Abstract
Background
Concomitant biceps tendon pathology is often present in patients undergoing rotator cuff repair (RCR). Management of biceps pathology has been reported to influence outcomes of RCR; however, the impact on the pace of recovery remains unclear. The purpose of this study was to analyze the effects of simultaneous RCR with biceps tenodesis (RCR-BT) on time to achieve maximum improvement and recovery speed for pain and function.
Methods
A retrospective review of 535 patients who underwent primary RCR for full-thickness tears. Patients treated with simultaneous RCR-BT were compared with RCR-only. Outcome measures and motion were recorded at preoperative routine postoperative intervals. Plateau in maximal improvement and recovery speed were analyzed for both pain and functional recovery.
Results
Baseline American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) function was significantly lower for the RCR-BT cohort (20.5) compared with RCR-only (23.9; P = .008). For visual analog scale (VAS) pain and measured motion, the plateau in maximal improvement occurred at 6 months for RCR-BT compared with 12 months for the RCR-only group. The remainder of the patient-reported outcome measures took 12 months to achieve a plateau in maximal improvement. At 3 months, 79% of improvement in pain and 42%-49% of functional improvement was achieved in the RCR-BT cohort. Similarly, at 3 months, the RCR-only cohort achieved 73% of pain improvement and 36%-57% of functional improvement at 3 months.
Conclusion
Patients requiring RCR with simultaneous biceps tenodesis have lower baseline ASES function and earlier postoperative plateaus in pain relief and motion improvement following surgery. Nonetheless, the speed of recovery was not influenced by the biceps tenodesis.
Keywords: Biceps tenodesis, arthroscopic rotator cuff tear, concomitant, speed of recovery, plateau, range of motion, patient-reported outcome measures
Concomitant long head biceps tendon pathology is frequently observed in patients with rotator cuff tears (RCTs) and is a known cause of anterior shoulder pain. The reported incidence of biceps tendon pathology in the setting of RCT ranges from 36%-83%,7,21 with worse biceps pathology seen in larger rotator cuff tears.6 Procedures including subacromial decompression, distal clavicle excision, and biceps tenodesis or tenotomy are routinely performed during arthroscopic rotator cuff repair (RCR) despite inconclusive evidence of their benefits.1,5,16,22 Although there is no consensus on best treatment for biceps tendon pathology, in the setting of significant biceps tendon tearing or instability, a biceps tenotomy or biceps tenodesis (BT) is often performed in an effort to eliminate the biceps tendon as a pain generator. Nonetheless, concomitant RCR-BT is being performed with increasing frequency, nearly tripling in incidence from 2005 to 2011.9,18 Furthermore, the current health care structure emphasizes cost efficiency and patient satisfaction, highlighting the importance of understanding how biceps tenodesis impacts recovery at various time points in the recovery process.
Numerous studies have demonstrated pain relief and functional improvement following isolated biceps tenodesis.3,19 To date, there is only 1 report that investigated the differences between isolated RCR and RCR with biceps surgery, at a minimum 1 year postoperatively.20 This study determined that the addition of either biceps tenodesis or tenotomy resulted in superior improvements for VAS pain (P = .02) and American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) scores (P = .032) compared with isolated RCR.20 However, it failed to elucidate when patients can expect to achieve improvements, and to what degree improvement was achieved at various time intervals during the recovery process. Previous work at our institution has demonstrated that the speed of recovery following rotator cuff repair saw 75% of pain relief and 50% of functional recovery at 3 months; however, maximum recovery typically took a full year to reach a plateau regardless of tear size.11 For those patients undergoing concomitant arthroscopic RCR-BT, defining the impact of biceps tenodesis on the recovery process remains unclear. The purpose of this study was to analyze the effect of concomitant biceps tenodesis on the speed of recovery and overall outcomes following RCR. We hypothesize that concomitant biceps tenodesis will improve the speed of recovery and overall outcomes following RCR.
Methods
A retrospective query of a single-institution shoulder surgery repository (WIRB Study no. 1138999, WIRB Protocol no. 20130731) was used to identify all patients undergoing primary arthroscopic RCR from November 2006 to December 2015. According to the standard registry protocol, patient-reported outcome measures (PROMs) and active range of motion (ROM) data collected via best-effort goniometer measurements were recorded preoperatively and at 3-month, 6-month, 1-year, and 2-year postoperative intervals. PROMs used included those for pain (visual analog scale [VAS] pain) and shoulder function (Simple Shoulder Test [SST], ASES, VAS Function, Single Assessment Numeric Evaluation). Patients were included in the study if they underwent primary arthroscopic RCR for full-thickness rotator cuff tears involving the supraspinatus, with or without biceps tenodesis, and had postoperative interval outcome data available at a minimum of the 6-month follow-up data point. Patients were excluded if they underwent a partial RCR, revision RCR, or a simultaneous biceps tenotomy during RCR. Missing data in a specific time point was replaced using group means from existing intervals.
