Abstract
Purpose
Limited data exist regarding volumetric trends and management of upper-extremity emergencies during periods of social restriction and duress, such as the coronavirus disease 2019 pandemic. We sought to study the effect of shelter-in-place orders on emergent operative upper-extremity surgery.
Methods
All patients undergoing emergent and time-sensitive operations to the finger(s), hand, wrist, and forearm were tracked over an equal number of days before and after shelter-in-place orders at 2 geographically distinct Level I trauma centers. Surgical volume and resources, patient demographics, and injury patterns were compared before and after official shelter-in-place orders.
Results
A total of 58 patients underwent time-sensitive or emergent operations. Mean patient age was 42 years; mean injury severity score was 9 and median American Society of Anesthesiologist score was 2. There was a 40% increase in volume after shelter-in-place orders, averaging 1.4 cases/d. Indications for surgery included high-energy closed fracture (60%), traumatic nerve injury (19%), severe soft tissue infection (15%), and revascularization of the arm, hand, or digit(s) (15%). High-risk behavior, defined as lawlessness, assault, and high-speed auto accidents, was associated with a significantly greater proportion of operations after shelter-in-place orders (40% vs 12.5%; P < .05). Each institution dedicated an average of 3 inpatient beds and one intensive care unit–capable bed to upper-extremity care daily. Resources used included an average of 115 minutes of daily operating room time and 8 operating room staff or personnel per case.
Conclusions
Hand and upper-extremity operative volume increased after shelter-in-place orders at 2 major Level I trauma centers across the country, demanding considerable hospital resources. The rise in volume was associated with an increase in high-risk behavior.
Type of study/level of evidence
Therapeutic IV.
Key words: Coronavirus, COVID-19, Extremity trauma, Hand and upper-extremity emergencies, Replantation
First identified in December 2019, SARS-CoV-2 is a novel coronavirus responsible for coronavirus disease 2019 (COVID-19), a syndrome of variable severity that can lead to lung injury, organ failure, and death.1,2 Multiple factors, including easy transmission of the virus, severe symptomatology in certain individuals, and concern that hospitals may exceed capacity, led to national and state quarantine efforts.3 The response to the viral outbreak has generated economic hardship and a sharp rise in unemployment over a short period of several weeks.4,5 Trauma volume, along with rates of violence and suicide, can change based on economic conditions and temporal or seasonal patterns.6,7 However, the COVID-19 pandemic presents a unique mixture of social isolation, despair, economic hardship, and medical and psychologic pathology that has resulted in persisting upper-extremity injury and trauma.
Management of high-acuity upper-extremity traumatic injuries requires a functional trauma network and referral to tertiary centers that can provide readily available operating rooms, microsurgical techniques, inpatient beds, and an orthoplastic surgical approach.8 All of these resources have come under scrutiny during the COVID-19 pandemic.9 Thus, the American College of Surgeons (ACS) recommended that trauma centers maintain access for acute care services while canceling elective surgery.4,10 The disability of devastating hand and upper-extremity injuries is well-understood; delays in the management of fractures, major nerve injury, severe infection, and dysvascular extremity negatively affects patient outcomes.11, 12, 13 Thus, it is important to evaluate these potentially competing stressors on the health system critically during this unique public health crisis.
On March 19, 2020, California Governor Gavin Newsom issued an executive order declaring that all Californians should stay at home, and on March 23, Governor Tom Wolf of Pennsylvania followed suit for 7 counties including and surrounding Philadelphia.14,15 These declarations outlined social distancing practices intended to prevent and slow the spread of the virus. The authors at 2 geographically disparate Level I trauma centers observed persisting emergent upper-extremity injury despite orders to distance socially. As such, we hypothesized that several sociocultural drivers of upper-extremity injury were still present despite shelter-in-place orders. Here, we describe our findings from a series of patients who underwent emergent or urgent surgery of the upper extremity during the 24 days encompassing shelter-in-place orders.
