Abstract
Background
Intraoperative identification of the normal pectoralis major (PM) footprint can be challenging to identify in the acute and chronic settings. The purpose of this study was to revisit the anatomic footprint of the PM tendon and to determine which nearby landmarks can be used to re-create the normal insertion site during anatomic repair or reconstruction.
Methods
Twenty-one fresh-frozen human cadaveric shoulder specimens were used to define the PM tendon width (ie, superior-to-inferior) and to determine the relationship between the superior aspect of the PM insertion and that of the latissimus dorsi (LD) and anterior deltoid (AD) tendons. An attempt was made to identify potential useful bony landmarks that can be used during anatomic repair or reconstruction of the PM tendon.
Results
The mean PM tendon width was 68.8 ± 4.4 mm. The superior margin of the LD insertion was 9.4 ± 5.9 mm above and the AD was 48.4 ± 7.1 mm below the superior margin of the PM tendon insertion, respectively. In 17 of 21 specimens (81%), the superior insertion of the PM tendon attached onto a bony prominence, named the pectoral eminence.
Conclusions
The LD and AD tendon insertions represent reliable soft tissue landmarks for identifying the superior extent of the PM tendon along its bony footprint. The pectoral eminence can also be used as an additional reference point in the majority of cases to facilitate anatomic restoration of the pectoralis tendon during repair and reconstruction. Surgeons should be familiar with the proximity of nearby neurovascular structures when performing PM repairs.
Keywords: Pectoralis major, tendon, footprint, anatomy, pectoral eminence, rupture, repair, reconstruction
The pectoralis major (PM) is a complex, multipennate muscle of the anterior shoulder girdle that is responsible for adduction, internal rotation, and flexion of the humerus.1,8,39 The musculotendinous anatomy is composed of 2 divisions—an anterior clavicular division and a posterior sternal-abdominal division that coalesce to form a bilaminar tendon before inserting onto the humerus.10 Tears of the PM tendon occur predominantly in young active men (between 20 and 40 years of age) following indirect trauma when a maximal force is applied, typically when the PM is eccentrically contracting.5,8,24
Surgical repair of PM tendon tears remains an effective treatment option in young, active adults with a high rate of return to sport and work40; however, a recent report has demonstrated that only 50% of patients are able to return to the same preoperative intensity of sport.26 Several accepted methods for fixation of the avulsed tendon to its humeral insertion exist.11 Intraoperative identification of the normal PM anatomic footprint (ie, superior-to-inferior dimension) can be challenging to identify in both the acute and chronic settings. Only 2 studies to date have reported on nearby landmarks that can be used intraoperatively to achieve anatomic repair of the PM tendon3,6; however, concern remains regarding patient-to-patient variability and intraoperative accessibility of such bony and soft tissue reference points in the anterior shoulder during open repair and reconstruction of the PM tendon.
The purpose of this study was to revisit the anatomic footprint (ie, superior-to-inferior dimension) of the pectoralis major tendon on the humerus and to determine which nearby anatomic landmarks (soft tissue and/or bony) can be used with the least amount of variability to determine the upper margin of the normal PM footprint during anatomic repair or reconstruction. We also aimed to determine if there was a relationship between patient height and PM tendon insertional anatomy (ie, width). We hypothesized that the latissimus dorsi tendon insertion on the humerus would not be a consistent reference point for establishing the correct upper margin of the pectoralis major tendon footprint based on clinical experience of open shoulder surgery. We also hypothesized that there would be a linear relationship between footprint width and patient height. The secondary objective of this study was to review the existing literature and summarize the dimensions of the PM tendon and anatomic relationships of the PM insertion to nearby musculoskeletal and neurovascular structures.
Materials and methods
Specimen preparation
Twenty-two fresh-frozen upper extremity cadaveric specimens were dissected after approval by the institutional review board. Six specimens were paired (12 shoulders). One specimen was found to have a previous humeral shaft fracture at the level of the deltoid insertion; this specimen was excluded from the analysis, resulting in 21 shoulders for final analysis. Specimens were obtained from and dissections performed at the institution’s Advanced Technical Skills Simulation Laboratory; all specimens were free of surgical dissection in the anatomic area(s) of interest. Each specimen was thawed to room temperature before dissection. Surgical exposure of the PM muscle and tendon and nearby anatomic structures was performed via a standard deltopectoral approach. The position of the humerus relative to the scapula (ie, axial, sagittal, and coronal planes) did not affect the measurements as none of the final measurements taken on the humerus were referenced to the scapula. Study conceptualization and initial methodology was designed by one investigator (A.J.B.) and final methodology was agreed on by both investigators (A.J.B., I.K.Y.L.) prior to starting anatomic dissections. All anatomic dissections (including measurements and digital photographs) were performed by one of the study investigators (A.J.B.).
Data collection
The tendons of the PM, anterior deltoid (AD), and latissimus dorsi (LD) were identified and sharply dissected down to their respective bony insertion on the humerus. The long-head biceps tendon was carefully removed from the bicipital groove, while preserving the tendinous attachments of the LD and PM. The presence of the falciform ligament was variable between specimens and was excluded from measurements (ie, excised before measurements performed). When present, this ligament represents a fibrous expansion of the PM that extends in a superior-oblique orientation along the lateral aspect of the bicipital groove and can easily be differentiated from the thick tendinous insertion of the PM directed perpendicular to the humerus (Fig. 1). The width (ie, superior-to-inferior) dimension of the PM tendon insertion on the humerus was first identified and measured; meticulous dissection was required adjacent to the proximal and distal PM insertion due to the intricate relationship with the adjacent LD and AD, respectively (Fig. 2). Next, the superior aspect of the LD and AD were identified. A line perpendicular to the axis of the humerus intersecting the superior margin of the LD and AD was marked as previously described.6 The relationship between the superior aspect of the PM insertion and that of the LD and AD was measured (Fig. 3). The relationship between the superior margin of the PM tendon and lower border of the lesser tuberosity (LT) and to the tip of the coracoid process were assessed as potential useful bony landmarks (ie, consistent reference points) for assisting anatomic repair of the PM tendon. All measurements were performed using digital calipers and recorded in millimeters (Absolute Digimatic Caliper Series 500; Mitutoyo, Aurora, IL, USA). The measurements were performed twice, and the average of the 2 measurements used as the final measurement.
