Abstract
A 71-year-old male with history of clear cell renal cell carcinoma (RCC) 6-years status post nephrectomy presented for gross hematuria. Cystoscopy revealed a bulge of the right ureteral orifice, and transurethral resection confirmed RCC metastasis to the ureteral stump. Ureterectomy with bladder cuff excision was performed, and the patient is currently undergoing aggressive imaging surveillance. This is the 57th case of metastasis of RCC to the ureteric stump, and this case occurred beyond baseline surveillance recommendation of five years. Potential mechanisms of metastasis of RCC are reviewed, and RCC surveillance is discussed.
Keywords: Renal cell carcinoma, Ureteric metastasis, Renal cell carcinoma surveillance
Introduction
Renal cell carcinoma (RCC) accounts for the vast majority of renal malignancies. Partial or radical nephrectomy is often curative for local disease. However, metastasis occurs in up to 50% of patients who undergo this procedure.1 Metastases may arise in any organ and may occur beyond recommended baseline durations of surveillance.
We report a rare case of metachronous distal ureteral stump metastasis occurring more than six years after open radical nephrectomy.
Case presentation
In October 2018, a 71-year-old male presented to urgent care for an episode of gross hematuria. Patient had a history significant for right radical nephrectomy in August 2012 for Fuhrman grade III clear cell renal cell carcinoma [pT3aNXM0] (Fig. 1) followed by surveillance. Surveillance studies from 2012 to 2017 were negative with stable renal function. The patient had an active lifestyle as a runner and regular hiker.
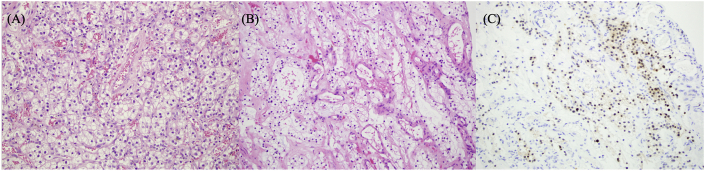
Fig. 1.
Light microscopy
(A) Primary tumor of right kidney. Hematoxylin and eosin (H&E) stain, x20 magnification shows clear cells with grade III WHO/ISUP based on obvious nucleoli and larger nuclei.
(B) Tumor of right distal ureter. H&E stain, x20 magnification shows clear cell carcinoma with smaller nuclei finalized as grade II WHO/ISUP.
(C) Tumor of right distal ureter. PAX8 nuclear marker, x20 magnification, expressed by tumor cells in a scattered nuclear pattern.
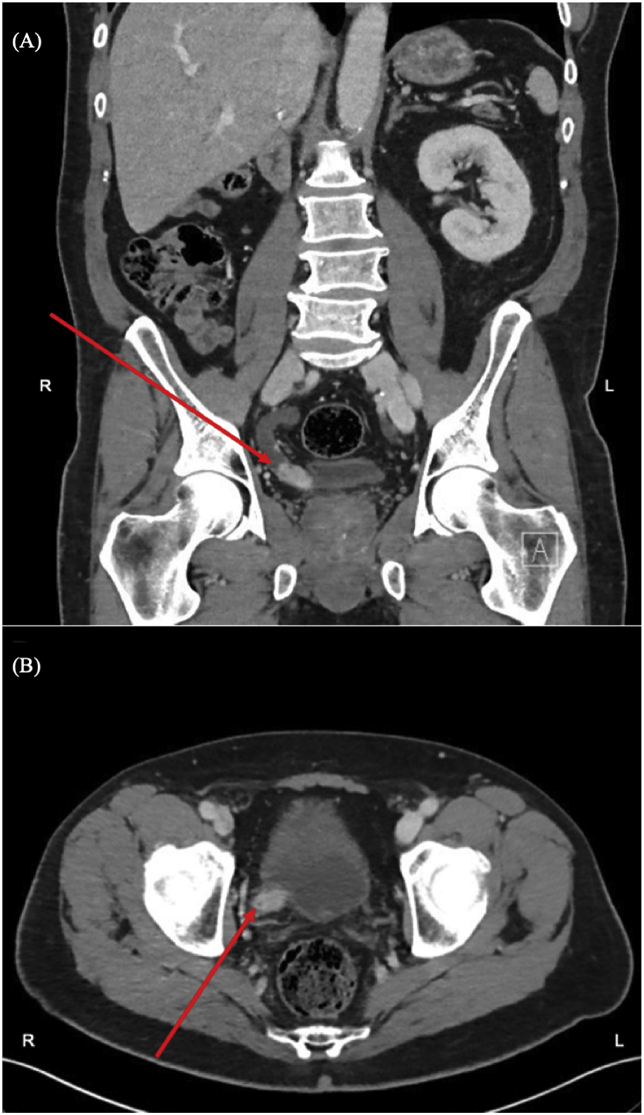
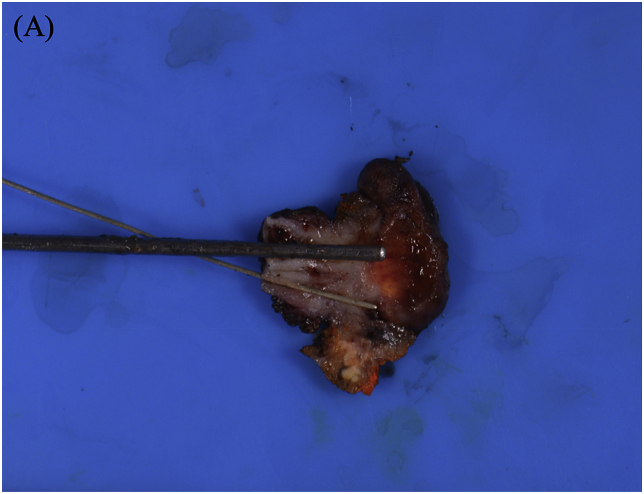
At the time of presentation, a computed tomography scan of the abdomen and pelvis revealed a “right ureteral remnant dilation with enhancing soft tissue mass at the distal ureter, abutting the bladder wall at the ureterovesical junction” (Fig. 2). No contralateral renal lesions or other metastatic lesions, including within the surgical bed, were noted on imaging. Cystoscopy subsequently identified a bulge of the right ureteral orifice due to underlying mass, but no obvious intravesical tumors. Transurethral resection was performed and identified underlying tumor that returned