Abstract
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has now widely spread globally. The main transmission routes of SARS-CoV-2 comprise human-to-human droplet infection, including inhalation and contact infection of patient's saliva, blood and other body fluids through oral mucosa, nasal mucosa, and the eyes, and orofecal transmission. Dental treatment necessitates close-proximity, face-to-face practices and can generate droplets or aerosols containing water, saliva, blood, microorganisms, and other debris during the procedure. Therefore, dental professionals are at a high risk of SARS-CoV-2 infection. To prevent nosocomial SARS-CoV-2 spread during dental procedures, Taipei City Hospital established a dental patient triage and workflow algorithm for the provision of dental services during the COVID-19 pandemic. Given the highly contagious nature of SARS-CoV-2, it is imperative to institute an appropriate standard procedural policy for patient management and recommendation of dental treatment at hospitals during the COVID-19 pandemic.
Keywords: COVID-19, Dental care, Dental triage flowchart, Infection-control, Nosocormial infection
Introduction
Coronavirus disease 2019 (COVID-19) induces a severe, atypical, infectious pneumonia and has spread rapidly from Wuhan City, China.1 Between December 2019 and May 5, 2020, there have been more than 3.6 million confirmed cases of COVID-19 and over 257,239 deaths. Worldwide, more than 187 countries are battling the COVID-19 outbreak and are affected by this highly infectious disease. On January 30, 2020, the World Health Organization (WHO) declared this global pneumonia outbreak as the 6th Public Health Emergency of International Concern of the past decade and on March 11, 2020, the outbreak status was upgraded from epidemic to pandemic by the WHO.
To face this rapidly emerging infectious disease, we reviewed the literature about the newly emerged virus and provided a standard operating procedure, dental health facilities to combat and prevent further global spread of the pandemic.
The global impact and comparison of three major diseases caused by coronaviruses
Seven coronaviruses are known to cause human disease and in particular three highly pathogenic coronaviruses strains caused severe acute respiratory syndrome (SARS), Middle East Respiratory Syndrome (MERS) and COVID-19, generate more serious outcomes.2
In 2003, SARS outbreak resulted in 8,096 confirmed cases and 774 deaths over 29 countries and regions; the overall case-fatality rate (CFR) was 10%. In Taiwan, of the 668 confirmed cases, 181 (27.1%) patients including 17 healthcare providers succumbed to the disease. The basic reproduction number (R0) is the average number of secondary cases caused by a single infective individual when there is a lack of widespread immunity. The R0 of SARS was approximately 3.3
The MERS outbreak affected 26 countries from Saudi Arabia in June 2012, with 2,494 confirmed cases and 858 deaths reported so far. However the CFR was 34.4% and the R0 was estimated between 2 and 5 during the outbreak phase.4
COVID-19 caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has an average incubation period of 5.2 days; however, some studies had shown longer incubation periods of up to 14 days. The R0 was reported to be 1.4–2.5 by the WHO on January 18, 2020, and other studies have estimated the R0 to be between 1.5 and 3.5.3
The WHO reported that the overall CFR of COVID-19, as of March 3, was 3.4%, and it increased to 7.02% on May 5, 2020. This value varies considerably among different countries and regions depending on the level of the outbreak, rate of infection, and availability of medical facilities. Until May 5, 2020, the CFR of COVID-19 was 1.4% (6 deaths/438 confirmed cases) in Taiwan.
The transmission routes and high contagious periods of SARS-CoV-2
The transmission routes of SARS-CoV-2 include: direct transmission through inhaled droplets, from patient's cough or sneeze; contact with an infected patient's saliva, blood and other body fluids through the oral mucosa, nasal and ocular membranes; and orofecal contact.5 Based on the infection carrier and origin, transmission could be classified into three types.
