To reduce the risk of overwhelming their healthcare systems during the COVID-19 pandemic, many countries are postponing medical services and procedures considered as “non-essential” or “deferrable”. However, this practice could eventually contribute to increasing the burden due to other medical conditions.
With specific regard to hepatitis C virus (HCV) infection, the availability of a safe and effective cure has led the World Health Organization (WHO) to set ambitious goals for eliminating it as a public-health threat by 2030. However, because of the COVID-19 pandemic, deferring HCV treatment has become an almost universal practice. Healthcare system has been placed under enormous stress, and entire hospitals and wards have been providing care exclusively for individuals with this disease. For this reason, the National Health Service must reassess its priorities and probably redistribute funding, so that there may not be sufficient resources for other public-health concerns, such as the elimination of HCV infection.
To quantify the effect that deferral will have on disease outcome and on the public-health burden, we performed a modelling analysis using a Markov chain for liver-disease progression (validated and adopted in previous studies), based on actual epidemiological data from patients treated with DAAs in Italy and the United Kingdom (UK) (1). Both countries are on track to reach the WHO elimination goals, but have also witnessed an early and massive exposure to SARS-COV-2.
In the analysis, we considered a base scenario in which the standard of care is HCV treatment provided without interruption or restrictions, versus a scenario in which treatment is delayed (delays of 3, 6, 9, and 12 months). As the outcomes, we considered the number of incident cases of Advanced Liver Diseases (ALD) (i.e., decompensation, HCC, and the need for liver transplantation) and the number of HCV-related deaths for 1,000 standardized patients in a perspective view of 5 years, excluding the mortality by other causes according to official sources for Italy and the UK.
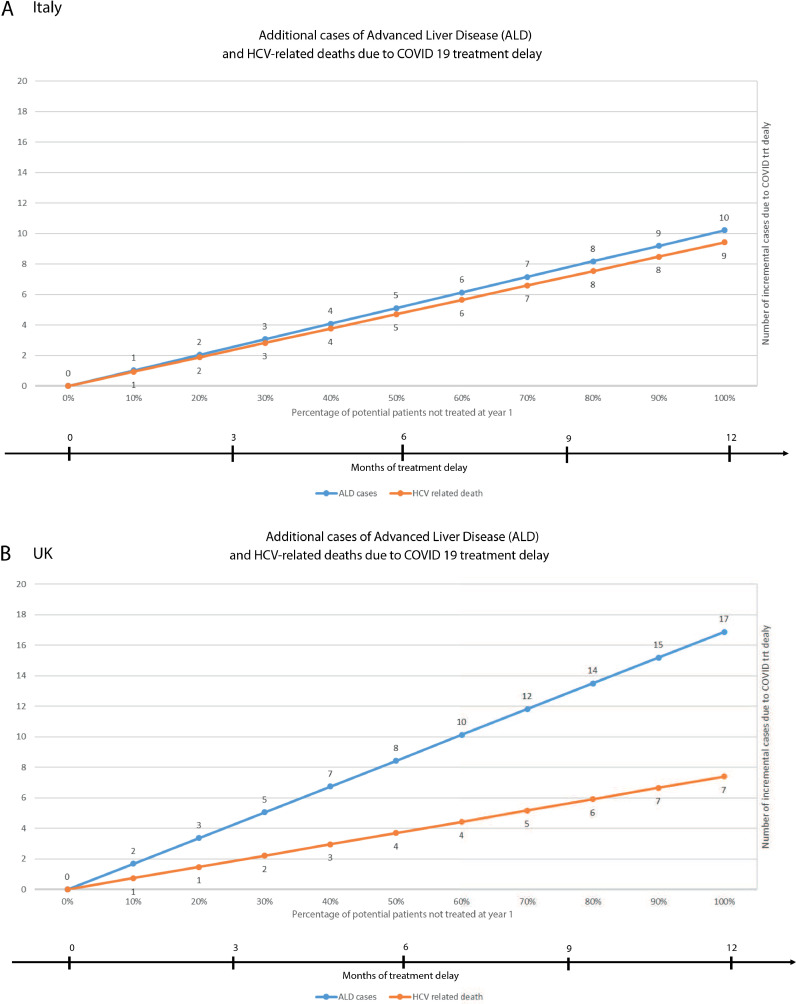
In the Fig. 1 , we illustrate the numbers of additional cases of ALD and HCV-related deaths attributed to delays in treatment of 3-12 months for 1,000 standardized patients taking into consideration distribution of the fibrosis stage in 2019. In both countries, there is a progressive increase in the number of cases and deaths for each delay. In Italy, for a delay of 3, 6, 9, and 12 months, we estimated an increase of 2, 5, 7, and 10 cases of ALD, respectively, and almost the same increase in the number of HCV-related deaths. For the UK, there was an increase of 3, 8, 12, and 17 cases of ALD and of 1, 4, 5, and 7 HCV-related deaths, respectively for 1,000 standartized patients. Despite the fact that there are great differences in the epidemiology of HCV infection between the two countries, with the UK having a significantly lower burden of infected cases, the delayed treatment scenario generates comparable outcomes, mostly because both countries have still a high proportion of patients with advanced fibrosis or cirrhosis (F3/F4 stages). Over time, the severe outcomes will be more evident for the UK, given that, compared to Italy, the infected population is younger and thus less affected by natural mortality and more likely to have a greater burden due to liver disease complications.
Fig. 1.
To better understand the actual impact of these standardized estimates, the disease burden should be considered. In Italy, in the past year, more than 7,000 treated patients had liver cirrhosis. Of those that are awaiting treatment and of those that are expected to be diagnosed through screening in the period 2020-2021, more than 100,000 patients are estimated to have advanced progressive liver disease (2). Hence deferring DAA treatment for an additional 6 months would, at 5 years, increase the number of HCV patients dying of a liver-related condition in Italy to over 500 patients, deaths totally avoidable by a not deferred test and treatment approach.
If we accept as unavoidable the need to decrease temporarily the efforts made toward HCV elimination due to the COVID-19 pandemic, we should at least preserve the availability of immediate treatment for patients with advanced fibrosis or cirrhosis. Although this could reduce severe disease outcomes, it would only be partially effective since: a) patients with less severe stages of fibrosis may proceed further, if delayed; and b) undiagnosed HCV patients with severe fibrosis would not be screened and treated in time. Based on our model, we suggest that, in all countries worldwide, whatever the residual burden of untreated HCV infection, when pursuing the exit strategy from strict lockdown measures for COVID-19, the prescription of DAAs should continue to be a high priority, in order to continue to follow the HCV elimination strategy and to reach the WHO goal.
Footnotes
On Behalf of all authors I declare none conflict of interest to be declared-
References
- 1.Marcellusi A, Viti R, Kondili LA, Rosato S, Vella S, Mennini FS. Economic consequences of investing in anti-HCV antiviral treatmentfrom the Italian NHS perspective: a real-world-based analysis of PITER data. Pharmacoeconomics. 2019;37:255–266. doi: 10.1007/s40273-018-0733-3. [DOI] [PubMed] [Google Scholar]
- 2.Kondili LA, Gamkrelidze I, Blach S. Optimization of hepatitis C virus screening strategies by birth cohort in Italy. Liver International. 2020 doi: 10.1111/liv.14408. (In press) https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]