All surgeries were performed at a single, high-volume institution by a shoulder and elbow fellowship-trained orthopedic surgeon (senior author, J.C.L.). Beach chair positioning was used for all procedures, and rotator cuff repair was performed arthroscopically according to tear size as previously described.11 Intraoperative assessment of tear size using the Patte classification was recorded based on description within the operative record.17 If subluxation and/or partial tearing of the long head of the biceps tendon or instability of the biceps origin was observed intraoperatively, the biceps was extracted out of the anterolateral portal, and a Krackow suture was placed into the tendon. A biceps tenodesis was performed at the end of the case using either a lateral row tenodesis technique14 or tenodesis within the bicipital groove using a knotless suture anchor. All patients were placed in a shoulder immobilizer for the first 6 weeks postoperatively. Those with Patte grade 1 tears17 were allowed early active assist and passive motion based on a physical therapist–directed protocol. Those with Patte grade 2 or grade 3 tears used a self-directed home therapy program consisting of pendulum exercises for the initial 6 weeks postoperatively, followed by active-assisted stretching exercises for 6 weeks. Strengthening exercises were not prescribed for any patient until after 3 months postoperatively.
Using a methodology identical to that used for evaluating the plateau in maximal improvement and speed of recovery following arthroscopic rotator cuff repairs, the outcome, pain, and motion data from preoperative, 3-month, 6-month, 1-year, and 2-year postoperative intervals were analyzed. 11
Plateau in maximal improvement
Using previous methodology,15 the plateau in maximal improvement was defined as the follow-up point at which no subsequent statistically significant improvement was observed compared with the immediately preceding follow-up interval.
Speed of recovery
Speed of recovery was defined as the percentage of the total improvement (achieved at the plateau point) attained at each follow-up interval for each outcome measure.15
Statistical analysis
Subgroup comparative analysis was performed for patients with simultaneous biceps tenodesis vs. patients without biceps tenodesis. Demographics including age, sex, and body mass index were queried and compared between groups, in addition to retraction grade, mean outcomes, speed of recovery for PROMs, and motion at each time interval. Plateaus in maximal improvement were also determined for each subgroup.
Independent samples t test, paired samples t tests, and repeated measures analyses of variance were used where appropriate. Statistical analyses were conducted using SPSS, version 22 (IBM, Armonk, NY, USA). Significance was set at P < .05.
Results
During the 9-year study period, 759 patients were treated with an arthroscopic rotator cuff repair for full-thickness rotator cuff tears. There were 535 patients (342 males and 193 females) who met the inclusion criteria. The mean age at surgery was 61.5 years (range 29.8-84.3 years) and the mean body mass index was 28.2. Two cohorts were created: patients who underwent an isolated arthroscopic rotator cuff repair (RCR-only, n = 370 patients) and those who had an arthroscopic rotator cuff repair with concomitant biceps tenodesis (RCR-BT, n = 165 patients). Mean age and sex ratios were similar between the 2 groups; however, the RCR-only cohort demonstrated a significantly higher mean body mass index (28.51 vs. 27.49, P = .025; Table I). Additionally, similar rates of Patte grade 1 and 3 rotator cuff tears were observed in both groups, but there were significantly more grade 2 tears in the RCR-BT cohort (37.6% vs. 28.9%, P = .049; Table II).
Table I.
Comparison of demographic data between patients with rotator cuff repair only (RCR-only) and those with concomitant biceps tenodesis (RCR-BT)
| RCR-only (n = 370) |
RCR-BT (n = 165) |
P value | |
|---|---|---|---|
| Age, yr | 61.14 | 62.35 | .158 |
| Sex, male-female | 228:142 | 114:51 | .097 |
| Body mass index | 28.51 | 27.49 | .025 |
Table II.