Materials and Methods
All consecutive patients undergoing operative management of time-sensitive and emergency finger, hand, wrist, and forearm pathology by the combined Plastic and Orthopaedic Hand Surgery Services at the University of California, Irvine (UCI) and the University of Pennsylvania (UPenn) from March 11, 2020 to April 3, 2020 were included. The University of California, Irvine acts as Orange County’s tertiary referral center and only Level I trauma center, servicing 3.2 million residents. The University of Pennsylvania services Philadelphia County (1.5 million residents) and 7 surrounding counties in a metropolitan setting. This study did not include nonsurgical upper-extremity consultations and or procedures performed in the emergency department. Institutional review board approval was obtained at each institution.
The authors hypothesized that 5 sociocultural themes drove upper-extremity injury during this unique pandemic: (1) high-risk behavior, defined as lawlessness, assault, battery, robbery, and high-speed automobile accidents; (2) the presence of suicidal ideation or suicide attempt; (3) a lack of usual resources such as home help, meal assistance, or handypersons owing to social distancing ascertained by patient or family history; (4) participation in new home activities or building projects; and (5) avoidance of health care and delay in care for fear of contracting the virus. The presenting diagnosis for each patient was categorized thematically by social changes related to the COVID-19 pandemic if any of the following 5 parameters were met. Change in frequency of these sociocultural drivers were compared before and after shelter-in-place orders.
Descriptive information and related imaging were collected from medical records and reviewed retrospectively. Demographic data regarding surgical date, age of the patient, injury severity score (ISS), American Society of Anesthesiologist (ASA) physical status classification, diagnosis, and procedures were collected. Hospital and operating room resources were tracked, including the use of hospital masks, gowns, gloves, hospital, and intensive care unit (ICU) beds. Institutional and temporal differences between operative volume and patient and surgical details before and after shelter-in-place orders were analyzed using descriptive statistics, univariate analysis, and paired t tests, where appropriate. Operative and postoperative complications were noted until the conclusion of the study period on April 3, 2020.
Results
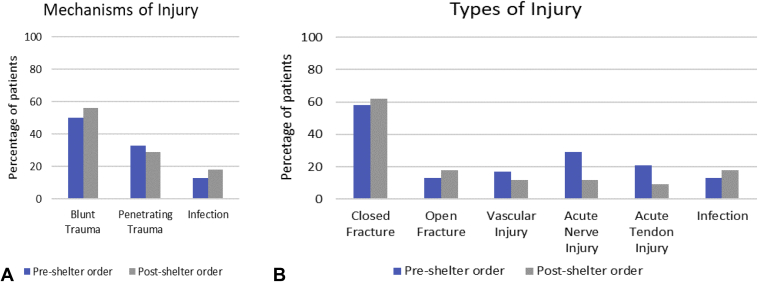
A total of 58 patients underwent emergency operations to the finger(s), hand, wrist, and forearm during the 24-day study period before and after the shelter-in-place order at each institution (Table 1). Twenty-four operations occurred before shelter-in-place orders whereas 34 (59%) occurred after shelter-in-place orders. Average patient age was 42 years (range, 18–85 years); most were men (69%). Forty-nine patients (84%) presented after trauma with an average ISS of 9 (range, 1–59). Blunt trauma was more common than penetrating trauma both before and after shelter-in-place orders (Fig. 1A). Nine patients (15%) presented with nontraumatic pathology, including severe soft tissue infection and osteomyelitis. High-energy fractures were the most common indication for surgery (35 of 58; 60%). Nerve injuries, including sharp lacerations of the radial (n = 1), ulnar (n = 2), and digital nerves (n = 9), were the second most common indication for surgery (21%). Nine patients (15%) underwent revascularization of the arm, hand, or digit, or digital replantation. Figure 1B demonstrates the types of injury before and after the shelter-in-place orders.
Table 1.