1. Symptomatic transmission: This involves transmission through direct contact with a symptomatic individual. On average, it takes 2–14 days after exposure for symptoms to develop. The common symptoms include fever, coughing, fatigue, sputum, dyspnea, myalgia, anorexia, sore throat, stuffy nose, wheezing, headache, and diarrhea et al.1,2 During symptom onset, higher viral loads were detected in patients, especially in the nasal cavity than in the pharynx.6
2. Pre-symptomatic or asymptomatic transmission: Some studies have reported COVID-19 patients with mild flu-like symptoms or those who may be even asymptomatic.7 According to a study published in Nature,8 viral loads in the SARS-CoV-2 patient can be detected as early as the onset of atypical or very mild symptoms. The viral loads in the initial 5 days reached peak concentrations that were a 1000-fold higher than that of the SARS-CoV during the same period. The transmission rate of SARS-CoV-2 is enhanced because of transmission from pre-symptomatic and asymptomatic carriers.9
3. Environmental transmission: Evidence from studies have shown that SARS-CoV-2 can survive in aerosols for up to 3 hours and is capable of surviving for up to 4 and 24 hours on copper and cardboard, respectively. Furthermore, the virus can survive on plastic and stainless-steel surfaces for approximately 48 and 72 hours, respectively.5 SARS-CoV-2 is stable on contaminated surfaces and in aerosols,10 the risk of nosocomial transmission is high.
Healthcare providers face a high occupational risk of SARS-CoV-2 infection and standardized procedural policies for patient management on hospital arrival are imperative for risk mitigation during the COVID-19 pandemic.
Dental patient triage and workflow during the COVID-19 pandemic in the hospital
COVID-19 poses a higher risk for dental practitioners, as many routine dental interventions involve aerosol-generating procedures. Dentists come into contact with the saliva and blood of patients and also inhale airborne particles and aerosols produced during dental procedures as well as patient exhalation. The Taiwan CDC care guidelines and standards for dental care during the pandemic recommend the use of Level 3 PPE, including medical standard N95 face masks, disposable waterproof gowns, goggles, and face shields for dental personnel.
At present, there are no large-scale community infections in Taiwan. Approximately 86% of confirmed cases were imported carriers. In patients with suspected COVID-19 infection, emergent dental conditions can be treated while ensuring complete personal protection of dental practitioners.
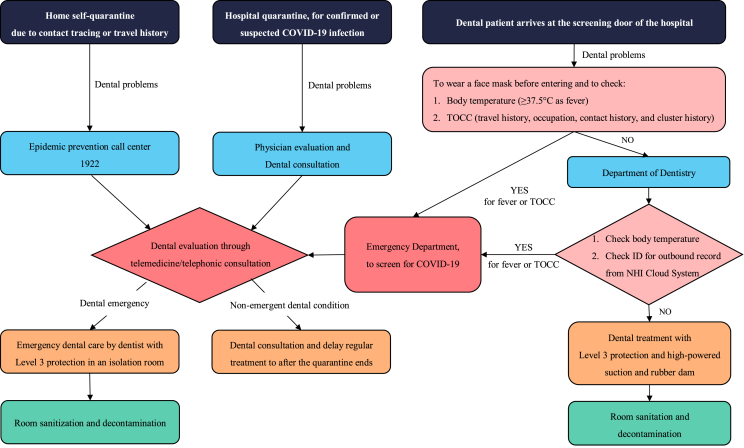
The Taipei City Hospital is a 4,700-bed regional healthcare organization with 7 branches that provides access to health services for all citizens of Taipei City. In 2003, SARS epidemic severely affected Taiwan's healthcare system and led to a lockdown at Heping Hospital, a branch of Taipei City Hospital. The outbreak resulted in 35 deaths at the time. Based on their previous SARS experience, Taipei City Hospital established a standard operating procedure for dental treatment to contain nosocomial COVID-19 transmission at the beginning of the COVID-19 pandemic in February 2020 (Fig. 1).
Figure 1.
Standard operating procedure for dental treatment during the COVID-19 pandemic in Taipei City Hospital.
When a patient arrives at the screening door of the hospital, strict rules are to be enforced and complied with. Everyone is required to wear a face mask, the body temperature is recorded, (≧37.5 °C marked as fever), and history of travel, occupation, contact, and cluster (TOCC) is ascertained. Patients with fever and TOCC are directly escorted to the emergency department (ED) through a special passage. We regard the temperature higher than 37.5 °C as fever, the guideline is as the same as of that in Japan and Korea compared to 38 °C in Hong Kong and 100 °F (=37.78 °C) in the guideline of ADA. The relative TOCC records are also collected in the above countries. A visitor with the travel history of COVID-19 outbreaking area during the last 3 weeks is not allowed to enter hospital access of the Asan Medical Center in Seoul, Korea.