Comparison of rotator cuff retraction grade between groups using the Patte classification
| Retraction grade | RCR-only n (%) (n = 370) |
RCR-BT n (%) (n = 165) |
P value |
|---|---|---|---|
| 1 | 193 (52.16) | 75 (45.45) | .152 |
| 2 | 107 (28.92) | 62 (37.58) | .047 |
| 3 | 69 (18.65) | 28 (16.97) | .642 |
| Unknown | 1 (2.70) | 0 (0.00) | n/a |
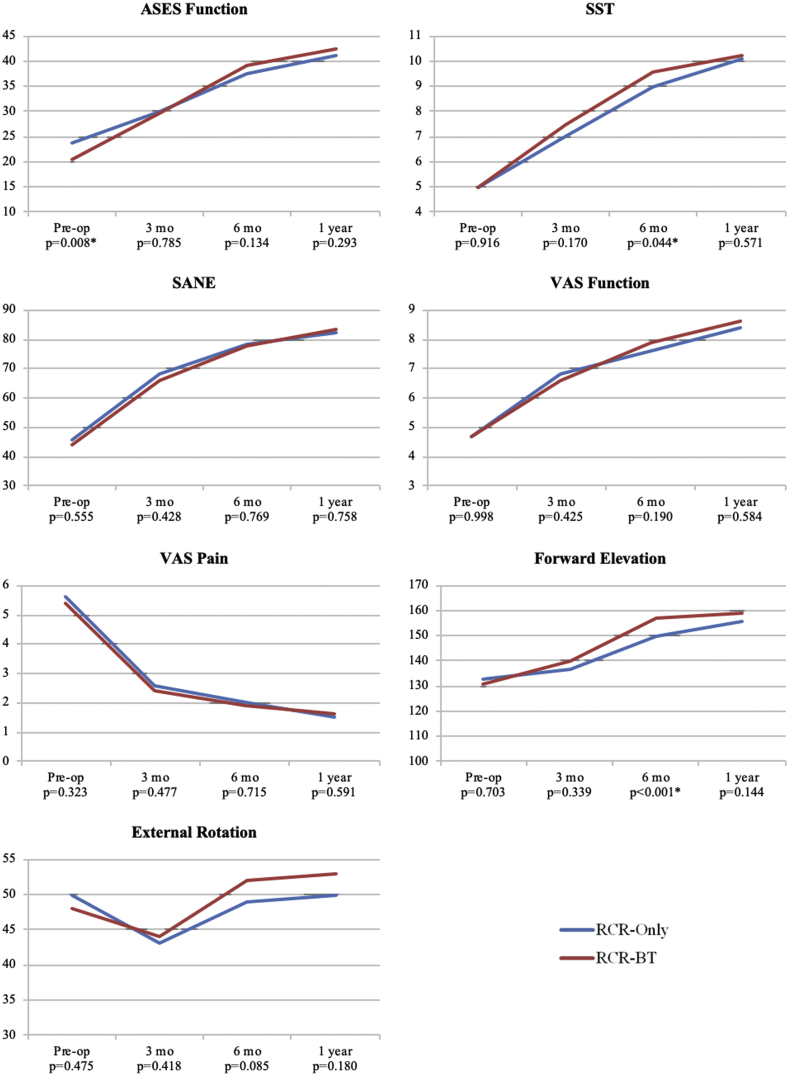
Baseline SST, Single Assessment Numeric Evaluation, VAS function, VAS pain, forward elevation (FE), and external rotation (ER) were similar between the 2 cohorts. However, baseline ASES function was significantly lower (20.5) in the RCR-BT cohort compared with RCR-only (23.9; P = .008; Table III). Equivalent outcomes for all measures between cohorts were observed at 3 and 12 months postoperatively. However, at the 6-month follow-up, RCR-BT demonstrated higher SST (9.6 vs. 9.0; P = .044) and greater FE (157o vs. 150o; P < .001) compared with RCR only (Table III, Fig. 1).
Table III.
Comparison of outcomes at various time points in recovery for patients who underwent rotator cuff repair only or rotator cuff repair with biceps tenodesis
| Interval | Procedure | ASES function | SST | SANE | VAS function | VAS pain | FE | ER |
|---|---|---|---|---|---|---|---|---|
| Preoperation | RCR only | 23.9 | 5.0 | 45.7 | 4.7 | 5.6 | 133 | 50 |
| Biceps tenodesis | 20.5 | 5.0 | 44.1 | 4.7 | 5.4 | 131 | 48 | |
| P value | .008∗ | .916 | .555 | .998 | .323 | .703 | .475 | |
| 3 mo | RCR only | 30.0 | 7.0 | 68.1 | 6.8 | 2.6 | 137 | 43 |
| Biceps tenodesis | 29.7 | 7.5 | 66.2 | 6.6 | 2.4 | 140 | 44 | |
| P value | .785 | .170 | .428 | .425 | .477 | .339 | .418 | |
| 6 mo | RCR only | 37.6 | 9.0 | 78.4 | 7.6 | 2.0 | 150 | 49 |
| Biceps tenodesis | 39.2 | 9.6 | 77.7 | 7.9 | 1.9 | 157 | 52 | |
| P value | .134 | .044∗ | .769 | .190 | .715 | <.001∗ | .085 | |
| 1 yr | RCR only | 41.1 | 10.1 | 82.4 | 8.4 | 1.5 | 156 | 50 |
| Biceps tenodesis | 42.4 | 10.2 | 83.2 | 8.6 | 1.6 | 159 | 53 | |
| P value | .293 | .571 | .758 | .584 | .591 | .144 | .180 |
Significant difference.