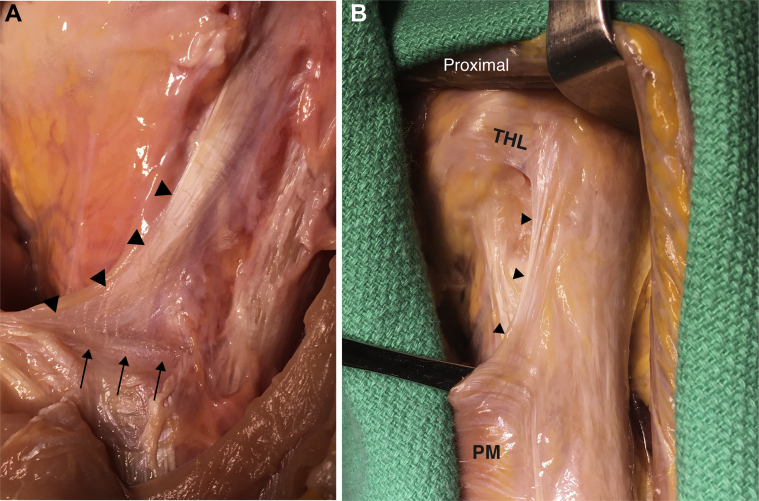
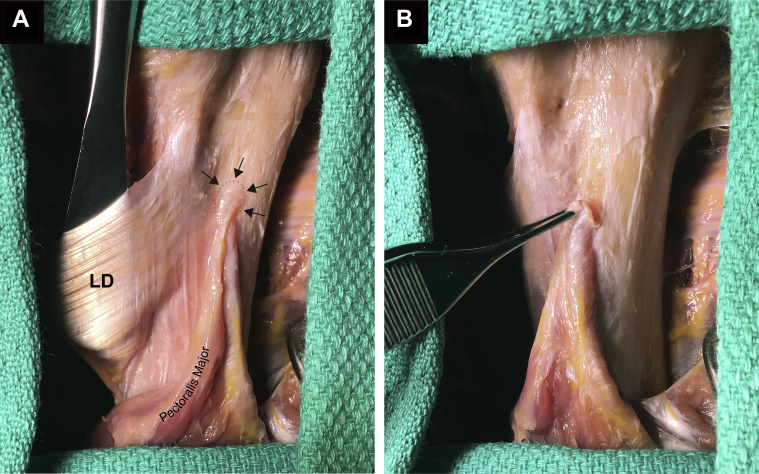
Figure 1.
The falciform ligament is demonstrated in 2 different left shoulder specimens (►). (A) The pectoralis major tendon (PM) can be differentiated from the falciform ligament as a thick tendinous expansion spanning in the transverse plane to the humeral footprint (→). (B) The superior-oblique orientation of the falciform ligament is visualized and easily differentiated from the PM. The intimate relationship with the transverse humeral ligament (THL) and bicipital tunnel is appreciated.
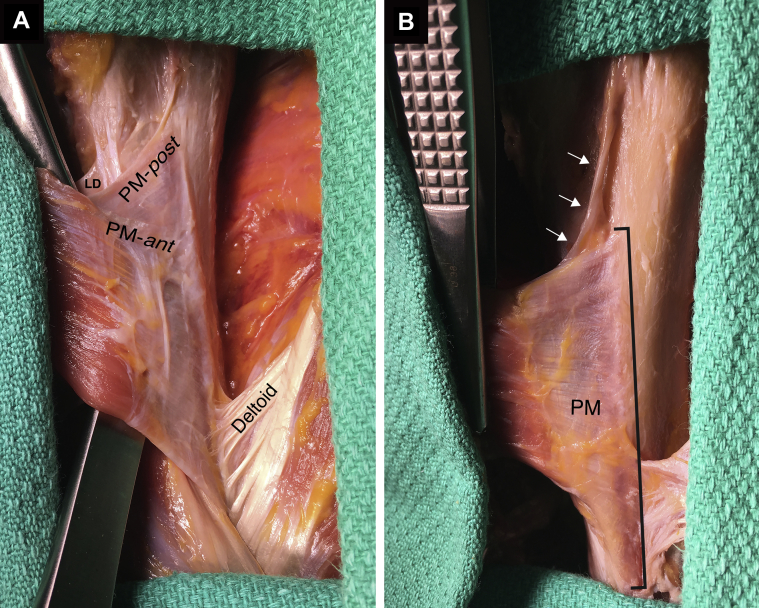
Figure 2.
Relationship between the pectoralis major (PM), latissimus dorsi (LD), and anterior deltoid tendons. (A) Left shoulder specimen demonstrating one of the few examples encountered of a clearly defined bilaminar PM tendon, represented by the anterior (PM-ant) and posterior (PM-post) laminae. The posterior lamina is observed extending in an oblique fashion to the humeral insertion; a less well-defined falciform ligament is observed immediately superior to its upper margin. This was also one of the few examples demonstrating the close relationship of the superior aspect of both the PM and LD tendons inserting onto the humerus. (B) A different left shoulder specimen demonstrating the broad PM tendon footprint on the humerus. The superior-oblique falciform ligament is present extending above the upper border of the PM (→).
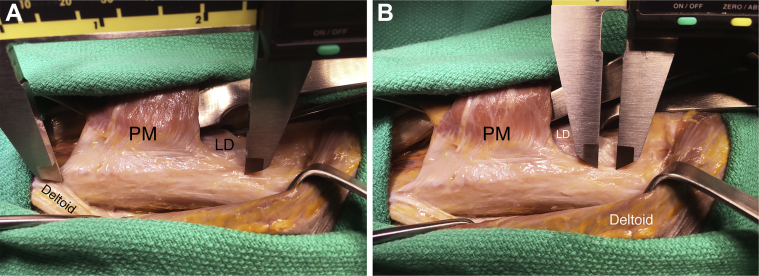
Figure 3.
Measurements obtained from a left shoulder specimen between the pectoralis major tendon (PM) and the anterior deltoid (A) and the latissimus dorsi (LD) tendons (B).
