Most often, a fracture of the proximal humeral lesser tuberosity (LT) is combined with a posterior dislocation of the shoulder12 or an associated greater tuberosity fracture. Reports of isolated avulsion fracture of the LT are uncommon; it occurs primarily in the adolescent population.5 The injury usually follows with an acute forced abduction–external rotation of the upper arm to the shoulder.13,16 It is interesting to note that several reports have imputed the injury to the overuse of the shoulder involving fly fishing and pitching.17 Although patients tend to complain about anterior shoulder pain with weakness of the subscapularis muscle,17 the diagnosis is often delayed. Moreover, the plain radiographic findings, often negative, are misleading in the early stage.
Conservative treatment is generally considered for slight displacement of a bone fragment with a satisfactory functional outcome.7 Surgical treatment for a dislocated avulsion fracture involves open reduction–internal fixation1,17 and arthroscopic reconstruction.4,11,14 We present the case of an isolated subscapularis avulsion in a middle-aged female patient, which—to our knowledge—is the first report of a double-row knotless arthroscopic repair technique with suture anchors.
Case report
A healthy 38-year-old female patient presented to the primary hospital after she fell onto a wet floor with an acute abduction–external rotation of the upper arm to the shoulder in January 2019. She experienced severe pain and swelling in the left shoulder. With negative plain radiologic report findings, she was sent home. However, she complained about the persistent pain and weakness in internal rotation and was transferred to our hospital. The 3-dimensional computed tomography (3D-CT) scan and magnetic resonance imaging (MRI) in the axial plane revealed the subscapularis avulsion fracture with no rotator cuff tear, whereas the radiographic findings were negative again (Fig. 1).
Figure 1.
Preoperative 3-dimensional computed tomography (a-c) and magnetic resonance imaging (d) in the axial plane show a fracture of the lesser tuberosity (→), whereas the radiographic findings (e, f) are negative.
The patient's left shoulder showed swelling. She had tenderness over the anterior of the shoulder and pain on all passive and active motions, especially internal rotation. Because of her pain, evaluation of the rotator cuff and shoulder instability could hardly be performed. However, she had a positive belly-press test finding. No neurologic or vascular injury was detected.
With the patient under general anesthesia, in the lateral decubitus position, a standard posterior portal was created to examine the glenohumeral joint and subacromial space. Besides the fracture, several co-pathologies were detected, including looseness of the long head of the biceps tendon in the groove without dislocation, as well as adhesion and contraction of the glenohumeral joint. Considering these co-pathologies, arthroscopic circumferential capsulotomy, adhesion lysis, and thorough débridement of both the glenohumeral joint and subacromial space were performed through anterior and lateral portals.
After detection and débridement of the avulsion fracture through anterior, lateral, and anterosuperior portals, 1 polydioxanone suture was introduced through the subscapularis tendon to control and retract the avulsion fracture. One suture anchor with 4 limbs of FiberWire (Arthrex, Naples, FL, USA) was screwed into the medial side of the bicipital groove. The polydioxanone suture was pulled out through the anterosuperior portal, shuttling 1 limb of the FiberWire through the subscapularis tendon. Another 3 limbs of FiberWire were dealt with in the same fashion in the lateral, posterior, and lateral-posterior region to where the first limb was perforated. Therefore, these 4 limbs crossed over the subscapularis tendon and the fragment and were fixed into the distal humerus head with a Versalok screw (DePuy Mitek, Raynham, MA, USA). In this way, the avulsion fragment could tightly reduce to the anatomic side of the humeral head (Fig. 2). Finally, biceps tenotomy was performed for prevention of postoperative inflammation and pain.