Figure 1.
Graphical depiction of mean outcomes during recovery after rotator cuff repair for patients with and without biceps tenodesis. ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; SST, Simple Shoulder Test. *Significant difference.
Differences in plateaus in maximal recovery were observed for VAS pain, FE, and ER, as earlier plateaus occurred at 6 months for the RCR-BT cohort, whereas the RCR-only cohort reached plateaus at 12 months (Table IV). Biceps tenodesis did not affect the achievement of recovery plateaus for the remainder of the variables, as patients in both cohorts continued to see improvements through 12 months for ASES function, SST, Single Assessment Numeric Evaluation, and VAS function (Fig. 1).
Table IV.
Plateau in maximal improvement for patients who underwent rotator cuff repair only and rotator cuff repair with biceps tenodesis
| Interval | ASES function | SST | SANE | VAS function | VAS pain | FE | ER |
|---|---|---|---|---|---|---|---|
| 6 mo | RCR-BT | RCR-BT | RCR-BT | ||||
| 1 yr | RCR only and RCR-BT | RCR only and RCR-BT | RCR only and RCR-BT | RCR only and RCR-BT | RCR only | RCR only | RCR only∗ |
ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; RCR, rotator cuff tear; RCR-BT, rotator cuff tear with biceps tenodesis; SST, Simple Shoulder Test; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; FE, forward elevation; ER, external rotation.
No true plateau as there was no significant improvement from the preoperative value.
Speed of recovery was not influenced by biceps tenodesis. At 3 months, 79% of improvement in pain and 42%-49% of functional improvement was achieved in the RCR-BT group. Comparably, the RCR-only group achieved a 73% pain improvement and 36%-57% improvement in function at 3 months (Table V).
Table V.
Speed of recovery for patients who underwent rotator cuff repair only and rotator cuff repair with biceps tenodesis
| Procedure | Interval | ASES function, % | SST, % | SANE, % | VAS function, % | VAS pain, % | FE, % | ER, % |
|---|---|---|---|---|---|---|---|---|
| RCR only | 3 mo | 36 | 39 | 61 | 57 | 73 | 17 | —∗ |
| 6 mo | 80 | 78 | 89 | 78 | 88 | 74 | 80† | |
| 1 yr | 100 | 100 | 100 | 100 | 100 | 100 | 100† | |
| Biceps tenodesis | 3 mo | 42 | 48 | 57 | 49 | 79 | 31 | —∗ |
| 6 mo | 85 | 88 | 86 | 82 | 92 | 93 | 85† | |
| 1 yr | 100 | 100 | 100 | 100 | 100 | 100 | 100† |
ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; RCR, rotator cuff tear; RCR-BT, rotator cuff tear with biceps tenodesis; SST, Simple Shoulder Test; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale; FE, forward elevation; ER, external rotation.
ER decreased compared to preoperative value and thus is excluded.
Speed of recovery (% improvement) based on 3-month to 1-year improvement.