For the secondary objective of the study, a literature search was conducted using the MEDLINE database. All relevant clinical and basic science studies in the English language were reviewed and considered for inclusion. Studies were included if clear descriptions of the PM footprint were provided and/or if the anatomic relationship between the PM insertion and nearby musculoskeletal and neurovascular structures was described. Studies were excluded if they met the following criteria: (1) imaging studies of the pectoralis major tendon insertion without anatomic correlation; (2) reviews, expert opinions, and technique articles without anatomic data; and (3) conference abstracts and gray literature. The reference lists of all included studies were cross-referenced to capture additional studies missed by the initial literature search.
Data analysis
For the purpose of statistical analysis, each matched pair was considered an independent specimen. Descriptive statistical analysis was performed to include mean, range, and standard deviation. The relationship between donor height (in inches) and tendon width (mm) was summarized in a scatterplot, as well as with Pearson correlations. Because of the small number of paired specimens (n=6), statistical analysis was not performed to assess for side-to-side differences in PM dimensions. Previous studies reporting the PM insertional anatomy and the relationships to nearby musculoskeletal and neurovascular structures were summarized in table format. When possible, values were calculated as weighted means.
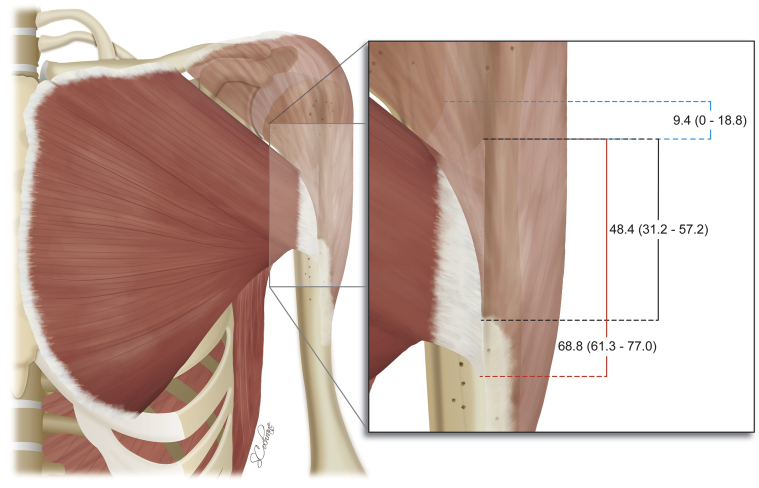
Results
The dissections were carried out on 11 male and 4 female cadavers with an average age of 75.8 years (range, 54-94 years). There were 8 right and 13 left shoulder specimens. The mean proximal-to-distal width of the PM tendon (ie, at the humeral insertion) was 68.8 ± 4.4 mm. The mean distance from the superior margin of the LD insertion to the superior aspect of the PM tendon insertion was 9.4 ± 5.9 mm. The mean distance between the superior margin of the AD insertion to the superior aspect of the PM tendon insertion was 48.4 ± 7.1 mm (Table I, Fig. 4).
Table I.
Pectoralis major tendon measurements and relationships
| Variable | N | Mean ± SD | Minimum | Maximum |
|---|---|---|---|---|
| Donor height (ht), in. | 21 | 67.2 ± 3.8 | 59 | 72 |
| Footprint width (w), mm | 21 | 68.8 ± 4.4 | 61.3 | 77.0 |
| Distance to anterior deltoid insertion (ad), mm | 21 | 48.4 ± 7.1 | 31.2 | 57.2 |
| Distance to latissimus dorsi insertion (ld), mm | 21 | 9.4 ± 5.9 | 0 | 18.8 |
SD, standard deviation; w, width of pectoralis major tendon insertion (ie, superior-to-inferior dimension); ad, distance between the superior margin of the pectoralis major tendon insertion and the anterior deltoid tendon insertion; ld, distance between the superior margin of the pectoralis major tendon insertion and the superior margin of the latissimus tendon insertion.
Figure 4.
Illustration summarizing the mean (range) pectoralis tendon width and measurements between the pectoralis major, latissimus dorsi, and anterior deltoid tendons.
Bony landmarks that may be identified during open repair or reconstruction of the PM tendon were assessed in the suprapectoral region, including the LT and tip of the coracoid process. The geometry of the lesser tuberosity made it challenging to identify one consistent region of the LT to use as a reference point (ie, central apex or lower border of the LT), likely a result of the overlying thick tendinous and muscular portions of the subscapularis inserting onto the LT. The coracoid process was similarly found to be an unreliable bony landmark based on the position of the scapula relative to the humerus and the foreseeable difficulty in reproducing this position in the laboratory setting and intraoperatively.
During the assessment of nearby bony landmarks, it became apparent that the superior thick tendinous insertion of the PM tendon attached onto a bony prominence in nearly all specimens (Figs. 5 and 6). The dimensions of this prominence were not formally measured. Although the anterior-to-posterior (ie, height) dimension of this prominence seemed variable between specimens, it could be palpated with a gloved finger while the tendinous attachment was intact in nearly all specimens. In a smaller number of specimens, this prominence represented the most superior aspect of a bony ridge that extended inferiorly, nearly the entire width of the PM tendon insertional footprint, analogous to the deltoid tuberosity (Fig. 6); this ridge is often referred to as the lateral lip of the bicipital groove. We have referred to the former bony prominence as the pectoral eminence and the bony ridge extending below this eminence as the pectoral tuberosity; to our knowledge, this eminence has not been previously described in the literature.
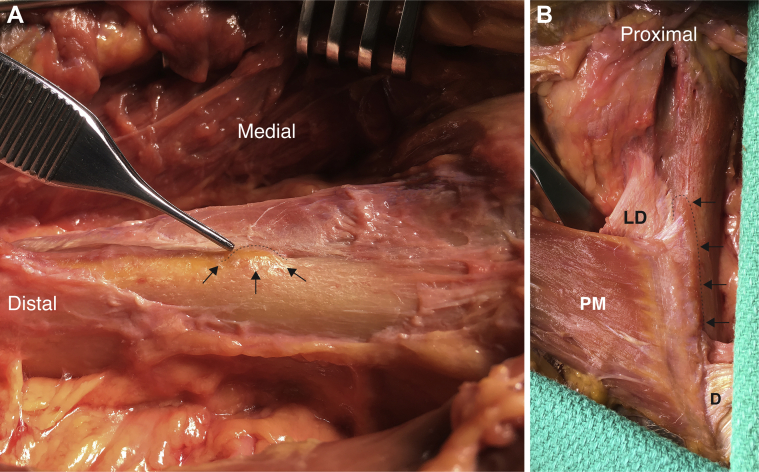
Figure 5.
