Differentials for this condition can include mesenchymal hamartoma of the liver, however, the age of presentation helps in differentiation. Hydatid cyst in an endemic region, abscess, hepatoblastoma, or HCC with degeneration and cystic metastasis can be other differential diagnoses [4].
In our case, the mass was predominantly solid on ultrasonography and cystic on CT and MRI. With FDG uptake peripherally within the solid component. Also, normal levels of alfa-fetoprotein and b-HCG were seen. These features were in favor of undifferentiated embryonal sarcoma in this age group, accordingly, the diagnosis was given which matched with the final Histopathological findings.
References
- 1.Gao J, Fei L, Li S. Undifferentiated embryonal sarcoma of the liver in a child: a case report and review of the literature. Oncol Lett. 2013;5(3):739–742. doi: 10.3892/ol.2012.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sodhi KS, Bekhitt E, Rickert C. Paradoxical hepatic tumor: Undifferentiated embryonal sarcoma of the liver. Indian J Radiol Imaging. 2010;20(1):69–71. doi: 10.4103/0971-3026.59760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim M, Tireno B, Priscilla J. Undifferentiated embryonal sarcoma of the liver. American Journal of Roentgenology. 2008;190(4):W261–W262. doi: 10.2214/AJR.07.3058. [DOI] [PubMed] [Google Scholar]
- 4.Chung EM., Lattin GE., Jr RC, Lewis RB, Marichal-Hernández C, Shawhan R. From the archives of the AFIP: pediatric liver masses: radiologic-pathologic correlation Part 2. Maliganant tumours. Radiographics. 2011;31(2):483–507. doi: 10.1148/rg.312105201. [DOI] [PubMed] [Google Scholar]