Clinical vignette
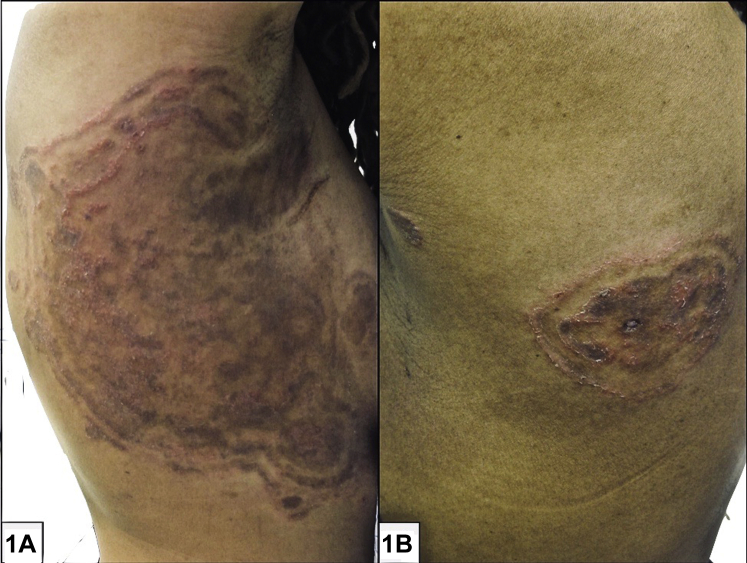
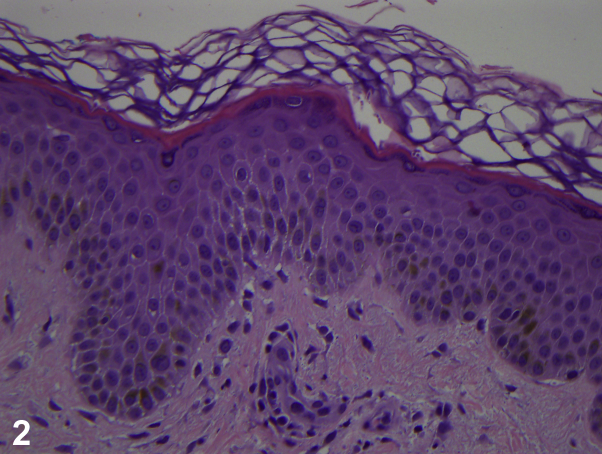
A 48-year-old black woman with a history of infiltrating ductal breast carcinoma, now in remission, presented with a 6-month history of enlarging, pruritic, violaceous, annular plaques composed of concentric rings on the right flank, back, and right thigh (Fig 1). The rash initially started on her right flank and worsened during several months despite application of triamcinolone 0.1% cream daily. A punch biopsy was taken from the thigh (Fig 2).
Fig 1.
Fig 2.
Question 1: Which of the following is the best diagnosis?
-
A.
Erythema gyratum repens
-
B.
Superficial erythema annulare centrifugum
-
C.
Tinea pseudoimbricata
-
D.
Metastatic breast carcinoma
-
E.
Nummular dermatitis
Answers:
-
A.
Erythema gyratum repens—Incorrect. Erythema gyratum repens is a paraneoplastic figurate erythema typically associated with breast, lung, and esophageal cancer that presents within 1 year of a cancer diagnosis. Tinea pseudoimbricata and erythema gyratum repens can have similar morphology, with pruritic, annular, erythematous plaques composed of concentric rings with a wood-grain appearance and fine scale. Although histopathology is nonspecific, there are no fungal elements as observed in tinea pseudoimbricata. Erythema gyratum repens expands more rapidly than tinea pseudoimbricata and does not worsen with steroids.1
-
B.
Superficial erythema annulare centrifugum—Incorrect. Superficial erythema annulare centrifugum is a figurate erythema characterized by erythematous annular expanding plaques with trailing scale, not concentric rings. It is associated with dermatophyte infections, drugs, and malignancies. Histopathology is nonspecific, but tight “coat sleeving” of lymphocytes around superficial vessels is suggestive.1
-
C.
Tinea pseudoimbricata—Correct. Tinea pseudoimbricata is a dermatophytosis with the same clinical appearance of multiple concentric rings as tinea imbricata.2 Unlike tinea imbricata, which is caused by Trichophyton concentricum, tinea pseudoimbricata is caused by T tonsurans and other dermatophytes.2 Tinea pseudoimbricata is thought to be a form of tinea incognito associated with long-term topical steroid use.2,3 Histopathology is usually nonspecific but may show hyphae in the stratum corneum.
-
D.
Metastatic breast carcinoma—Incorrect. Cutaneous metastases usually present suddenly as multiple firm, dark, painless papulonodules, located on the chest or involving mastectomy scars.4
-
E.
Nummular dermatitis—Incorrect. Nummular dermatitis classically presents as coin-shaped eczematous plaques on the extremities. It would not present with concentric rings.
Question 2: Which of the following is the likely causative organism?
-
A.
T tonsurans
-
B.
T concentricum
-
C.
T mentagrophytes
-
D.
Epidermophyton floccosum
-
E.
Microsporum canis
Answers:
-
A.