(A) Left shoulder specimen demonstrating the relationship between the pectoralis major and latissimus dorsi (LD) tendons. The pectoral eminence is clearly demonstrated (→). (B) Superior aspect of pectoralis major tendon held in forceps adjacent to pectoral eminence.
Figure 6.
(A) Left shoulder specimen demonstrating the pectoral eminence (→). (B) A different left shoulder specimen revealing the relationship between the pectoralis major (PM), latissimus dorsi (LD), and anterior deltoid (D) tendons. Above the anterior deltoid tendon insertion on the humerus, the PM tendon is shown inserting into a visible and palpable bony ridge along the lateral lip of the bicipital groove (ie, pectoral tuberosity), continuous with the pectoral eminence at the most superior PM tendon insertion (→).
The relationship between donor height and PM tendon width demonstrated no discernible relationship, with a correlation of 0.13 (P value .58). In addition, a simple linear regression confirmed these findings (coefficient 0.14, P value .58). In summary, a relationship between these 2 variables did not appear evident; however, with only 15 unique patient proportions for analysis (ie, 6 matched pairs used within the sample of 21 specimens), this relationship likely represents a trend and requires further investigation.
Pectoralis major tendon dimensions previously reported in the literature are summarized in Table II. The mean (ie, weighted mean) PM tendon width (ie, superior-to-inferior) was 6.25 cm,2, 20, 21, 22, 25, 28, 3, 31, 39, 4,6,9,10,12,16, 17, 18,20, 21, 22,25,28,31,39 mean tendon length (ie, medial-to-lateral) was 2.22 cm,2,9,10,18,21,25,39 and mean tendon thickness (ie, anterior-to-posterior) was 0.16 cm (Table II).3,4,6,10,18 The anatomic relationships between the PM tendon insertion and nearby anatomic structures (ie, musculoskeletal and neurovascular) are summarized in Tables III and IV.
Table II.
Summary of pectoralis major tendon dimensions previously reported in the literature
| Study | No. | Age (range) | M/F | R/L | Method of measurement | Tendon width (superior-to-inferior), cm | Tendon length (medial-to-lateral), cm | Tendon thickness (anterior-to-posterior), cm | Insertional surface area, mm2 |
|---|---|---|---|---|---|---|---|---|---|
| Ashley (1952)2 | 60 | — | — | — | — | — | 0.6-1.9 | — | — |
| Chaffaï and Mansat (1988)4 | 7 | — | — | — | — | 4.4 ±0.3 (4.1-4.9)∗ | — | 0.1-0.2† | — |
| Kretzler and Richardson (1989)21 | — | — | — | — | — | — | 1.0 (AL) 2.5 (PL) |
— | — |
| Wolfe et al (1992)39 | 2 | 60 (58-63) | 2:0 | — | — | 5.0 | 0.5 | — | — |
| Lee et al (2000)25 | 6 | — | 1:2 | 3:3 | MRI correlation | 5.0 (4-6) | 1.0 (0.5-1.5) | — | — |
| Klepps et al (2001)20 | 20 | 64 (48- 82) | 5:5 | 10:10 | Ruler | 5.7 ±0.5 (4.8-6.6)† | — | — | — |
| Jennings et al (2007)18 | 21 | 54 (19-96) | 11:10 | — | Calipers | 4.7 (2.4-6.3) (AL) 4.3 (2.4-6.4) (PL) |
1.5 (0.9-2.2) (AL) 3.7 (2.3-5.1) (PL) |
0.1 (0.1-0.2) (AL) 0.1 (0.1-0.2) (PL) |
|
| Fung et al (2009)10 | 11 | 78 (54-98) | 6:5 | — | 3D digital modeling | 6.6 ±1.1 (5.2-8.2) (AL) 7.7 ±1.4 (6.5-9.7) (PL) |
5.4 ±0.6 (AL) 5.4 ±0.7 (PL) |
0.2 ±0.05 (0.1-0.3) (AL) 0.2 ±0.03 (0.2-0.3) (PL) |
— |
| Carey and Owens (2010)3 | 12 | — | — | 6:6 | Digital calipers | 7.2 ±1.2 (5.1-8.7) | — | 0.1 ±0.02 (0.1-0.2) | — |
| Jarrett et al (2011)17 | 12 | 84 (69-98) | 3:9 | 10:2 | Ruler | 5.3 (5.0-5.7)† | — | — | — |
| Figueiredo et al (2013)9 | 20 | 65.4 (51-75) | 5:5 | 10:10 | Calipers | 8.8 ±7.1 (7.0-9.0) | 0.6 ±0.07 (0.5-0.7) | — | — |
| LaFrance et al (2013)22 | 10 | 67 (43-88) | 9:1 | — | Digital calipers | 7.7 ±1.2 | — | — | — |
| Nossov et al (2016)31 | 20 | 76.9 (61-93) | 15:5 | 9:11 | Ruler | 5.4 | — | — | — |
| Moatshe et al (2018)28 | 10 | 52 (33-64) | 5:5 | 5:5 | Coordinate measuring device | 4.6 (3.7-5.4)† | — | — | 148.4 (126.9-169.8)† |
| Dannenbaum et al (2018)6 | 12 | 60 ± 7 | 7:5 | — | Ruler | 7.3 ±1.0 (6.0-9.5) | — | 0.3 ±0.05 cm (0.25-0.4) | — |
| Haladaj et al (2019)12 | 80 | 69.3 (48-90) | 22:18 | 40:40 | Digital calipers | 6.5 ±1.0 (4.4-8.3) | — | — | — |
| Jagiasi et al (2019)16 | 10 | 50 (40-60) | 5:0 | 5:5 | Calipers | 4.6 ±0.5 (4.2-5.6) | — | — | — |
M, male; F, female; R, right; L, left; MRI, magnetic resonance imaging; AL, anterior lamina; PL, posterior lamina; 3D, 3-dimensional.