Patient Demographic Characteristics, Operative Features, Resources, and Relationships to COVID-19 Comparing Before and After Shelter-in-Place Orders
| Demographic Characteristics | Total (n = 58) | Before Shelter (n = 24) (41%) | After Shelter (n = 34) (58%) | P Value |
|---|---|---|---|---|
| Age average, y (range) | 42.7 (18–85) | 42 (18–84) | 42 (21–85) | .47 |
| Male sex (%) | 40 (69) | 17 (70) | 23 (67) | .79 |
| ISS average (range) | 9.6 (1–59) | 8.8 (1–48) | 10.2 (1–59) | .35 |
| Penetrating trauma, n (%) | 18 (31) | 10 (42) | 8 (23) | .19 |
| Blunt trauma, (%) | 31 (53) | 12 (50) | 19 (56) | .66 |
| ASA score mode (range) | 1 (1–5) | 1 (1–5) | 2 (1–5) | .30 |
| Operative variables | ||||
| Average procedures per d | 1.2 | 1.04 | 1.4 | .91 |
| Operating time average, min (range) | 115 (11–416) | 128 (11–416) | 103 (24–365) | <.05 |
| General anesthetic, n (%) | 30 (52) | 10 (42) | 20 (59) | .2 |
| Monitored anesthesia care, n (%) | 23 (39) | 10 (42) | 13 (38) | .38 |
| Regional anesthesia only, n (%) | 5 (8.6) | 4 (17) | 1 (3) | .18 |
| Resource use | ||||
| Personnel per procedure average, n (range) | 8.3 (3–15) | 9 (6–15) | 8 (3–14) | .5 |
| Masks used, total average, n (range) | 8.3 (3–15) | 9 (6–15) | 8 (3–14) | .5 |
| Gowns used, total average, n (range) | 4.7 (2–10) | 5 (3–10) | 4. (2–10) | .33 |
| Gloves used total average, n (range) | 7.6 (2–20) | 8.1 (4–14) | 7 (2–20) | .15 |
| Blood products used, total average, units | 17 | 6 | 11 | |
| Inpatient days average, n (range) | 2.25 (0–10) | 2.2 (0–10) | 2.3 (0–8) | .45 |
| ICU days total, patients/d average (range) | 21 (0.87) | 8 (0.33) | 13 (0.38) | .44 |
| Diagnosis related to COVID-19, n (%) | 35 (60) | 9 (37.5) | 26 (76) | Odds ratio = 4.6 <.01 |
| Suicide attempt, n (%) | 2 (3.4) | 2 (8) | 0 | |
| Home quarantine building project, n (%) | 4 (7) | 2 (8) | 2 (6) | .71 |
| Lack of social support or distancing, n (%) | 2 (3.4) | 0 | 2 (6) | |
| High-risk behavior, n (%) | 19 (33) | 3 (12.5) | 16 (47) | Odds ratio = 5 .001 |
| Health care avoidance related to COVID, n (%) | 8 (12) | 2 (8) | 6 (18) | .32 |
Figure 1.
A Mechanisms of upper-extremity injury before and after shelter-in-place orders. B Injury types before and after shelter-in-place orders.
Patients were analyzed separately based on institution to identify differences in practice patterns and patient population. Patients at UCI had higher average ISS (12 vs 7; P = .05) and general anesthetic use (77% vs 33%; P < .05), as opposed to monitored anesthesia care or regional, compared with UPenn. Otherwise, patient and care data were similar between institutions.
Shelter-in-place effect
High-risk behavior, leading to upper-extremity injury and emergent or urgent operative intervention, increased after shelter-in-place orders (12.5% before vs 47% after; P = .001). Similarly, an increase in urgent or emergent surgical volume by 40% was observed, an increase in daily case average from 1 to 1.4. Mechanism of injury, rate of penetrating trauma, diagnosis, and type of surgery were similar. Health care avoidance rose by 10% after shelter-in-place orders (P > .05).
Resource use
Given the 40% increase in operative cases after shelter-in-place orders, the total sum of resources used increased correspondingly. However, there was no notable change in the quantity of resources used per case before and after shelter-in-place orders besides a drop in operating room time. On average, resource use per case included an average daily use of 115 minutes of operating room time, 122 minutes of intraoperative mechanical ventilator use, 8 surgical masks, 5 sterile gowns, and 8 pairs of sterile gloves, along with a variety of usual equipment needs including instrumentation, hardware, operative microscope, and fluoroscopy. The surgical team consisted of an average of 8 medical staff/case (range, 3–15), including operating room nurses, technicians, anesthesia staff, and surgeons. Fifty-seven percent of patients were hospitalized for 1 to 10 days (average of 2.2 days length of stay). In addition, 21 total ICU days were required during the 12 days before and after the shelter-in-place order including at least one ICU bed that was used 70% of the time at UCI and 31% at UPenn, respectively.