If a dental patient has no fever or TOCC concerns, they proceed to the Department of Dentistry and undergo a second screening. The patient's outbound record is checked via the Taiwan National Health Insurance Cloud System before treatment performed. The dental treatment is undertaken with a focus on minimizing aerosol-generating practices by decreasing the usage of the rotary and high-speed handheld devices, together with high-powered suction, rubber dam application, and hand curettage instead of ultrasonic cleaning. Scheduling of patient appointments during this period is limited and the next patient enters the clinic only after the previous patient has left the room and all room decontamination procedures have been completed. Each dental treatment space is separated by high wall coverage to limit the possibility of cross-contamination by aerosols in the environment and the clinic isolation room has a single dental chair only.
In the ED, a physician initially evaluates the patient with fever or positive TOCC and decides whether the patient needs to be tested for COVID-19 diagnosis. All suspected cases of COVID-19 would be isolated and monitored. If a patient has persistent dental issues, the ED doctor will request a dental consultation. A dentist would undertake an initial patient evaluation via telemedicine or telephonic consultation. For a patient who is quarantined at the hospital because of COVID-19, dental conditions are initially evaluated by a physician followed by referral for a telemedicine dental consultation, if required.
Individuals under home self-quarantine and quarantined in a designated quarantine site due to overseas travel history or contact tracing to confirmed cases can call the epidemic prevention call center helpline 1922 for instructions and assistance for urgent dental concerns. As mentioned above, an initial dental evaluation via telemedicine or telephone consultation is undertaken to assess the patient's dental problem. We had an example of successfully solving the oral problems of an elderly person who was isolated in a central quarantine site and complained of chewing pain while wearing his removable prosthesis via telephone consultation. We taught the patient how to relieve the pain and suggested the caregiver of quarantine site to arrange soft-diet for him.
Based on the telemedicine or telephonic consultation, all non-emergent dental concerns will be delayed until COVID-19 symptoms have improved and the quarantine ends. In patients with a true dental emergency, dental care can be provided in an isolated or a negative-pressure treatment room by personnel using Level 3 PPE.
The SARS-CoV-2 can survive on various surfaces from a few hours to days. Therefore, treatment room sanitation and disinfection with the appropriate disinfection guidelines is needed to decrease contact transmission.
This standard triage and workflow protocol is well performed in Taipei City Hospital and should be suitable to other community and regional hospitals. The dental practitioners of the private dental clinics have to access the patients’ condition including body temperature and TOCC before any dental treatment performed under the complete Level 3 PPE protection. To postpone non-emergency dental treatments of the suspected patients and referred the high-risk patients to hospital for emergency dental treatments are recommended.
Conclusion
Dental procedures necessitate close-proximity, face-to-face practices and involves the use of rotary instruments, high-speed handheld tools, air–water syringes and sharp surgical instrument. These procedures create visible aerosol sprays containing droplets with an admixture of water, saliva, blood, and other debris that are potentially contaminated with SARS-CoV-2, which increase the infection risk among dental personnel.
There are concerns associated with asymptomatic carrier transmission so a strict well-designed triage and workflow protocol is needed for dental professionals to screen against high-risk patient infection transmission and reduce the potential risk of nosocomial COVID-19 transmission developed from the dental department.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
Contributor Information
Ya-Ling Lee, Email: DAE30@tpech.gov.tw.
Yung-Feng Yen, Email: DAM37@tpech.gov.tw.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P., Yang X.L., Wang X.G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Trav Med. 2020;27 doi: 10.1093/jtm/taaa021. taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Listed N.A. MERS-CoV: a global challenge. Lancet. 2013;381:1960. doi: 10.1016/S0140-6736(13)61184-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ong S.W.X., Tan Y.K., Chia P.Y. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. Jama. 2020;323:1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai Y., Yao L., Wei T. Presumed asymptomatic carrier transmission of COVID-19. Jama. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wölfel R., Corman V.M., Guggemos W. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020 Apr 01 doi: 10.1038/s41586-020-2196-x. [Epubahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Tong Z.D., Tang A., Li K.F. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang province, China, 2020. Emerg Infect Dis. 2020;26:1052–1054. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doremalen N.V., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]