Clavicular portion of the pectoralis major tendon.
95% confidence interval.
Table III.
Summary of previously reported anatomic relationships (musculoskeletal) with the pectoralis major tendon
| Anatomic landmark | Study | No. of specimens | Method of measurement | Referenced to superior PMT insertion on humerus, cm |
|---|---|---|---|---|
| Bony structures | ||||
| Superior humeral head | Murachovsky et al (2006)29 | 40 | Calipers | 5.6 ± 0.5 (5.0-7.0) above PMT |
| Torrens et al (2008)38 | 20 | CT correlation | 5.6 (5.3-6.0) above PMT | |
| Hasan et al (2009)13 | 38 | Digital calipers | 5.8 ± 0.6 above PMT | |
| Ponce et al (2013)32 | 22 | Calipers | 5.6 ± 0.5 (4.3-6.2) above PMT | |
| Figueiredo et al (2013)9 | 20 | Calipers | 5.9 ± 0.3 (5.5-6.4) above PMT | |
| Articular margin of HH | Dannenbaum et al (2018)6 | 12 | Surgical ruler | 4.1 ± 0.9 above PMT |
| Greater tuberosity∗ | Carey and Owens (2010)3 | 12 | Digital calipers | 4.2 ± 0.9 (3.1-5.0) above PMT |
| Haladaj et al (2019)12 | 80 | Digital calipers | 5.2 ± 0.8 (3.8-6.5) above PMT | |
| Jagiasi et al (2019)16 | 10 | Calipers | 4.9 ± 0.4 (43-55) above PMT | |
| Center of greater tuberosity to center of PMT | Moatshe et al (2018)28 | 10 | Coordinate measuring device | 6.1 (95% CI, 5.6-6.6) above PMT |
| Center of lesser tuberosity to center of PMT | Moatshe et al (2018)28 | 10 | Coordinate measuring device | 6.2 (95% CI, 5.5-6.8) above PMT |
| Lateral epicondyle of the distal humerus | Hasan et al (2009)13 | 38 | Digital caliper | 24.9 ± 1.8 below PMT |
| Muscle-tendon structures | ||||
| Origin of LHB tendon | Hussain et al (2015)15 | 43 | Ruler | 8.1 ± 1.0 (6.3-10.4) above the PMT |
| MTJ of LHB tendon | Jarrett et al (2011)17 | 12 | — | 2.2 (95% CI, 1.2-3.1) below PMT |
| Denard et al (2012)7 | 21 | Digital calipers | 2.5 below PMT | |
| LaFrance et al (2013)22 | 10 | Digital calipers | 3.2 ± 1.4 below PMT | |
| Superior LD tendon insertion | Dannenbaum et al (2018)6 | 12 | Surgical ruler | <1 mm proximal or distal to PMT |
| Center of LD insertion to center of PMT | Moatshe et al (2018)28 | 10 | Coordinate measuring device | 1.8 (95% CI, 1.2-2.3) above PMT |
| Anterior deltoid insertion | Klepps et al (2004)19 | 36 | Ruler | 4.7 below PMT |
| Center of deltoid insertion to center of PMT | Moatshe et al (2018)28 | 10 | Coordinate measuring device | 4.4 below PMT (95% CI, 3.8-5.0) |
PMT, pectoralis major tendon; CT, computed tomography; HH, humeral head; CI, confidence interval; LHB, long head biceps; MTJ, myotendinous junction; LD, latissimus dorsi.
Superomedial aspect of the greater tuberosity to the superior border of PMT.
Table IV.
Summary of previously reported anatomic relationships (neurovascular) with the pectoralis major muscle and tendon
| Anatomic landmark | Study | No. of specimens | Method of measurement | Referenced to superior PMT insertion on humerus, cm |
|---|---|---|---|---|
| Neural structures | ||||
| Pectoral nerves | Klepps et al (2001)20 | 20 | Ruler | MPN: • 11.9 ± 2.0 (95% CI, 8.6-15.3) from the lateral humeral insertion • 2.6 ± 0.8 (95% CI, 1.2-2.8) from the inferior border of the PMT LPN: • 12.5 ± 1.8 (95% CI, 9.5-15.5) from the lateral humeral insertion |
| Macchi et al (2007)27 | 16 | Calipers | MPN: • Pierces through the pectoralis minor 10.3 ± 1.9 from the margin of the sternum, close to the midclavicular line at the level of the third intercostal space |
|
| Jennings et al (2007)18 | 21 | Calipers | MPN: • Enters the inferior sternal segment 1.4 (0.9-1.8) distal to the segmental split, 9.3 (8.6-9.9) from the humeral PMT insertion |
|
| Sefa Özel et al (2011)∗,35 | 20 | Ruler | LPN: • Point where the NV bundle enters the PM muscle: intersection of 2 lines crossing 2.8 ± 0.3 (2.5-3.5) inferior to the medial one-third clavicle and 8.1 ± 1.1 (7.0-11.0) lateral to the midsternal line |
|
| Prasad and Kuppasad (2014)34 | 50 | Calipers | MPN: • Pierces the deep surface of the PM muscle 10.1 ± 0.4 (8.8-10.8) from the lateral margin of the sternum LPN: • Pierces the deep surface of the PM muscle 8.6 ± 1.0 (5.8-10.2) from the lateral margin of the sternum |
|
| Axillary nerve (anterior Br.) | Lancaster et al (2014)23 | 12 | CT correlation | 0.2 ± 0.3 (95% CI, 0-0.4) “vertical distance” to the PMT |
| Shiu et al (2017)36 | 30 | Digital calipers | 0.3 (range, 0-0.8 mm) below the PMT | |
| Moatshe et al (2018)†,28 | 10 | Coordinate measuring device | 0.9 (95% CI, 0.5-1.4) | |
| Vascular structures | ||||
| Lateral thoracic artery | Jennings et al (2007)18 | 21 | Calipers | Enters the inferior sternal segment distal to the segmental split at 8.5 (7.0-10.4) from the humeral PMT insertion |
| Posterior circumflex humeral artery | Smith et al (2016)37 | 100 patients (clinical study) | Sterile ruler | • 0.5 ± 0.3 (range, 0-1.2) below the PMT in 30% of cases “above the PMT insertion” in 45% of cases |
| Vascular Br. of anterior humeral circumflex vessels | Neviaser et al (2018)30 | 11 | Digital calipers | 1.5 ± 0.4 above the PMT |
PMT, pectoralis major tendon; MPN, medial pectoral nerve; CI, confidence interval; LPN, lateral pectoral nerve; NV, neurovascular; PM, pectoralis major; CT, computed tomography; Br., branch.
