Abstract
The availability of clinical-relevant large animal models for research in wound healing study is limited. Although a few reports described the wound dressing fixation method using polyurethane foam in patients, no animal studies were conducted to investigate efficacy of the polyurethane foam in grafted burn wounds. In the present study, we report a simple fixation method of grafted burned skin using polyurethane foam dressing (Allevyn Non-Adhesive, smith & nephew, UK) in a clinically relevant ovine grafted burn wound model. The dressing was removed at postoperative day 7 after skin graft. The grafted skin was completely engrafted without any complications. This method was safe and easy to perform and associated with good engraftment without any complications. We believe that the polyurethane foam fixation method may be successfully used in clinical practice as well as in preclinical studies for grafted burn wound repair and regeneration research.
Keywords: Sheep, Burn wound healing, Autologous skin graft, Allogenous skin graft, Non-adhesive hydrocellular foam dressing, Polyurethane foam
Highlights
-
•
Polyurethane foam was effective for fixation of grafted skin in ovine burn wounds model.
-
•
Histopathology of ovine grafted skin model was similar to that of human.
-
•
Ovine is considered as a clinical-relevant animal model for wound regeneration research.
-
•
The polyurethane foam method can potentially be translated to clinical practice.
1. Introduction
Physicians face significant challenges in the management of burn patients. Delayed and poor burn wound healing leads to high mortality and causes hypertrophic scarring in survivors decreasing their quality of life [1]. For better management of burn wound care, development of a clinically relevant large animal burn wound healing model is of particular interest. Such models offer better translational approaches in this specific field.
Although the swine model of burn wound healing is available, and similarities of swine and human skin structures are well known, the ovine model has several advantages; sheep are easy to work with, and no aggressive sedation for all manipulations are needed. The ovine model enables us to mimic a clinical situation—escharectomy, grafting, wound biopsy sampling, intermittent wound assessment (blood flow by laser Doppler, photography for Planimetry assay), as well as monitoring hemodynamics (i.e. Swan-Ganz, arterial and venous catheters). In addition, the ovine model does not require special dressing. Sheep do not rub the wounds against the cage wall or roll over on the wounds. Finally, the ovine wound healing pattern, the anatomy of their organs, and their responses to inflammation are similar to those in humans [[2], [3], [4], [5], [6]].
Since Blair and Brown introduced the basics of the skin grafting in 1929 [7], the techniques and technology are significantly evolved requiring burn surgeons to exhibit high skills and adequate experiences in skin grafting procedures, such as escharectomy, donor skin harvesting and grafting, as well as graft fixation for favorable outcomes. We have previously reported the use of traditional tie-over dressings with gauze for grafted burn wound healing studies in sheep [8]. However, the use of conventional tie-over dressing is associated with intense labor and long operative time. Although various tie-over dressing substitutes, such as polyurethane foam or negative pressure wound therapy, have been reported [[9], [10], [11]], the conventional tie-over method is still used widely. One of the reasons for this might be related to the limited availability of clinical-relevant animal models comparing pro and cons of various tie-over methods to other techniques of graft fixation.
In the present study we introduce a simple skin graft fixation method using a polyurethane foam dressing in an ovine burn model. We aimed to mimic the clinical practice for preparation of burn wound and autografting. We believe that the method enables investigators to accomplish their research goals for effective wound repair and regeneration.
2. Materials and methods
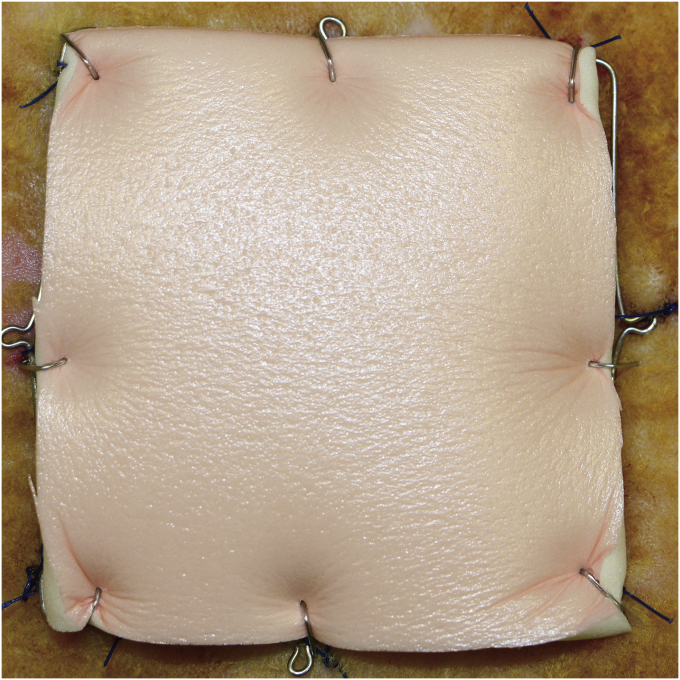
In the present study, we used the polyurethane foam dressing (Allevyn Non-Adhesive, smith & nephew, UK) for fixing grafted skin in an ovine burn wound model (Fig. 1). We used female Merino sheep (30–40 kg, approximately 3 years old; Talley Ranch, Bastrop, TX). This study was conducted in adherence with the guidelines detailed in the NIH Guide for the Care and Use of Laboratory Animals. The study was reviewed and approved by the Institutional Animal Care and Use Committee of the University of Texas Medical Branch at Galveston.