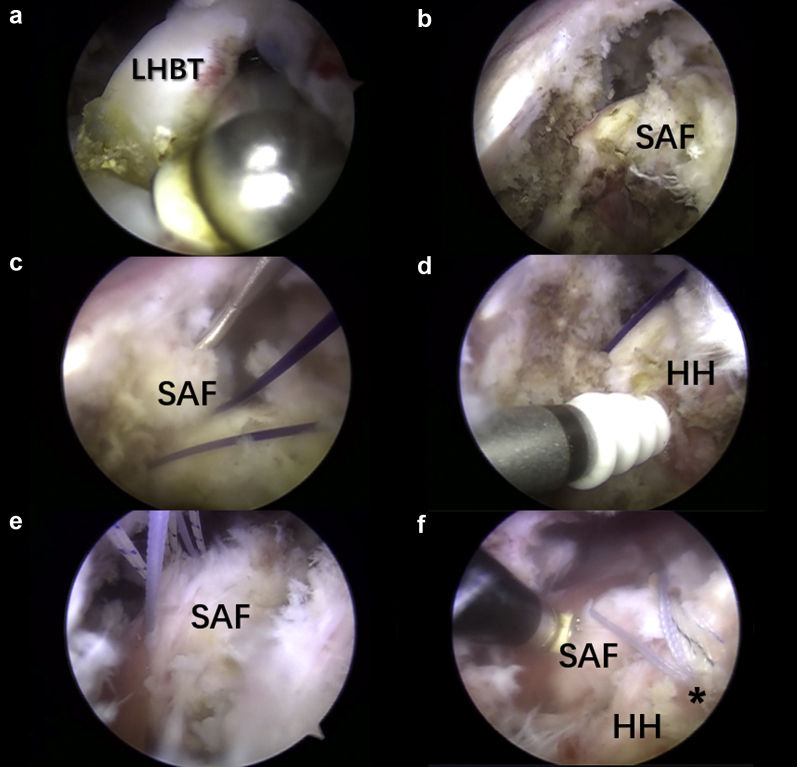
Figure 2.
Intraoperative arthroscopic views. (a) Long head of biceps tendon (LHBT) tenotomy. (b) The subscapularis avulsion fracture (SAF) is visualized. (c) Polydioxanone suture is introduced and transferred through the subscapularis. (d) A suture anchor with 4 FiberWires is screwed into the medial side of the bicipital groove. (e) All FiberWires are shuttled through the subscapularis tendon using polydioxanone sutures. (f) The SAF is anatomically reduced with all suture limbs fixed onto the humeral head (HH) with a Versalok screw (*).
The left arm was put in a brace in the neutral position of the shoulder for 6 weeks. Active range of motion was started on the first postoperative day and limited to 30° of flexion and extension. The patient was allowed to perform passive abduction up to 30°. However, active or passive external rotation should be avoided to prevent a possible re-avulsion for 6 weeks. Moreover, no weight lifting was allowed for the affected shoulder. After 6 weeks, the brace was removed, allowing full active-assisted exercise.
Results
The follow-up was undertaken at 6 weeks, 3 months, and 6 months postoperatively. Postoperative radiographs (anteroposterior and scapular views), 3D-CT, and MRI were performed at the latest follow-up. Six months after surgery, the Constant score improved from 11 to 92 points and the American Shoulder and Elbow Surgeons score improved from 10.01 to 88.32 points. Pain was remarkably relieved. The patient resumed work and was able to accomplish daily life activities. She achieved almost full range of motion (Fig. 3). The lift-off and Napoleon signs showed negative findings. The 3D-CT and MRI scans showed that the LT was well reduced to the anatomic position and the fracture had healed (Fig. 4).
Figure 3.
(a) At 6 months postoperatively, external rotation of the affected arm returned to normal. (b) Forward elevation of the left arm is similar to that of the unaffected side.
Figure 4.
Postoperative 3-dimensional computed tomography (a, b) and magnetic resonance imaging (MRI) (c, d) show that the lesser tuberosity is well reduced to the anatomic position and the fracture (→) has healed.
Discussion
An isolated subscapularis avulsion fracture is often missed by the initial doctor in the emergency department. Patients are inclined to complain about the palpated pain at the anterior of the shoulder right after the injury, probably along with the restriction of motion. Because of the overall pain and restriction, it is difficult or confusing to perform the lift-off, belly-press, or Napoleon test to evaluate the integrity of the subscapularis tendon. Moreover, the fracture, especially with no or little displacement, is often undetected on the plain radiographs, although the use of the axillary view to identify small fragments with little displacement has been reported.14 Thus, a 3D-CT scan is recommended for early diagnosis; besides, an MRI study could be used to rule out other lesions, such as rotator cuff tears.