Point of intersection between the vertical line at the junction between the medial one-third and lateral two-thirds of the clavicle and the horizontal line perpendicular to the midsternal line at the inferiormost level of the jugular notch.
Distance between the lower border of the PMT and the axillary nerve.
Discussion
The purpose of this anatomic study was to identify reliable soft tissue and bony landmarks for re-creating the footprint of the pectoralis major tendon during open anatomic repair or reconstruction, following full-thickness (partial- and full-width) acute and chronic tears. Our results demonstrate that, on average, the PM tendon footprint width is approximately 7 cm and is 5 cm above the anterior deltoid and 1 cm below the latissimus dorsi tendon insertions. We have identified a consistent bony eminence at the superior margin of the PM tendon insertion. Both the soft tissue and bony landmarks described in this study can be used to estimate the superior margin of the anatomic footprint of the PM tendon during repair or reconstruction.
In 2012, a systematic review of 365 reported cases of PM injury revealed that 45.2% (165 of 365 cases) occurred at the tendon insertion; 113 (68.5%) of such injuries were complete (ie, involving both the clavicular and sternal heads).8 When this tear pattern is encountered in both the acute and chronic settings, reconstituting the proper length-tension relationship of the PM requires reinsertion of the tendon to the anatomic footprint. Therefore, knowledge of the footprint dimensions (ie, superior-to-inferior dimension along the lateral lip of the bicipital groove) and relationship to nearby structures is crucial for anatomic repair and reconstruction of the PM tendon.
We are aware of 17 previous studies examining the PM insertional anatomy (Table II). Among these studies, the weighted average footprint width (ie, superior-to-inferior dimension) was 6.3 cm (range, 4.4-8.8 cm).2, 20, 21, 22, 25, 28, 3, 31, 39, 4,6,9,10,12,16, 17, 18,20, 21, 22,25,28,31,39 These findings correlate well with our data. Although not formally assessed in the current study, the PM tendon thickness (ie, anterior-to-posterior dimension) has been found to be approximately 1-3 mm.3,4,6,10,18 The largest variation of measurement between studies relates to the tendon length (medial-to-lateral dimension), ranges between 0.6 and 5.4 cm (Table II).2,9,10,18,21,25,39 Only 1 study has measured the PM tendon footprint area (Table II).28 Also not formally assessed in the current study, fusion of the bilaminar PM tendon before insertion onto the humerus was found to be variable between specimens (Fig. 2).
To our knowledge, only 2 previous studies have attempted to identify consistent anatomic landmarks that can be used intraoperatively to achieve anatomic repair of the PM tendon. Using 12 cadaveric shoulders (6 matched pairs), Carey and Owens used the superomedial corner of the greater tuberosity as a reference point to determine the location of the superior PM tendon insertion along the lateral lip of the bicipital groove.3 These authors found that the superior PM tendon insertion was 42.2 ± 8.5 mm below the superomedial corner of the greater tuberosity. Although easily identified in the laboratory setting, this bony landmark may not be readily accessible intraoperatively when using an axillary or modified deltopectoral incision (ie, lower two-thirds of the standard deltopectoral incision) to address PM tendon pathology. Dannenbaum et al6 evaluated 12 cadaveric shoulders to define the anatomic relationships between the PM insertion and the articular margin of the humeral head and the LD tendon insertion. These authors revealed that, on average, the superior margin of the PM tendon was within 1 mm of the LD insertion and 41.2 mm from the articular margin of the humeral head. However, in the current anatomic study, only 4 of 21 shoulders (19.0%) revealed a similar relationship between the superior margins of the PM and LD tendon insertions (ie, top of the PM tendon insertion within 2 mm of the LD insertion). In addition, we did not find that the articular margin of the humeral head would be a reliable intraoperative landmark during repair or reconstruction of the PM tendon and similarly found that identification of the superior aspect of the LD tendon would require unnecessary surgical dissection during repair or reconstruction of the PM tendon. In an evaluation of the deltoid insertion in 36 cadaveric shoulders, Klepps et al19 found that the PM tendon inserted onto the humerus a mean of 4.7 cm proximal to the insertion of the deltoid, which was similar to the measurements obtained in the current study (48 mm). We therefore recommend considering this landmark to define the superior margin of the PM tendon footprint along the lateral lip of the bicipital groove.
Another aim of the current study was to define a consistent bony landmark that could be used to consistently define the superior margin of the PM footprint during repair and reconstruction procedures. Although we did not find that the LT or coracoid tip were useful bony landmarks, we did discover that in the majority of specimens (ie, greater than 80%), a bony prominence was present and palpable with a gloved finger at the most superior margin of the intact PM tendon insertion. We have referred to this prominence as the pectoral eminence. This eminence, along with the AD and LD (if readily accessible) tendon insertions, can be used to help determine the upper margin of the PM tendon footprint during repair or reconstruction.
