Since late last year, Asia has faced the mounting challenge of the coronavirus disease 2019 (COVID-19) pandemic. The first cases were reported in China in late 2019, whereas Singapore saw their first imported case in late January 2020. Over the last few months, we have experienced many challenges in the clinical management of patients with glaucoma. In this commentary, we provide perspectives from China and Singapore on how glaucoma practice has adapted during this crisis.
Perspectives from Guangzhou, China
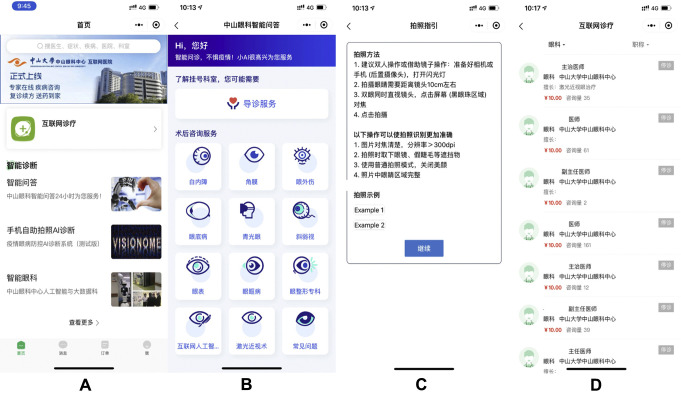
First, the pandemic made it difficult for patients to access medical care. To address this, we designed a chatbot program on the widely used WeChat app (Fig 1 ). Patients were asked a series of questions and responded by pressing the appropriate button on their phones. They also were encouraged to take photographs of their eyes and upload these to the program. The data were analyzed by either an artificial intelligence program or by doctors, depending on the information provided by the patient. A provisional diagnosis and management plan then were made and conveyed to the patient via the app. If medications were required, they were prescribed via the app. In terms of data privacy and security, this system uses the inbuilt WeChat cyber security microprogram that complies with the requirements of the Network Security Law and Personal Information Protection Act of China. The patients’ clinical data are accessible only by designated doctors who are granted access, and each login attempt is tracked by the security system. In a users’ survey, more than 90% of the 1500 patients so far enrolled in this project were satisfied with this service.
Figure 1.
Illustrations of the WeChat app used in Guangzhou, China. (A) Homepage of the Wechat microprogram; (B) displays the clinics available of different subspecialties; (C) instructions on how to take and upload the photo onto the AI system; (D) list of clinicians available for online consultation.
We also recognized early on the need to reduce drastically the number of patients attending clinics and operating theaters. By stratifying according to clinical need, nonurgent clinic cases were deferred, reducing clinics to one quarter of the usual load. Only patients who were deemed to be at high risk of permanent visual morbidity should their surgery be delayed underwent operations. All patients underwent a nasal swab and serologic analysis in the week before surgery to test for COVID-19 infection. After surgery, the operating theater was cleaned with chlorinated agents, with at least a 30-minute gap between cases.
Since the beginning of the pandemic, several ophthalmologists have become infected, and 3 died in Wuhan because of the lack of adequate protection. As soon as health authorities determined the transmission routes of COVID-19, we undertook a series of measures including mandating that all staff use eye goggles and surgical masks, installing plastic shields (made from old radiographic films) on slit lamps between the patient and the examining ophthalmologist, as well as changing gloves and sterilizing slit lamps before each patient encounter. Intraocular pressure was checked with noncontact tonometers, which were sterilized with alcohol wipes before use for each patient. Gonioscopes were soaked in 75% alcohol for half an hour before reuse.
Perspectives from Singapore
Early on in this crisis, we recognized 3 principles that needed to be followed. These were to protect staff and patients from acquiring and spreading infection, to ensure that adequate manpower was available to mitigate against staff illness (or home quarantine), and to reduce any significant ocular morbidity resulting from the deferral of appointments and treatment.
As in China, we implemented several changes to address these principles, such as the installation of plastic shields on slit lamps, mandatory use of face masks, as well as twice-daily temperature monitoring of all healthcare personnel. We segregated staff into 2 teams with designated rest areas for each, and no contact was allowed between teams. Finally, we deferred outpatient appointments for nonurgent cases to decongest clinics, with the length of deferral determined by doctors on review of the patients’ electronic health records. This reduced clinic numbers by approximately 50% to 80%. However, we have encountered many challenges in implementing the above changes. For example, identifying patients suitable for deferral of follow-up visits has been laborious, requiring the prospective categorization of patients into mild, moderate, or severe disease to decide who might be safe for deferral or video consultation.
In the next few weeks, we will be sending patients to new investigation units in the community for visual acuity assessment, intraocular pressure measurement, visual field testing, and anterior and posterior segment photography. These investigation units in the community are stand-alone units located in the community and staffed by technicians. A video consultation will be conducted 1 week after the investigations, with data reviewed by the physician and compared with data from the patient’s electronic health record. Any medications required will be delivered to the patient by courier. Patients whose condition is identified as worsening can have their medications modified or can be brought back to the clinic for further assessment.
What We Learned from the Crisis That Could Help Glaucoma Services in the Future
Through this crisis, we crucially have learned that the 2 methods of online and offline medical care cannot replace each other. Instead, a combination is necessary to manage patients with glaucoma optimally while saving medical resources. Patients should have the primary consultation first online, and only those requiring further assessment or surgical procedures should come to the hospital for in-person management. If systems can be designed such that investigations can be performed in the community without the need for human involvement (e.g., with the use of automated devices), then the model of investigation units in the community and asynchronous video consultation can help reduce COVID-19 spread further while also maintaining quality of care.
In conclusion, to reduce the risk of COVID-19 infection, changes have to be implemented as to how patients with glaucoma are managed. Apart from the improved segregation of patients and staff, as well as physical and chemical barriers to infection in clinics, novel initiatives such as increasing investigations in the community, coupled with the use of virtual consultations, will help minimize ocular morbidity from delayed care. The use of new digital technologies such as smartphone-based apps and artificial intelligence represent a further avenue to transform glaucoma management.
Footnotes
Financial Disclosure(s): The author(s) have no proprietary or commercial interest in any materials discussed in this article.