Currently, there is no consensus on the treatment options. Levine et al8 suggested that LT displacement by an amount greater than 5 mm or angulation greater than 45° be the criterion for surgery. Scheibel et al14 indicated that open procedures are suitable for severely dislocated fractures with displacement of the long head of the biceps whereas arthroscopic techniques are recommended in cases of an isolated subscapularis avulsion with less severe dislocation. However, there are no published data comparing the clinical results of the 2 techniques in the long term. Although Vezeridis et al18 found that their open reduction–internal fixation procedure was suitable for a large avulsion fracture, it might be difficult to perform fixation for a small fracture. In our case, fracture displacement was 7 mm; despite the possible difficulties and challenges when performing arthroscopic repair,8 the less invasive procedure was recommended. The surgical procedure, performed by a senior doctor (J.Z.), took around 1 hour, a shorter surgical time than reported for arthroscopic double-row repair of greater tuberosity fractures and close to that for the open procedure.9 Moreover, patients who underwent arthroscopic double-row suture anchor fixation were shown to have better range of motion and higher American Shoulder and Elbow Surgeons scores than those who underwent an open reduction–internal fixation procedure.9
After surgery, our patient attained early rehabilitation. At 6 months postoperatively, she returned to work and coped with daily life activities with no pain or difficulties. The physical examination showed functional recovery of the subscapularis, whereas the radiologic results revealed anatomic reunion. With minimally invasive surgery, patients could endure less pain and shorter rehabilitation periods; surgeons could treat co-pathology simultaneously (eg, adhesion, subluxated long head of the biceps tendon, superior labrum anterior-posterior tear, or Hill-Sachs lesions4). In terms of the biceps lesion, biceps tenotomy rather than tenodesis was chosen partially considering that the middle-aged patient was an ordinary office clerk with no desire for sport. She requested to reattain painlessness and daily life activities. Moreover, tenotomy presented an earlier improvement in postoperative pain relatively.2 Thus, tenotomy of the biceps tendon was indicated in our middle-aged patient with pain and no need for heavy work or sport. However, ranges of practice patterns observed in a patient of this age entail being further analyzed and generalized. Furthermore, through the arthroscopic procedure, nerves and vessels can be protected more visually through exact standard portals and no instrumentation pierces the fragment, eluding secondary fracture and loose fixation.
In the biomechanical research on avulsion fracture, compared with transosseous braided-tape fixation, double-row repair techniques showed stronger and more stable properties.3 Compared with single-row repair in terms of greater tuberosity fractures, double-row suture anchor fixation could avoid over-reduction of the fragment and represented boosted load to failure on biomechanical assessment.15 Lin et al10 further established that suture anchor fixation was stronger than screw fixation and that double-row suture anchor fixation showed better contact performance at all tested abduction angles than a suture bridge construct.
Limited biomechanical research on arthroscopic avulsion fracture repair has been reported, whereas several reports using arthroscopic procedures have shown acceptable clinical results trying to approach maximal anatomic healing, as described by Scheibel et al,14 Heyworth et al,6 and Cregar et al.4 Scheibel et al and Heyworth et al proposed mattress suture formation anterior to the subscapularis tendon to ensure secure fixation. However, the anchors were inserted directly into the fracture site with relatively less bony contact interface for healing. Cregar et al put the anchors lateral to the fracture site using a bridging technique to enlarge the limited contact area with 2 sutures covering the fragment.
Our arthroscopic double-row repair procedure using suture anchors further improved the technique performed by Cregar et al.4 With 4 sutures crossed over the fragment, which reduced tightly to the LT bone bed, our procedure presented an enlarged contact area and improved anatomic footprint.
Conclusion
MRI and 3D-CT are necessary for the early diagnosis of an isolated subscapularis avulsion fracture. Operative intervention, especially arthroscopic procedures, is mainly recommended for fracture displacement and co-pathology. Our double-row knotless arthroscopic repair for an isolated subscapularis avulsion fracture resulted in good clinical and radiologic outcomes at mid-term follow-up.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
No institutional review board approval was required for this case report.