Fig. 1.
The grafted skin was fixation on the excised burn wound with surgical skin stapler. Then, the trimmed polyurethane foam was fixed on the grafted skin. The second foam was then overlapped on the first foam and fixed on the surround fire flame.
2.1. Skin grafting and polyurethane foam fixation
Full-thickness flame burn sites of 25 cm2 were made on the dorsum under anesthesia as described previously [3]. 24 h after burn, the escharectomy to the fascia was performed, and 30/1000 inches autologous split-thickness skin was harvested, meshed, and grafted to the wounds. The grafted skin was fixed with skin stapler (Manipler AZ, B.Braun, GER, Fig. 2A). Then the polyurethane foam was trimmed to fit the wound size, overlaid onto the wound, and fixed with skin stapler directly onto the grafted skin. Thereafter, a slightly bigger second foam was overlapped on the first foam as shown in Fig. 1. The second foam was fixed with skin stapler to surround the wire frame. Polyurethane foams were removed 7 days after the dressing.
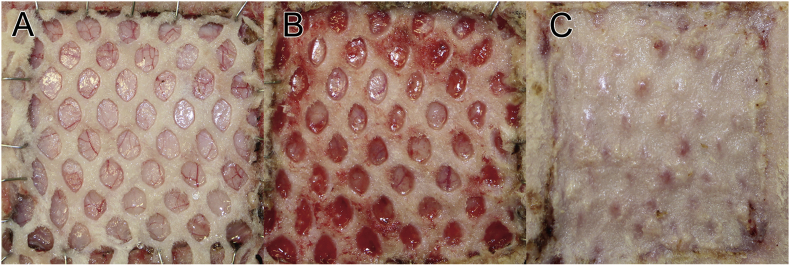
Fig. 2.
(A) Intraoperative finding after split-thickness skin graft (STSG). After the escharectomy, 0.03 inches autologous split-thickness skin were harvested, meshed, and grafted to the wounds using surgical stapler. The grafted skin was fixed with 2 pieces of polyurethane foam. (B) Postoperative finding 8 days after STSG. The fixation was removed at postoperative day 7. The grafted split skin graft was observed to be completely engrafted to the wound without any complications. (C) Postoperative finding 14 days after STSG. Favorite re-epithelialization was observed.
3. Result
As shown in Fig. 2B, the grafted skin was firmly attached to the wound bed and no wound complications such as hematoma, infection, and skin necrosis were observed, indicating that the wound dressing with double foam was sufficient to fix the grafted skin with proper pressure applied. The wound was completely healed 14 days after the dressing (Fig. 2C).
4. Discussion
The main advantages of the present method are: it is simple, easy, safe to perform, timesaving, does not require specific instruments, and most importantly it enables a firm attachment of the graft leading to the successful acceptance of the grafted skin. In the present study, we used wire frame to prevent possible wound contraction in order to more precisely assess the wound healing pattern. We have also fixed the second polyurethane foam to the wire to apply a proper pressure to the wounds.
Yamamoto et al. used a rubber band tie-over dressing in the ovine large flame burn and grafted wound healing model [3]. The rubber band method is suitable for large grafted burn wounds, and its efficacy has been shown in clinical studies [12]. However, the tie-over dressing is associated with certain disadvantages because the rubber band pressure varies depending on both the wound and rubber sizes. The high pressure leads to wound overcompression, while low pressure results in displacement of grafts [13]. It has been reported that the optimal tie-over dressing pressure is 2–10 mmHg [9]. It has been also suggested that high pressure is not critical for favorable graft taking.
