Highlights
-
•
Fungal endocarditis/aortitis.
-
•
The first case of polyethylene-terephthalate (PETE) graft aortitis caused by A. niger.
-
•
Transoesophageal echocardiography (TEE).
Keywords: fungal infection, aspergillus niger, aortitis, echocardiography
Abstract
Fungal endocarditis/aortitis is an uncommon yet emerging entity accounting for 2% to 4% of all cases of infective endocarditis and continues to be associated with a poor prognosis. We present the first case of polyethylene-terephthalate (PETE) graft aortitis caused by A. niger, a rare fungal agent. Early diagnosis with frequent transoesophageal echocardiography (TEE) and a prompt surgical intervention coupled with optimal antifungal therapy are still the only option to reduce the exceedingly high mortality and morbidity.
Introduction
Aspergillus is an opportunistic nosocomial fungus generally associated with a high mortality rate [1]. While A. fumigatus has been reported to be the most frequent cause of aspergillosis, A. niger has been rarely associated with infection and only few cases have been reported in patients who have recently undergone valvular heart surgery [[2], [3], [4], [5]] and pacemaker implantation [6], as well as in patients with neoplastic diseases, intravenous treatment or drug addiction, long-term parenteral feeding and immunosuppression.
Case report
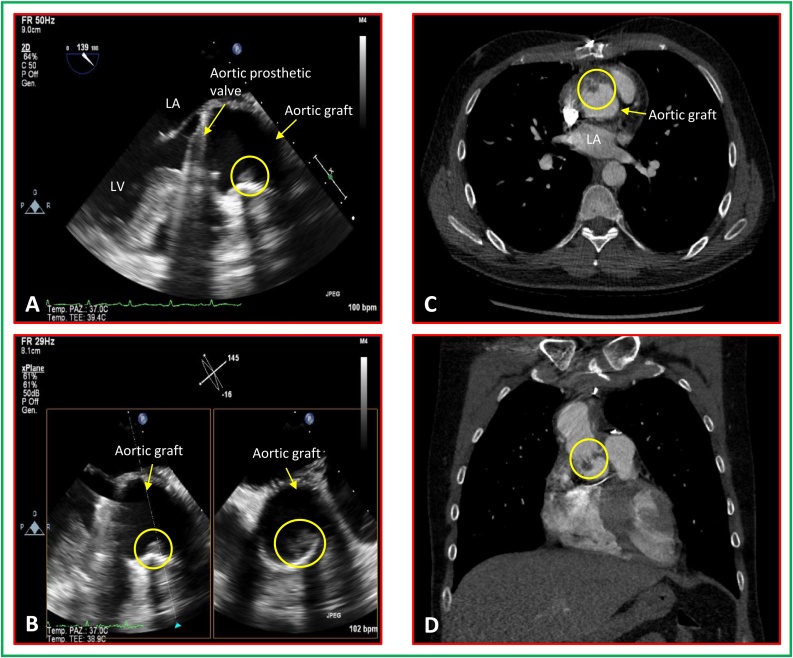
A 38-year-old man with a history of congenital aortic valve stenosis underwent a mechanical aortic valve replacement (21 mm SJ Regent) with aortotomy closure by a pericardium patch at an external center. The postoperative period was impacted by sporadic fever treated with empiric antibacterial therapy (amoxicillin) but two months after surgery he was referred to our center due to continuing low-grade fever and mild leucocytosis (13.2 109/L); Apart from these signs his physical examination was unremarkable and there were no signs of petechiae, splenomegaly or clubbing. All microbiological evaluations were uneventful, transoesophageal echocardiography (TEE) examination showed no endocarditis signs but computerized tomography (CT) scan unveiled a pseudo-aneurysmatic degeneration (6.5 × 5.3 cm) on the aortic wall in correspondence of the aortotomy suture. Reoperation was decided upon and he underwent an ascending aortic replacement with polyethylene-terephthalate (PETE) 28 mm Hemashield graft and no signs suggestive of active infection were detected in the pericardial patch, therefore cultures of the sample was not performed; He was discharged in excellent condition but after 7 months he was re-admitted to our center for new onset of fever (> 38 °C) and malaise, distal leg and spleen embolization and high levels of inflammatory biomarkers (WBC 16.3 109/L, CRP 220 mg/dL). In cardiac auscultation, cardiac sounds were rhythmic and metallic valve sound was heard. The TEE showed a regular aortic prosthesis, the CT scan a peri-aortic fluid collection without enhancement and the positron emission tomography (PET) confirmed a nonspecific postoperative collection around the graft. All four blood culture sets were negative as were serologies for rickettsia and Q fever. The patient was treated empirically with vancomycin and ceftriaxone and fever subsided and two different TEEs confirmed no sign of endocarditis. After three weeks of antibacterial therapy, inflammatory biomarkers increased again (WBC 14.8 109/L, CRP 101 mg/dL) and for the first time TEE revealed two mobile masses (15 x 16 mm each), suggestive of vegetations, with a stalk at the ascending aorta graft wall (Fig. 1A, B; Supp Video) one cm around over the right coronary ostium without evidence of valvular damage. A new CT scan confirmed the diagnosis showing a 8 mm filling defect in the same position (Fig. 1C, D). All six blood culture sets were negative and with the diagnosis of culture-negative graft aortitis caspofungin was administered due to the β-d-glucan (BDG) positivity (> 500 pg/mL). Repeat surgery was performed with aortic homograft root implantation and intraoperative exploration confirmed the aortitis of the PETE prothesis and the resected material was sent to the microbiology laboratories: direct microscopy of the vegetation stained with 10% KOH-Quink revealed septate hyphae and culture grew A. niger. The patient’s hemodynamic has been supported by dobutamine for 8 days and heart rate by temporary epicardial ventricular pacing due to third-degree atrioventricular block with following spontaneous recovery with sinus rhythm. The patient received parenteral liposomal amphotericin-B (5 mg/kg per day) for 45 days followed by oral voriconazole for another 6 months with good clinical evolution. The six-month follow-up TEE showed no endocarditis/aortitis and all the inflammatory biomarkers were negative.