Our last aim of the study was to provide a summary of musculoskeletal3,6,7,9,12,13,15, 16, 17,19,22,28,29,32,38 and neurovascular14,18,20,23,27,28,30,33, 34, 35, 36, 37 relationships to the PM tendon. Of the musculoskeletal landmarks, an additional intraoperative landmark for consideration during repair or reconstruction of the PM tendon includes the musculotendinous junction of the biceps brachii (weighted mean, 2.5 cm below the top of the PM tendon) (Table III).7,17,22 The neurovascular structures summarized in Table IV do not provide a distinct intraoperative landmark during repair or reconstruction of the PM tendon, but rather provide knowledge of the “safe zone” when performing these procedures. Specifically, understanding the proximity of the axillary nerve as the most vulnerable structure is critical to safely repair or reconstruct the PM tendon (Table IV).23,28,36
This study is subject to several limitations, commonly observed in cadaveric studies. Shoulder dissections and measurements were performed on a relatively low number of shoulder specimens and by 1 surgeon only, which could affect the generalizability of the results. However, the consistency of measurements between this study and most of the previously published studies on PM tendon insertional anatomy represents substantial strengths of this study. Another limitation includes the low number of female specimens, which prevented subgroup analysis and our ability to generalize the results to the female population; however, injury to PM tendon occurs most often in males and therefore represents a small limitation of the current study. Anatomic differences that may be based on ethnicity were also not assessed in this study. Additional strengths of our study are the identification of soft tissue and bony anatomic landmarks that can be used to reliably define the PM tendon insertion. The measurements recorded in this study were not influenced by specimen position, which is a common limitation in other studies that use forequarter cadaveric specimens. Lastly, further clinical studies are required: (1) to assess the clinical outcomes comparing anatomic and nonanatomic repair or reconstruction of the PM tendon; (2) to better define the pectoral eminence and lateral lip of the bicipital groove (ie, pectoral tuberosity) and its relationship with the PM insertion and the deltoid tuberosity inferiorly; and (3) to further elucidate whether a relationship exists between patient height and PM tendon width using a larger sample of specimens.
Conclusion
The pectoralis major tendon has a broad insertion along the lateral lip of the bicipital groove (tendon width, 68.8 ± 4.4 mm). The width of the PM tendon insertion does not seem to be influenced by patient height; however, this requires further investigation. The latissimus dorsi and anterior deltoid tendon insertions represent reliable landmarks for identifying the superior extent of the pectoralis tendon along its bony footprint, inserting 9.4 mm below and 48.4 mm above these landmarks, respectively. When present, the pectoral eminence can also be used as an additional reference point to facilitate anatomic restoration of the pectoralis tendon during repair and reconstruction. Surgeons should be familiar with the proximity of nearby neurovascular structures when performing PM repairs.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors thank Sandy Cochrane, Illustrator, Cumming School of Medicine (University of Calgary), for drawing Fig. 4. The authors also wish to thank all staff at the Advanced Technical Skills Simulation Laboratory (Cumming School of Medicine, University of Calgary) for their ongoing support during this study. The authors received funding support from the Calgary Surgical Research Development Fund (CSRDF) for this study (Project ID: RT756782).
Footnotes
Institutional Review Board approval was granted from the University of Calgary Research Ethics Board (REB18-1929).
References
- 1.Ackland D.C., Pak P., Richardson M., Pandy M.G. Moment arms of the muscles crossing the anatomical shoulder. J Anat. 2008;213:383–390. doi: 10.1111/j.1469-7580.2008.00965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashley G.T. The manner of insertion of the pectoralis major muscle in man. Anat Rec. 1952;113:301–307. doi: 10.1002/ar.1091130305. [DOI] [PubMed] [Google Scholar]
- 3.Carey P., Owens B.D. Insertional footprint anatomy of the pectoralis major tendon. Orthopedics. 2010;33:23. doi: 10.3928/01477447-20091124-27. [DOI] [PubMed] [Google Scholar]
- 4.Chaffaï M.A., Mansat M. Anatomic basis for the construction of a musculotendinous flap derived from the pectoralis major muscle. Surg Radiol Anat. 1988;10:273–282. doi: 10.1007/BF02107898. [DOI] [PubMed] [Google Scholar]
- 5.Cordasco F.A., Mahony G.T., Tsouris N., Degen R.M. Pectoralis major tendon tears: functional outcomes and return to sport in a consecutive series of 40 athletes. J Shoulder Elbow Surg. 2017;26:458–463. doi: 10.1016/j.jse.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Dannenbaum J.H., Eckhoff M.D., Galvin J.W., Bean B.K., Wilson D.J., Arrington E.D. Pectoralis major tendon insertion anatomy and description of a novel anatomic reference. J Surg Orthop Adv. 2018;27:39–41. [PubMed] [Google Scholar]
- 7.Denard P.J., Dai X., Hanypsiak B.T., Burkhart S.S. Anatomy of the biceps tendon: implications for restoring physiological length-tension relationship during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28:1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 8.ElMaraghy A.W., Devereaux M.W. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg. 2012;21:412–422. doi: 10.1016/j.jse.2011.04.035. [DOI] [PubMed] [Google Scholar]
- 9.Figueiredo E.A., Terra B.B., Cohen C., Monteiro G.C., de Castro Pochini A., Andreoli C.V. The pectoralis major footprint: an anatomical study. Rev Bras Ortop. 2013;48:519–523. doi: 10.1016/j.rboe.2013.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fung L., Wong B., Ravichandiran K., Agur A., Rindlisbacher T., Elmaraghy A. Three-dimensional study of pectoralis major muscle and tendon architecture. Clin Anat. 2009;22:500–508. doi: 10.1002/ca.20784. [DOI] [PubMed] [Google Scholar]