Discussion
Patients undergoing arthroscopic rotator cuff repair (RCR) often require a concomitant biceps tenodesis (RCR-BT) as a result of significant tearing and/or instability of the long head of the biceps (LHB) tendon. However, the impact of the additional biceps tenodesis on the recovery process is not well established. Performing a biceps tenodesis may create additional pain-generating morbidity, which has the potential to impact recovery negatively. It has previously been established that arthroscopic RCR recovery plateaus at 1 year postoperatively11; however, no study has assessed the influence of biceps tenodesis on this recovery process. In the current study, speed of recovery was not influenced by biceps tenodesis. However, patients with RCR-BT reached an earlier plateau for pain and motion compared to patients with RCR-only. Results of this study suggest that the plateau in maximal improvement for pain and motion occurs earlier when biceps tenodesis is performed, and these patients achieve slightly higher SST scores and greater shoulder elevation at 6 months. One may speculate as to why patients who required biceps tenodesis were found to have slightly improved function and pain scores at 6 months. One possibility is that during rotator cuff repair with a retained biceps tendon, inaccurate reduction of the supraspinatus can create a stenotic effect on the biceps tendon as it transitions out of the biceps groove. Similar to what can occur with an “hour-glass” biceps, the rotator cuff repair can impair the natural kinematics of the LHB tendon during the recovery. This can potentially result in pain and limitation in shoulder elevation and motion. Although this aspect cannot be confirmed in this study, further investigation into the impact of a rotator cuff repair on biceps kinematics would help clarify this theory. With 1-year results being no different between the 2 groups, it is likely that this effect diminishes over time.
Although the functional role of LHB is poorly understood, LHB is recognized as a clear pain generator in patients with RCT.3,4 In the setting of an irreparable rotator cuff tear, Boileau et al3 demonstrated significant postoperative improvements in Constant pain scores and active anterior elevation following biceps tenodesis or tenotomy. When present with a rotator cuff tear, Ahrens and Boileau2 suggested performing a tenotomy or tenodesis for all cases of rotator cuff repair regardless of the presence of biceps pathology. Although subsequent series focused recommendations on either biceps tenotomy or tenodesis for patients with identifiable biceps tendon pathology,10,12,23 the results of the current study could be misinterpreted in support of routine simultaneous biceps tenodesis given the earlier improvements in recovery observed with concomitant tenodesis. However, to support this recommendation, a comparison would need to be made among patients with rotator cuff repairs and normal biceps tendons treated with or without simultaneous biceps tenodesis, which was not the basis of this study.
For patients undergoing RCR, management of biceps tendon pathology has been shown to result in improved PROMs.8,13 The current study similarly demonstrated positive improvements when a biceps tenodesis was necessary. Overall, these patients achieved 90% improvement in pain and forward elevation by 6 months and demonstrated a plateau in maximal recovery for VAS pain, FE, and ER 6 months earlier than the RCR-only group. However, the speed of recovery was no different.
Long-term studies have demonstrated improvements in outcome following RCR with adjuvant biceps procedures. In a retrospective, multicenter study of 249 patients at 10 years postoperatively, Godenèche et al8 demonstrated equivalent Constant scores in patients with normal biceps who underwent RCR and those with pathologic biceps tendons who were treated with RCR and simultaneous biceps tenodesis or tenotomy. Conversely, in a retrospective review of 80 patients who underwent isolated RCR compared to RCR with either biceps tenotomy or tenodesis, Watson et al20 showed that patients who underwent concomitant biceps procedure had lower baseline ASES scores but greater overall improvement 1 year postoperatively in ASES, VAS, and Western Ontario Rotator Cuff index scores.
This study is not without limitations. Although significant differences were observed in the time to plateau in maximal recovery, the clinical significance of this difference may not have a dramatic implication. Furthermore, although 535 patients were included, the fragility of the observations may change with an even larger series of patients. Finally, although there were similar distributions of patient age and sex between the cohorts, other comorbidities that influence the speed of recovery were not considered in this study. Nevertheless, this is the first study to evaluate the impact biceps tenodesis has on the speed of recovery at various time intervals following RCR.
Conclusion
Patients requiring RCR with simultaneous biceps tenodesis have lower baseline ASES Function Scores, and earlier postoperative plateaus in pain relief and motion improvement following surgery. Nonetheless, speed of recovery was similar at all time points among patients undergoing RCR-Only and RCR-BT.
Disclaimer
Jonathan Levy is a paid consultant for DJO Orthopaedics and Globus Medical. He receives royalties from DJO Orthopaedics and Innomed. No Federal funds or outside sponsorship helped fund this study. All the other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
This study received Exemption status for institutional review board approval per CFR 46.101(b)(4) on 2/18/2016.