5. Conclusion
The results of the present study report polyurethane foam as an effective tool for fixation of grafted skin in small sized wounds. The method can potentially be translated to clinical practice. The limitation of the present study is that the study did not compare the efficacy of simple polyurethane dressings to those using the traditional tie-over method. Secondly, we did not test the efficacy of the polyurethane dressing in large burn wounds. Future research is warranted to address these limitations.
Declartion of Competing of Interest
The authors declare no competing interests.
Acknowledgements
The authors thank the staff of the Translational Intensive Care Unit at the University of Texas Medical Branch at Galveston for their valuable assistance in conducting these studies, and Ms. Clemmie White–Matthews for the editorial assistance in preparing this article. Dr. Enkhbaatar received funding from the Shriners of North America grant # 84050.
Footnotes
Peer review under responsibility of the Japanese Society for Regenerative Medicine.
References
- 1.Finnerty C.C., Jeschke M.G., Branski L.K., Barret J.P., Dziewulski P., Herndon D.N. Hypertrophic scarring: the greatest unmet challenge after burn injury. Lancet. 2016;388(10052):1427–1436. doi: 10.1016/S0140-6736(16)31406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Enkhbaatar P., Pruitt B.A., Suman O., Mlcak R., Wolf S.E., Sakurai H. Pathophysiology, research challenges, and clinical management of smoke inhalation injury. Lancet. 2016;388(10052):1437–1446. doi: 10.1016/S0140-6736(16)31458-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamamoto Y., Enkhbaatar P., Sakurai H., Rehberg S., Asmussen S., Ito H. Development of a long-term ovine model of cutaneous burn and smoke inhalation injury and the effects of early excision and skin autografting. Burns. 2012;38(6):908–916. doi: 10.1016/j.burns.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niimi Y., Matsumine H., Fukuda S., Salsbury J.R., Niimi Y., Herndon D.N. Surgical anatomy of ovine facial and hypoglossal nerves for facial nerve reconstruction and regeneration research: an experimental study in sheep. Microsurgery. 2020;40:51–58. doi: 10.1002/micr.30405. [DOI] [PubMed] [Google Scholar]
- 5.Sakurai H., Nozaki M., Traber L.D., Hawkins H.K., Traber D.L. Microvascular changes in large flame burn wound in sheep. Burns. 2002;28(1):3–9. doi: 10.1016/s0305-4179(01)00067-5. [DOI] [PubMed] [Google Scholar]
- 6.Niimi Y., Fukuda S., Gilbert R.S., Baljinnyam T., Niimi Y., Matsumine H. Surgical anatomy of the ovine sural nerve for facial nerve regeneration and reconstruction research. Sci Rep. 2019;9(1):10564. doi: 10.1038/s41598-019-46661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blair V.P., Brown J.B. The use and uses of large split skin grafts of intermediate thickness. Surg Gynecol Obstet. 1929;49:82. [Google Scholar]
- 8.Ito H., Asmussen S., Traber D.L., Cox R.A., Hawkins H.K., Connelly R. Healing efficacy of sea buckthorn (Hippophae rhamnoides L.) seed oil in an ovine burn wound model. Burns. 2014;40(3):511–519. doi: 10.1016/j.burns.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Sakurai A., Hashikawa K., Yokoo S., Terashi H., Tahara S. Simple dressing technique using polyurethane foam for fixation of skin grafts. Dermatol Surg. 2007;33(8):976–979. doi: 10.1111/j.1524-4725.2007.33202.x. [DOI] [PubMed] [Google Scholar]
- 10.Niimi Y., Ito H., Sakurai H. Negative-pressure wound therapy for fixing full-thickness skin graft on the thumb. JPRAS Open. 2018;18:22–27. doi: 10.1016/j.jpra.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niimi Y., Mori S., Takeuchi M. A new procedure for wrapped-negative pressure wound therapy for congestion after arterialized venous flap surgery. Clin Med Insights Case Rep. 2017;10 doi: 10.1177/1179547617747279. 1179547617747279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng L.F., Lee J.T., Chou T.D., Chiu T.F., Sun T.B., Wang C.H. Experience with elastic rubber bands for the tie-over dressing in skin graft. Burns. 2006;32(2):212–215. doi: 10.1016/j.burns.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 13.Flowers R.S. Unexpected postoperative problems in skin grafting. Surg Clin. 1970;50(2):439–456. doi: 10.1016/s0039-6109(16)39092-2. [DOI] [PubMed] [Google Scholar]