Seventeen units of blood product, including 12 packed red cells, were transfused in this series. Fifteen units of blood were used for severely traumatized individuals independent of the extremity trauma. Two units were used after a replanted digit developed venous congestion requiring heparinization and leech therapy. The congested digit was successfully salvaged. This marked the only complication in the group. There were no other acute postsurgical infections, thrombotic events, or systemic complications.
Coronavirus disease 2019 themes
Although no patient in this study exhibited symptoms of COVID-19 or had positive test results, 60% of the study population (n = 35) met 1 of 5 themes related to the COVID-19 pandemic: (1) high-risk behavior and lawlessness, (2) suicidality, (3) lack of usual social and physical resources, (4) home improvement projects, and (5) avoidance of health care facilities. There was a significant increase in injuries categorized within these 5 themes after shelter-in-place orders (37.5% before vs 76% after; P < .01) (Table 1). Figure 2 summarizes the 24-day event time line, including the respective shelter-in-place order dates, and demonstrates volumetric changes in cumulative operations. Figure 3 shows the proportion of patients demonstrating the 5 themes relative to the stay-at-home orders. High-risk behavior, including multiple stabbings, gunshot injuries, high-speed auto accidents, attempted escape from police custody, and assaults, increased nearly 4-fold (P = .001). Two suicide attempts occurred, in which one patient did not have a clear, antecedent psychiatric diagnosis and wished to end life for fear of “spreading the virus” (Fig. 4). Four patients (7%) engaged in home-improvement activity, resulting in 2 mutilating table-saw incidents (Fig. 5). Two patients (3.5%) lacked usual social support after the shelter-in-place order, leading to falls and wrist fractures while at home alone. This included an open wrist fracture in an otherwise healthy woman lacking a usual handyperson and a severely deformed, closed, both-bone forearm fracture in an 85-year-old woman whose caregiver was avoiding contact with her. Eight patients (12%; 2 before vs 6 after) had delayed presentations owing to health care avoidance, including one scenario of a digital amputation for a severe necrotizing infection (Fig. 6).
Figure 2.
Time line of pandemic events, cumulative operative volumes, and proportion of cases related to 5 unique pandemic-associated themes. WHO, World Health Organization.
Figure 3.
Proportion of patients demonstrating (1) high-risk behavior, (2) suicidality, (3) lack of social and physical support, (4) participation in home improvement projects, and (5) avoidance of health care or delay in seeking treatment before and after shelter-in-place orders versus patients without COVID-19–related interventions.
Figure 4.
A 27-year-old man with underlying bipolar disorder attempted suicide with a hand saw to the left neck and hand. A Dysvascular index and middle fingers requiring repair of the B ulnar digital arteries, and C multiple nail bed, tuft, nerve and zone II flexor tendon injuries requiring repair to restore a normal cascade.
Figure 5.
A 69-year-old woodworker experienced a righthanded table saw injury to multiple digits requiring revascularization of the index and middle fingers with A poor turgor and color and B later improvement (Pre). C Final intraoperative tenodesis showing restoration of the cascade. This patient began active motion on postoperative day 5 (Post).
Figure 6.
A 39-year-old man avoided health care facilities for 10 days for fear of contracting coronavirus. A Intraoperative findings demonstrated tissue necrosis and erosion of the flexor sheath. B Sheath irrigation with a pediatric feeding tube. C Primary amputation was performed at the proximal interphalangeal joint. The patient went on to heal without difficulty after a 14-day course of oral antibiotics.