as clear cell renal cell carcinoma (ccRCC) (Fig. 1). Subsequent immunohistochemical (IHC) staining of neoplastic cells revealed scattered nuclear positivity for PAX8 (Fig. 1), positivity for cytokeratins AE1/AE3, and nonreactivity for CK7, which suggested a renal primary consistent with metastatic recurrence. The patient then underwent right ureterectomy with bladder cuff excision showing a 2.3 cm × 1.5 cm x 1.9 cm projection of tumor from the orifice into the bladder lumen (Fig. 3). The tumor was diagnosed as Fuhrman grade II clear cell renal cell carcinoma, and margins of the ureter and bladder cuff were free of tumor. Because histology and immunohistochemical staining were adequate for diagnosis, no further testing for genetic or molecular characteristics was performed in this case. Pelvic lymphadenectomy on the right was negative for malignancy.
Fig. 2.
Radiographic Imaging. Coronal view (A) and axial view (B) of arterial phase on CT reveals right ureteral remnant dilation with enhancing soft tissue mass (arrows) at the distal ureter, abutting the bladder wall at the ureterovesical junction.
Fig. 3.
Distal right ureters and bladder cuff. (A) Gross photograph of the parallel duplicated ureters involved by tumor as they enter the bladder wall at two separate ureteral orifices.
Discussion
Renal cell carcinoma (RCC) is the most common renal malignancy, with clear-cell (ccRCC) type being its most common subtype. Metastases occur in up to 50% of those with ccRCC, and metastatic implantation can occur in any location, the most common of which are lung, bone, regional lymph nodes, and liver.1 Metastasis within the genitourinary tract is a very rare event. This is the 57th reported case of ureteric metastasis of RCC. The timing of detection of metastasis to the ureteric stump has ranged from only months to more than 8 years following radical nephrectomy.2
Mechanisms underlying the metastatic spread of RCC within the urinary tract remain a subject of debate. Multiple mechanisms have been proposed, including hematogenous spread through systemic circulation, lymphatic dissemination, and intraluminal dissemination of cells with seeding of distal urothelium.3 While any are possible in this case, the presence of tumor projecting into the ureter and bladder lumen, as well as the absence of distant metastases and absence of pelvic lymph node involvement are most consistent with the intraluminal dissemination theory, which would allow for anterograde spread of tumor cells with implantation into distal ureteral urothelium. In future cases, molecular and biologic studies of primary and metastatic tumors may offer greater understanding of mechanisms of RCC metastasis within the genitourinary tract, especially in cases like ours in which there is extended length of time to recurrence after nephrectomy.