References
- 1.Abrams G.D., Gupta A.K., Hussey K.E., Tetteh E.S., Karas V., Bach B.R. Arthroscopic repair of full-thickness rotator cuff tears with and without acromioplasty: randomized prospective trial with 2-year follow-up. Am J Sports Med. 2014;42:1296–1303. doi: 10.1177/0363546514529091. [DOI] [PubMed] [Google Scholar]
- 2.Ahrens P.M., Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg Br. 2007;89:1001–1009. doi: 10.1302/0301-620X.89B8.19278. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Baqué F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 4.Burns W.C., Whipple T.L. Anatomic relationships in the shoulder impingement syndrome. Clin Orthop Relat Res. 1993:96–102. [PubMed] [Google Scholar]
- 5.Chahal J., Mall N., MacDonald P.B., Van Thiel G., Cole B.J., Romeo A.A. The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: a systematic review and meta-analysis. Arthroscopy. 2012;28:720–727. doi: 10.1016/j.arthro.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Chen C.-H., Hsu K.-Y., Chen W.-J., Shih C.-H. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma. 2005;58:1189–1193. doi: 10.1097/01.TA.0000170052.84544.34. [DOI] [PubMed] [Google Scholar]
- 7.Desai S.S., Mata H.K. Long head of biceps tendon pathology and results of tenotomy in full-thickness reparable rotator cuff tear. Arthroscopy. 2017;33:1971–1976. doi: 10.1016/j.arthro.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 8.Godenèche A., Kempf J.-F., Nové-Josserand L., Michelet A., Saffarini M., Hannink G. Tenodesis renders better results than tenotomy in repairs of isolated supraspinatus tears with pathologic biceps. J Shoulder Elbow Surg. 2018;27:1939–1945. doi: 10.1016/j.jse.2018.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Jensen A.R., Cha P.S., Devana S.K., Ishmael C., Di Pauli von Treuheim T., D'Oro A. Evaluation of the trends, concomitant procedures, and complications with open and arthroscopic rotator cuff repairs in the Medicare population. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117731310. 2325967117731310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koh K.H., Ahn J.H., Kim S.M., Yoo J.C. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38:1584–1590. doi: 10.1177/0363546510364053. [DOI] [PubMed] [Google Scholar]
- 11.Kurowicki J., Berglund D.D., Momoh E., Disla S., Horn B., Giveans M.R. Speed of recovery after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2017;26:1271–1277. doi: 10.1016/j.jse.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Lee H.-J., Jeong J.-Y., Kim C.-K., Kim Y.-S. Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: a prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg. 2016;25:1107–1114. doi: 10.1016/j.jse.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Leroux T., Chahal J., Wasserstein D., Verma N.N., Romeo A.A. A systematic review and meta-analysis comparing clinical outcomes after concurrent rotator cuff repair and long head biceps tenodesis or tenotomy. Sports Health. 2015;7:303–307. doi: 10.1177/1941738114539627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy J.C. Simultaneous rotator cuff repair and arthroscopic biceps tenodesis using lateral row anchor. Arthrosc Tech. 2012;1:e1–e4. doi: 10.1016/j.eats.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levy J.C., Everding N.G., Gil C.C., Stephens S., Giveans M.R. Speed of recovery after shoulder arthroplasty: a comparison of reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1872–1881. doi: 10.1016/j.jse.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Park Y.B., Koh K.H., Shon M.S., Park Y.E., Yoo J.C. Arthroscopic distal clavicle resection in symptomatic acromioclavicular joint arthritis combined with rotator cuff tear: a prospective randomized trial. Am J Sports Med. 2015;43:985–990. doi: 10.1177/0363546514563911. [DOI] [PubMed] [Google Scholar]
- 17.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990:81–86. [PubMed] [Google Scholar]
- 18.Vellios E.E., Nazemi A.K., Yeranosian M.G., Cohen J.R., Wang J.C., McAllister D.R. Demographic trends in arthroscopic and open biceps tenodesis across the United States. J Shoulder Elbow Surg. 2015;24:e279–e285. doi: 10.1016/j.jse.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Walch G., Edwards T.B., Boulahia A., Nové-Josserand L., Neyton L., Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Watson S.T., Robbins C.B., Bedi A., Carpenter J.E., Gagnier J.J., Miller B.S. Comparison of outcomes 1 year after rotator cuff repair with and without concomitant biceps surgery. Arthroscopy. 2017;33:1928–1936. doi: 10.1016/j.arthro.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 21.Werner B.C., Brockmeier S.F., Gwathmey F.W. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43:570–578. doi: 10.1177/0363546514560155. [DOI] [PubMed] [Google Scholar]
- 22.Yi Y., Lee J.-M., Kwon S.H., Kim J.-W. Arthroscopic proximal versus open subpectoral biceps tenodesis with arthroscopic repair of small- or medium-sized rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2016;24:3772–3778. doi: 10.1007/s00167-015-3641-5. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Q., Zhou J., Ge H., Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:464–469. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]