Discussion
A steady volume of high-acuity hand and upper-extremity pathology continued to present to both Level I trauma centers despite governmental orders for persons to self-quarantine, practice social distancing, and shelter in place. Unlike some cities and places in the United States overwhelmed by treating COVID-19 patients, surgeons at both medical centers had resources necessary to treat the increased surgical volume of traumatic hand care. Accordingly, we identified 5 concerning societal themes during the COVID-19 pandemic and shelter-in-place orders: (1) high-risk behavior and lawlessness, (2) suicidality related to the virus, (3) lack of usual social and physical support owing to distancing, (4) home improvement and woodworking projects, and (5) avoidance of health care facilities causing delay in care and treatment.
Hand and upper-extremity injuries have historically represented 12% of all traumatic injuries in the United States that present to emergency rooms.16 From 2009 to 2012, this equated to 34 billion emergency room visits nationally for hand injuries.17 Moreover, hand injuries follow temporal patterns, with a rise and fall in volume from April through October, peaking around early July.17 This temporal pattern is followed in step by overall trauma admissions in the United States, with peaks associated with warmer temperatures and summer months.18 Although hand injury can act as a model for societal trends and trauma volume, the increased number of operative hand cases observed in our series seemed to follow, if not exceed, historical norms unique to the COVID-19 pandemic and related societal interventions. Further study involving a longer time frame and exacting comparison between operations during the COVID-19 pandemic versus historical rates at each institution is required to delineate further COVID-19’s effect on patient volume. It would appear that governmental restrictions geared toward slowing viral spread seems to have increased high-risk activity among a subset of patients presenting with operative hand trauma, uncoupling operative hand trauma from trauma volume at large. This rise in operative extremity surgery cannot be generalized toward the overall volume of crime in a community that, on the whole, has dropped nationally and regionally.19
Cross-sectional population studies have demonstrated increased psychological distress, depression, and suicide after economic recession.6 In addition to our identification of 2 suicide attempts in this series, one published case report presented a suicide directly attributed to a fear of COVID-19.20 However, to the authors' knowledge, there are no published reports regarding general or upper-extremity trauma volumes in other times of great social stress within America, such as after Hurricane Katrina and 9/11. Social isolation, new unemployment, and financial and emotional despair can contribute to a rise in trauma volume during a pandemic and warrant further investigation.
Although unable to work or engage with the community, people may engage in behaviors or activity at home which they may not ordinarily do. Isolated elderly patients may be unable to rely on others for daily tasks, leading to increased injury. The most frequent cause of hand injury in patients greater than age 65 years is a fall caused by tripping, stumbling, or slipping.21 With imposed shelter-in-place orders and less available assistance, it is likely that elderly people are at increased risk for traumatic injury during the pandemic.
Fear of disease and diagnosis is well-documented, with reports in the literature of fear-based delays in care for colorectal disease, cancer, and asthma.22, 23, 24 Although there are no published data regarding delay in seeking treatment for upper-extremity injury, many patients do not prioritize hand care, waiting days to weeks before addressing infections or fractures. With this amount of time, a hand infection can quickly progress to involve bone or proximal structures and necessitate wide debridement or amputation for an initially trivial injury. We hypothesize that the widespread fear and panic induced by the COVID-19 pandemic exacerbated delays in medical attention in several patients in our series.25
Management of severe upper-extremity injuries requires substantial hospital resources that have come under considerable scrutiny, such as masks, gowns, gloves, hospital beds, and ventilators.9 Both academic centers adhered to the ACS Statement on March 20, 2020 with regard to maintenance of the trauma network and consistent trauma care.10 During each 24-day period, nearly 2 hours of dedicated operating room and ventilator time were used per institution per day at each institution. Operating room time decreased by a half hour after shelter-in-place orders, but it is unclear whether this resulted from a variation in case mix and or a conscious decision on the surgeon’s part to speed the operation. Further study in this area is required. The cancellation of all elective surgery, recommended by the ACS on March 13, 2020, and the Centers for Medicare and Medicaid Services on March 18, 2020, assisted in freeing operating rooms and equipment for these emergent cases. There was no delay in treatment owing to the lack of resources.4,26 Our operative volume was also affected by adjusted practice patterns during this period. At UCI, 14 patients with closed fractures meeting operative indications presented to the emergency department and were surgically corrected during the same hospital stay, because it was believed that additional clinic visits to arrange elective fracture care at an outside surgery center would have increased the number of health care visits and overall exposure to staff. In addition, allowing fractures to go on to nonunion or malunion would only delay a potentially inevitable course of treatment and increase the number of future interventions. Accordingly, this led to the use of hospital beds, ICU beds, operating rooms, and up to 15 staff/d to manage injuries to the hand and upper extremity. This presents a considerable ethical controversy in the face of limited resources during the current and future pandemics.