Fig. 1.
TEE showing the mobile masses (in the yellow circle) suggestive of vegetations with a stalk at the ascending aorta graft wall (A: 130°, mid-esophageal, long-axis view; B: X-plane view); CT scan revealing a filling defect (in the yellow circle) in the aortic graft (C: axial plane; D: coronal plane). LA, left atrium; LV, left ventricle.
Discussion
Fungal endocarditis/aortitis is an uncommon yet emerging entity accounting for 2% to 4% of all cases of infective endocarditis and continues to be associated with a poor prognosis [7]. A. fumigatus is the most common fungal agent responsible for the aspergillus aortitis and its diagnosis is very difficult. Blood cultures are negative in over 50% of cases, β‐D‐glucan has a sensitivity and specificity of 69.9% and 87.1% respectively [7] and the infection may be overlooked by transthoracic echocardiography as it localizes in the ascending aorta. This represents the fourth case of A. niger aortitis [4,5,8], the first one involving a PETE graft. The only predisposing factor for A. niger infection in this patient was the first open heart surgery. Although A. niger mycotic endocarditis/aortitis is rare among immunocompetent patients, the diagnosis should be considered for all patients with fever and an unidentified infection origin who have had heart surgery. The case emphasizes the role of serial TEEs in the diagnosis and management of these patients particularly with negative cultures and it illustrates the possible insidious course of fungal endocarditis/aortitis that continues to be associated with a poor prognosis. Early diagnosis and a prompt surgical intervention coupled with optimal antifungal therapy are still our only option to reduce the exceedingly high mortality and morbidity.
Author statement
All authors have read and approved the manuscript; in particular:
Matteo Marro and Francesco Atzeni wrote the paper and elaborated the images.
Michele La Torre, Matteo Attisani e Mauro rinaldi performed the surgeries.
Stefania Belloro and Francesco De Rosa managed the antimicrobiological therapy and followed the patient after the surgery.
Mauro Rinaldi revised the manuscript critically for important intellectual content.
Funding source
No funding has been needed for this work.
Ethical approval
The whole work, text and figures too, have been authorized by the patient and ethical committee.
Declaration of Competing Interest
The authors declare that there are no conflicts of interest.
Acknowledgment
None.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.idcr.2020.e00823.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Glampedakis E., Cassaing S., Fekkar A., et al. Invasive aspergillosis due to Aspergillus section Usti: a multicenter retrospective study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa230. [DOI] [PubMed] [Google Scholar]
- 2.Moore R.S., Hasleton P.S., Lawson R.A., Stanbridge T.N. Aspergillus niger endocarditis complicating aortic tissue valve replacement. Thorax. 1984;39(1):76–77. doi: 10.1136/thx.39.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kreiss Y., Vered Z., Keller N., Kochva I., Sidi Y., Gur H. Aspergillus niger endocarditis in an immunocompetent patient: an unusual course. Postgrad Med J. 2000;76(892):105–106. doi: 10.1136/pmj.76.892.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duygu H., Nalbantgil S., Ozerkan F., Kirilmaz B., Yagdi T. Aspergillus niger aortitis after aortic valve replacement diagnosed by transesophageal echocardiography. Echocardiography. 2006;23(5):405–406. doi: 10.1111/j.1540-8175.2006.00122.x. [DOI] [PubMed] [Google Scholar]
- 5.Jamieson R.W., Wallace W.A., Din J.N., Raza Z. Acute aortic occlusion with sudden paraplegia secondary to Aspergillus niger embolism from Aspergillus niger aortitis. J Vasc Surg. 2011;54(5):1472–1474. doi: 10.1016/j.jvs.2011.04.056. [DOI] [PubMed] [Google Scholar]
- 6.Ho I.C., Milan D.J., Mansour M.C., et al. Fungal infection of implantable cardioverter-defibrillators: case series of five patients managed over 22 years. Heart Rhythm. 2006;3(8):919–923. doi: 10.1016/j.hrthm.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Ammannaya G.K.K., Sripad N. Fungal endocarditis: what do we know in 2019? Kardiol Pol. 2019;77(7-8):670–673. doi: 10.33963/KP.14869. [DOI] [PubMed] [Google Scholar]
- 8.Noordally S.O., Sohawon S., De Bels D., Duttmann R., Gottignies P., Devriendt J. Late onset of Aspergillus aortitis presenting as femoral artery embolism following coronary artery bypass graft surgery. Acta Medica (Hradec Kralove) 2011;54(4):175–176. doi: 10.14712/18059694.2016.45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.