T tonsurans—Correct. T tonsurans is the most frequently reported cause of tinea pseudoimbricata, although other species have been reported to cause lesions of this morphology, including T mentagrophytes and certain Microsporum species.5 T tonsurans is the most common cause of tinea capitis in the United States and is also a frequent cause of tinea corporis.1 It is thought that local immunosuppression contributes to the development of concentric rings in this condition.2
-
B.
T concentricum—Incorrect. T concentricum causes tinea imbricata. This organism is usually endemic to the Pacific Islands and Southeast Asia. The increasing frequency of international travel has made this organism more relevant to physicians in other countries.6
-
C.
T mentagrophytes—Incorrect. T mentagrophytes is known to cause tinea corporis, tinea cruris, inflammatory tinea pedis, and tinea barbae and is associated with exposure to small mammals.1
-
D.
E floccosum—Incorrect. E floccosum is a common cause of moccasin-type and interdigital tinea pedis in addition to tinea cruris, unguium, and manuum. It is thought to be responsible for outbreaks of tinea cruris associated with lockers rooms and dormitories.1
-
E.
M canis—Incorrect. M canis is the second most common cause of tinea capitis in the United States and is a very common cause of tinea capitis worldwide. It is associated with exposure to both cats and dogs. This organism also causes tinea corporis and tinea faciei.1
Question 3: Which of the following is the next best step in the management of this patient?
-
A.
Topical ketoconazole 2% cream twice daily for 4 weeks
-
B.
Oral terbinafine 250 mg daily for 4 weeks
-
C.
Oral ketoconazole 200 mg daily for 4 weeks
-
D.
Topical clobetasol 0.05% ointment twice daily for 2 weeks
-
E.
Oral prednisone 60 mg daily for 3 weeks
Answers:
-
A.
Topical ketoconazole 2% cream twice daily for 4 weeks—Incorrect. A topical antifungal agent alone would not be appropriate, given the extensive areas of involvement and previous extended treatment with topical corticosteroids.
-
B.
Oral terbinafine 250 mg daily for 4 weeks—Correct. Oral terbinafine is one of the most effective treatments for tinea imbricata and tinea pseudoimbricata.2,4 Oral antifungal therapy can be combined with topical antifungals for an enhanced cure rate.4
-
C.
Oral ketoconazole 200 mg daily for 4 weeks—Incorrect. Although oral ketoconazole may be effective in the treatment of dermatophytosis, the Food and Drug Administration has applied a black-box warning because of the risk of serious hepatotoxicity potentially requiring liver transplant.7 The oral form of this medication is not indicated to treat skin or nail infections. It is contraindicated in patients with acute or chronic liver failure.
-
D.
Topical clobetasol 0.05% ointment twice daily for 2 weeks—Incorrect. Although topical corticosteroids may be helpful in cases of erythema gyratum repens, their use in tinea imbricata or tinea pseudoimbricata would be expected to worsen the disease.3
-
E.
Oral prednisone 60 mg daily for 3 weeks—Incorrect. Oral corticosteroids may be helpful in cases of erythema gyratum repens but would not be indicated for the treatment of tinea imbricata or tinea pseudoimbricata. Systemic immunosuppression could potentially worsen the progression of a dermatophyte infection.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Bolognia J.L., Schaffer J.V., Cerroni L., editors. Dermatology. 4th ed. Elsevier; London, United Kingdom: 2018. [Google Scholar]
- 2.Kansal N.K. Tinea pseudoimbricata: a striking “ring-within-a-ring” form of corticosteroid-modified dermatophytosis. Indian Dermatol Online J. 2019;10(3):354. doi: 10.4103/idoj.IDOJ_169_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta V., Bhatia R., Sondhi P., Mahajan R. 'Ring-within-a-ring' appearance: morphological clue to topical steroid abuse in dermatophytosis. J Eur Acad Dermatol Venereol. 2017;31(1):e2–e3. doi: 10.1111/jdv.13576. [DOI] [PubMed] [Google Scholar]
- 4.Waldman R.A., Finch J., Grant-Kels J.M., Stevenson C., Whitaker-Worth D. Skin diseases of the breast and nipple part I: benign and malignant tumors. J Am Acad Dermatol. 2019;80(6):1467–1481. doi: 10.1016/j.jaad.2018.08.066. [DOI] [PubMed] [Google Scholar]
- 5.Rao A.G., Datta N. Tinea corporis due to Trichophyton mentagrophytes and Trichophyton tonsurans mimicking tinea imbricata. Indian J Dermatol Venereol Leprol. 2013;79(4):554. doi: 10.4103/0378-6323.113109. [DOI] [PubMed] [Google Scholar]
- 6.Leung A.K.C., Leong K.F., Lam J.M. Tinea imbricata: an overview. Curr Pediatr Rev. 2019;15(3):170–174. doi: 10.2174/1573396315666190207151941. [DOI] [PubMed] [Google Scholar]
- 7.Food and Drug Administration FDA drug safety podcast: FDA warns that prescribing of nizoral (ketoconazole) oral tablets for unapproved uses including skin and nail infections continues; linked to patient death, Available at. https://www.fda.gov/drugs/fda-drug-safety-podcasts/fda-drug-safety-podcast-fda-warns-prescribing-nizoral-ketoconazole-oral-tablets-unapproved-uses