The risks for aerosolization of coronavirus during intubation and increased use of protective personal equipment have prompted the ASA to make several recommendations based on experiences from China and Canada.27 We attempted to maximize the use of regional blockade and monitored anesthesia care without intubation whenever possible. However, most patients were ultimately intubated in this series owing to an inability to manage and treat severely traumatized patients with multisystem injury safely without airway control. At the time of the study, preoperative COVID-19 testing was not in wide use. We screened each patient clinically, and the importance cannot be overstated given recent reports from Wuhan showing a 40% mortality rate among orthopedic fracture patients who had COVID-19 concurrently.28
Limitations of this study include the short duration of observation, small patient numbers, inherent institutional differences, and insufficient statistical power. The limited design of the study does not allow for comparison with a dataset outside the pandemic period. Thus, we cannot be certain that trends are directly related to the shelter-in-place effect. Rather, they may reflect broader changes due to the COVID-19 pandemic or fluctuations in baseline seasonal trauma patterns. Also, few published datasets are available for historical comparison that are specific to operative hand trauma. This series is a reflection of a unique practice environment of metropolitan Level I academic trauma centers. Colleagues in different practice settings or supporting different patient populations may not experience identical effects.
Conclusion
In the setting of shelter-in-place orders and social distancing, this study demonstrates a persistent volume of upper-extremity trauma requiring hospital care and resource use under growing scrutiny in the current economy. We described 5 sociocultural themes during the COVID-19 pandemic outside usual temporal or institutional trauma patterns that could account for the volume of upper-extremity injury: (1) high-risk behavior and lawlessness; (2) suicidality; (3) lack of usual social and physical resources; (4) home improvement projects; and (5) avoidance of health care facilities, leading to a delay in treatment. Despite limitations in access to nonessential activities during the current COVID-19 pandemic, we find that patients continue to experience major hand injury and infections that require urgent care. It is important for hospitals and health systems to maintain unrestricted patient access to emergency hand surgical care and provide the full scope of services.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received by the authors related directly or indirectly to the subject of this article.
References
- 1.Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections–more than just the common cold [published online ahead of print January 23, 2020]. JAMA. https://doi.org/10.1001/jama.2020.0757 [DOI] [PubMed]
- 2.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The White House. 15 days to slow the spread. Available at: https://www.whitehouse.gov/articles/15-days-slow-spread/. March 16, 2020. Accessed June 1, 2020.
- 4.American College of Surgeons COVID-19: Recommendations for management of elective surgical procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at:
- 5.American Society of Plastic Surgeons ASPS statement on breast reconstruction in the face of COVID-19 pandemic. https://www.plasticsurgery.org/documents/medical-professionals/COVID19-Breast-Reconstruction-Statement.pdf Available at:
- 6.Silva M., Resurrección D.M., Antunes A., Frasquilho D., Cardoso G. Impact of economic crises on mental health care: a systematic review. Epidemiol Psychiatr Sci. 2018;29:e7. doi: 10.1017/S2045796018000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cinat M.E., Wilson S.E., Lush S., Atkins C. Significant correlation of trauma epidemiology with the economic conditions of a community. Arch Surg. 2004;139(12):1350–1355. doi: 10.1001/archsurg.139.12.1350. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal P., Vaishya R. Orthoplastic surgery: need of the hour. J Clin Orthop Trauma. 2019;10(5):837–838. doi: 10.1016/j.jcot.2019.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages—The need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 10.American College of Surgeons Maintaining trauma center access & care during the COVID-19 pandemic: guidance document for trauma medical directors. https://www.facs.org/quality-programs/trauma/maintaining-access Available at:
- 11.Giladi A.M., McGlinn E.P., Shauver M.J., Voice T.P., Chung K.C. Measuring outcomes and determining long-term disability after revision amputation for treatment of traumatic finger and thumb amputation injuries. Plast Reconstr Surg. 2014;134(5):746e–755e. doi: 10.1097/PRS.0000000000000591. [DOI] [PubMed] [Google Scholar]
- 12.Giladi A.M., Ranganathan K., Chung K.C. Measuring functional and patient-reported outcomes after treatment of mutilating hand injuries: a global health approach. Hand Clin. 2016;32(4):465–475. doi: 10.1016/j.hcl.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoon A.P., Kaur S., Chou C.H., et al. Reliability and validity of upper extremity patient-reported outcome measures in assessing traumatic finger amputation management. Plast Reconstr Surg. 2020;145(1):94e–105e. doi: 10.1097/PRS.0000000000006326. [DOI] [PubMed] [Google Scholar]
- 14.Calif Exec Order N-33-20 (2020).