To guide surveillance strategies of localized renal neoplasms, the American Urologic Association offers standardized recommendations for follow-up monitoring of localized renal neoplasms. For high-risk tumors (pT2-4N0 Nx or any T N+), recommended follow-up consists of initial baseline chest and abdominal scan (CT or MRI) within three to six months following surgery.4 For the following three years, imaging (US, CXR, CT, or MRI) should be performed every six months, and after three years, should be continued annually thereafter to year five.4 This surveillance is recommended due to the high risk of local and metastatic recurrence (~30–70%) of moderate-to high-risk tumors.4 Site-specific imaging is recommended as warranted by clinical symptoms suggestive of recurrent or metastatic spread.4 Considering these guidelines and the follow-up that our patient received, it is noteworthy that our patient, who had a high-risk tumor, developed metastasis at a date beyond the recommended surveillance time period of 5 years.
Due to the rarity of RCC metastasis to the ureter, there is no consensus regarding the most appropriate therapy. However, surgical excision of RCC metastasis to the bladder has been shown to improve prognosis,3 so it is logical to assume that excision of metastasis to the distal ureter will offer similar benefit. Additionally, for solitary bladder metastases, targeted adjuvant therapy is typically not necessary and is instead reserved for those patients in whom systemic metastatic spread is detected.5 By a similar logic, this management may offer similar outcomes in patients with solitary ureteric metastasis. After metastasectomy, our patient is being monitored every 3–6 months with imaging.
Conclusion
The current study describes a rare case of RCC metastasizing to the residual ureteric stump more than 6 years after radical nephrectomy. While surveillance post-nephrectomy certainly improves detection of RCC metastasis, our patient's RCC recurrence, occurring beyond recommended surveillance duration, emphasizes the unpredictability of this disease, underscores the importance of physician and patient awareness of patient health changes that may suggest metastatic disease, and suggests a potential benefit from prolonged surveillance for some patients with RCC.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
Acknowledgements
None.
Contributor Information
Alex Oserowsky, Email: aoxfh@health.missouri.edu.
Devin Allison, Email: dra246@health.missouri.edu.
Stephen Weinstein, Email: weinsteinS@health.missouri.edu.
Van Nguyen, Email: nguyenvt@health.missouri.edu.
Katie S. Murray, Email: murraykat@health.missouri.edu.
References
- 1.Janzen N.K., Kim H.L., Figlin R.A., Belldegrun A.S. Surveillance after radical or partial nephrectomy for localized renal cell carcinoma and management of recurrent disease. Urol Clin. 2003;30(4):843–852. doi: 10.1016/s0094-0143(03)00056-9. [DOI] [PubMed] [Google Scholar]
- 2.Macleod R., Kheirandish P., Ondego C., Biyani C.S. Chromophobe renal cell carcinoma recurrence in the ureter: a late presentation of a rare metastasis. Canad Urol Assoc J. 2015;9:E687–E689. doi: 10.5489/cuaj.3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumoto K., Hayakawa N., Nakamura S., Oya M. Bladder metastasis from renal cell carcinoma: retrospective analysis of 65 reported cases. Clin Exp Metastasis. 2015;32:135–141. doi: 10.1007/s10585-015-9698-1. [DOI] [PubMed] [Google Scholar]
- 4.Donat S.M., Diaz M., Bischoff J.T. Follow-up for clinically localized renal neoplasms. J Urol. August 2013:407–416. doi: 10.1016/j.juro.2013.04.121. [DOI] [PubMed] [Google Scholar]
- 5.Zhang M., Wah C., Epstein J. Metastatic renal cell carcinoma to the urinary bladder: a report of 11 cases. Am J Surg Pathol. 2014;38(11):1516–1521. doi: 10.1097/PAS.0000000000000257. [DOI] [PubMed] [Google Scholar]