References
- 1.Aagaard K.E., Lunsjo K. Occult fracture of the lesser tuberosity in a 9-year-old female swimmer. J Surg Case Rep. 2017;1:1–3. doi: 10.1093/jscr/rjw238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belay E.S., Wittstein J.R., Garrigues G.E., Lassiter T.E., Scribani M., Goldner R.D. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2019;27:4032–4037. doi: 10.1007/s00167-019-05682-1. [DOI] [PubMed] [Google Scholar]
- 3.Brais G., Menard J., Mutch J., Laflamme G.Y., Petit Y., Rouleau D.M. Transosseous braided-tape and double-row fixations are better than tension band for avulsion-type greater tuberosity fractures. Injury. 2015;46:1007–1012. doi: 10.1016/j.injury.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Cregar W.M., MacLean I.S., Verma N.N., Trenhaile S.W. Lesser tuberosity avulsion fracture repair using knotless arthroscopic fixation. Arthrosc Tech. 2018;7:e899–e905. doi: 10.1016/j.eats.2018.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gruson K.I., Ruchelsman D.E., Tejwani N.C. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39:284–298. doi: 10.1016/j.injury.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Heyworth B.E., Dodson C.C., Altchek D.W. Arthroscopic repair of isolated subscapularis avulsion injuries in adolescent athletes. Clin J Sport Med. 2019;18:461–463. doi: 10.1097/JSM.0b013e318188b1a5. [DOI] [PubMed] [Google Scholar]
- 7.Koper M.C., Jakma T.S. Case report of a proximal humeral fracture with an avulsion fracture of the lesser tuberosity in an adolescent girl. J Shoulder Elbow Surg. 2015;24:e260–e263. doi: 10.1016/j.jse.2015.05.054. [DOI] [PubMed] [Google Scholar]
- 8.Levine B., Pereira D., Rosen J. Avulsion fractures of the lesser tuberosity of the humerus in adolescents: review of the literature and case report. J Orthop Trauma. 2005;19:349–352. http://doi.org/01.bot.0000133859.59390.0f. [PubMed] [Google Scholar]
- 9.Liao W., Zhang H., Li Z., Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clin Orthop Relat Res. 2016;474:1269–1279. doi: 10.1007/s11999-015-4663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin C.L., Yeh M.L., Su F.C., Wang Y.C., Chiang C.H., Hong C.K. Different suture anchor fixation techniques affect contact properties in humeral greater tuberosity fracture: a biomechanical study. BMC Musculoskelet Disord. 2019;20:26. doi: 10.1186/s12891-019-2412-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nikolaou V.S., Chytas D., Tyrpenou E., Babis G.C. Two-level reconstruction of isolated fracture of the lesser tuberosity of the humerus. World J Clin Cases. 2014;2:219–223. doi: 10.12998/wjcc.v2.i6.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robinson C.M., Teoh K.H., Baker A., Bell L. Fractures of the lesser tuberosity of the humerus. J Bone Joint Surg Am. 2009;91:512–520. doi: 10.2106/JBJS.H.00409. [DOI] [PubMed] [Google Scholar]
- 13.Ross G.L., Love M.B. Isolated avulsion fracture of the lesser tuberosity of the humerus: report of two cases. Radiology. 1989;172:833–834. doi: 10.1148/radiology.172.3.2772197. [DOI] [PubMed] [Google Scholar]
- 14.Scheibel M., Martinek V., Imhoff A.B. Arthroscopic reconstruction of an isolated avulsion fracture of the lesser tuberosity. Arthroscopy. 2005;21:487–494. doi: 10.1016/j.arthro.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Seppel G., Saier T., Martetschlager F., Plath J.E., Guevara-Alvarez A., Henschel J. Single versus double row suture anchor fixation for greater tuberosity fractures—a biomechanical study. BMC Musculoskelet Disord. 2017;18:506. doi: 10.1186/s12891-017-1868-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shibuya S., Ogawa K. Isolated avulsion fracture of the lesser tuberosity of the humerus. A case report. Clin Orthop Relat Res. 1986:215–218. [PubMed] [Google Scholar]
- 17.Vavken P., Bae D.S., Waters P.M., Flutie B., Kramer D.E. Treating subscapularis and lesser tuberosity avulsion injuries in skeletally immature patients: a systematic review. Arthroscopy. 2016;32:919–928. doi: 10.1016/j.arthro.2015.10.022. [DOI] [PubMed] [Google Scholar]
- 18.Vezeridis P.S., Bae D.S., Kocher M.S., Kramer D.E., Yen Y.-M., Waters P.M. Surgical treatment for avulsion injuries of the humeral lesser tuberosity apophysis in adolescents. J Bone Joint Surg Am. 2011;93:1882–1888. doi: 10.2106/JBJS.K.00450. [DOI] [PubMed] [Google Scholar]