- 15.Governor Wolf and health secretary issue “stay at home” orders to 7 counties to mitigate spread of COVID-19. https://www.governor.pa.gov/newsroom/governor-wolf-and-health-secretary-issue-stay-at-home-orders-to-7-counties-to-mitigate-spread-of-covid-19/ Available at:
- 16.Maroukis B.L., Chung K.C., MacEachern M., Mahmoudi E. Hand trauma care in the United States: a literature review. Plast Reconstr Surg. 2016;137(1):100e–111e. doi: 10.1097/PRS.0000000000001879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colen D.L., Fox J.P., Chang B., Lin I.C. Burden of hand maladies in US emergency departments. Hand (N Y) 2018;13(2):228–236. doi: 10.1177/1558944717695749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stonko D.P., Dennis B.M., Callcut R.A., et al. Identifying temporal patterns in trauma admissions: Informing resource allocation. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0207766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Public Policy Institute of California COVID-19 and crime in major California cities. https://www.ppic.org/blog/covid-19-and-crime-in-major-california-cities/ Available at: April 7, 2020. Accessed June 1, 2020.
- 20.Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: first suicidal case in India! Asian J Psychiatr. 2020;49:101989. doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kringstad O., Dahlin L.B., Rosberg H.E. Hand injuries in an older population–a retrospective cohort study from a single hand surgery centre. BMC Musculoskelet Disord. 2019;20(1):245. doi: 10.1186/s12891-019-2617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds L.M., Bissett I.P., Consedine N.S. Emotional predictors of bowel screening: the avoidance-promoting role of fear, embarrassment, and disgust. BMC Cancer. 2018;18(1):518. doi: 10.1186/s12885-018-4423-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nonzee N.J., Ragas D.M., Ha Luu T., et al. Delays in cancer care among low-income minorities despite access. J Womens Health (Larchmt) 2015;24(6):506–514. doi: 10.1089/jwh.2014.4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Janson S., Becker G. Reasons for delay in seeking treatment for acute asthma: the patient's perspective. J Asthma. 1998;35(5):427–435. doi: 10.3109/02770909809048951. [DOI] [PubMed] [Google Scholar]
- 25.Depoux A., Martin S., Karafillakis E., Bsd R.P., Wilder-Smith A., Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. 2020;27(3):taaa031. doi: 10.1093/jtm/taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ambulatory Surgery Center Association Statement from the Ambulatory Surgery Center Association regarding elective surgery and COVID19. https://www.ascassociation.org/asca/resourcecenter/latestnewsresourcecenter/covid-19/covid-19-statement Available at: Published March 16, 2020. Accessed June 1, 2020.
- 27.Lie S.A., Wong S.W., Wong L.T., Wong T.G.L., Chong S.Y. Practical considerations for performing regional anesthesia: lessons learned from the COVID-19 pandemic [published online ahead of print March 24, 2020]. Can J Anaesth. https://doi.org/10.1007/s12630-020-01637-0 [DOI] [PMC free article] [PubMed]
- 28.Mi B., Chen L., Xiong Y., Xue H., Zhou W., Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients [published online ahead of print April 1 2020]. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.20.00390 [DOI] [PMC free article] [PubMed]