- 11.Gupton M., Johnson J.E. Surgical treatment of pectoralis major muscle ruptures: a systematic review and meta-analysis. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967118824551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haladaj R., Wysiadecki G., Clarke E., Polguj M., Topol M. Anatomical variations of the pectoralis major muscle: notes on their impact on pectoral nerve innervation patterns and discussion on the their clinical relevance. Biomed Res Int. 2019;2019:6212039. doi: 10.1155/2019/6212039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasan S.A., Rauls R.B., Cordell C.L., Heinzelmann A.D., Siegel E.R. Pectoralis major insertional ratio in proximal humerus fractures: a method to reconstruct humeral head height in arthroplasty. Orthopedics. 2009;32 doi: 10.3928/01477447-20090818-13. [DOI] [PubMed] [Google Scholar]
- 14.Hoffman G.W., Elliott L.F. The anatomy of the pectoral nerves and its significance to the general and plastic surgeon. Ann Surg. 1987;205:504–507. doi: 10.1097/00000658-198705000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hussain W.M., Reddy D., Atanda A., Jones M., Schickendantz M., Terry M.A. The longitudinal anatomy of the long head of the biceps tendon and implications on tenodesis. Knee Surg Sports Traumatol Arthrosc. 2015;23:1518–1523. doi: 10.1007/s00167-014-2909-5. [DOI] [PubMed] [Google Scholar]
- 16.Jagiasi J.D., Valavi A.S., Ubale T.V., Sahu D. Insertion anatomy of the pectoralis major tendon. J Clin Orthop Trauma. 2019;10:541–543. doi: 10.1016/j.jcot.2019.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jarrett C.D., McClelland W.B., Jr., Xerogeanes J.W. Minimally invasive proximal biceps tenodesis: an anatomical study for optimal placement and safe surgical technique. J Shoulder Elbow Surg. 2011;20:477–480. doi: 10.1016/j.jse.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Jennings G.J., Keereweer S., Buijze G.A., DeBeer J., DuToit D. Transfer of segmentally split pectoralis major for the treatment of irreparable rupture of the subscapularis tendon. J Shoulder Elbow Surg. 2007;16:837–842. doi: 10.1016/j.jse.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 19.Klepps S., Auerbach J., Calhon O., Lin J., Cleeman E., Flatow E. A cadaveric study on the anatomy of the deltoid insertion and its relationship to the deltopectoral approach to the proximal humerus. J Shoulder Elbow Surg. 2004;13:322–327. doi: 10.1016/j.jse.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 20.Klepps S.J., Goldfarb C., Flatow E., Galatz L.M., Yamaguchi K. Anatomic evaluation of the subcoracoid pectoralis major transfer in human cadavers. J Shoulder Elbow Surg. 2001;10:453–459. doi: 10.1067/mse.2001.117125. [DOI] [PubMed] [Google Scholar]
- 21.Kretzler H.H., Jr., Richardson A.B. Rupture of the pectoralis major muscle. Am J Sports Med. 1989;17:453–458. doi: 10.1177/036354658901700401. [DOI] [PubMed] [Google Scholar]
- 22.LaFrance R., Madsen W., Yaseen Z., Giordano B., Maloney M., Voloshin I. Relevant anatomic landmarks and measurements for biceps tenodesis. Am J Sports Med. 2013;41:1396–1399. doi: 10.1177/0363546513482297. [DOI] [PubMed] [Google Scholar]
- 23.Lancaster S.T., Smith G.C., Ogunleye O.E., Clark D.A., Packham I.N. Proximity of axillary nerve during cortical button repair of pectoralis major tendon rupture. Shoulder Elbow. 2014;6:29–34. doi: 10.1111/sae.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lau B.H., Butterwick D.J., Lafave M.R., Mohtadi N.G. Retrospective review of pectoralis major ruptures in rodeo steer wrestlers. Adv Orthop. 2013:1–4. doi: 10.1155/2013/987910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee J., Brookenthal K.R., Ramsey M.L., Kneeland J.B., Herzog R. MR imaging assessment of the pectoralis major myotendinous unit: an MR imaging-anatomic correlative study with surgical correlation. AJR Am J Roentgenol. 2000;174:1371–1375. doi: 10.2214/ajr.174.5.1741371. [DOI] [PubMed] [Google Scholar]
- 26.Liu J.N., Gowd A.K., Garcia G.H., Manderle B.J., Beletsky A., Nicholson G.P. Analysis of return to sport and weight training after repair of the pectoralis major tendon. Am J Sports Med. 2019;47:2151–2157. doi: 10.1177/0363546519851506. [DOI] [PubMed] [Google Scholar]
- 27.Macchi V., Tiengo C., Porzionato A., Parenti A., Stecco C., Mazzoleni F. Medial and lateral pectoral nerves: course and branches. Clin Anat. 2007;20:157–162. doi: 10.1002/ca.20328. [DOI] [PubMed] [Google Scholar]
- 28.Moatshe G., Marchetti D.C., Chahla J., Ferrari M.B., Sanchez G., Lebus G.F., et al Qualitative and quantitative anatomy of the proximal humerus muscle attachments and the axillary nerve: a cadaveric study. Arthroscopy. 2018;34:795–803. doi: 10.1016/j.arthro.2017.08.301. [DOI] [PubMed] [Google Scholar]
- 29.Murachovsky J., Ikemoto R.Y., Nascimento L.G., Fujiki E.N., Milani C., Warner J.J. Pectoralis major tendon reference (PMT): a new method for accurate restoration of humeral length with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2006;15:675–678. doi: 10.1016/j.jse.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 30.Neviaser A.S., Patterson D.C., Cagle P.J., Parsons B.O., Flatow E.L. Anatomic landmarks for arthroscopic suprapectoral biceps tenodesis: a cadaveric study. J Shoulder Elbow Surg. 2018;27:1172–1177. doi: 10.1016/j.jse.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 31.Nossov S.B., Ross J.R., Robbins C.B., Carpenter J.E. Qualitative assessment and quantitative analysis of the long head of the biceps tendon in relation to the pectoralis major tendon humeral insertion: an anatomic study. Arthroscopy. 2016;32:990–998. doi: 10.1016/j.arthro.2015.11.048. [DOI] [PubMed] [Google Scholar]
- 32.Ponce B.A., Thompson K.J., Rosenzweig S.D., Tate J.P., Sarver D.B., Thorpe J.B., 2nd Re-evaluation of pectoralis major height as an anatomic reference for humeral height in fracture hemiarthroplasty. J Shoulder Elbow Surg. 2013;22:1567–1572. doi: 10.1016/j.jse.2013.01.039. [DOI] [PubMed] [Google Scholar]
- 33.Porzionato A., Macchi V., Stecco C., Loukas M., Tubbs R.S., De Caro R. Surgical anatomy of the pectoral nerves and the pectoral musculature. Clin Anat. 2012;25:559–575. doi: 10.1002/ca.21301. [DOI] [PubMed] [Google Scholar]
- 34.Prakash K.G., Kuppasad S. Anatomical study of pectoral nerves and its implications in surgery. J Clin Diagn Res. 2014;8:1–5. doi: 10.7860/JCDR/2014/8631.4545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sefa Özel M., Özel L., Toros S.Z., Marur T., Yıldırım Z., Erdoğdu E. Denervation point for neuromuscular blockade on lateral pectoral nerves: a cadaveric study. Surg Radiol Anat. 2011;33:105–108. doi: 10.1007/s00276-010-0712-7. [DOI] [PubMed] [Google Scholar]
- 36.Shiu B., Jazini E., Robertson A., Henn R.F., Hasan S.A. Anatomical relationship of the axillary nerve to the pectoralis major tendon insertion. Orthopedics. 2017;40:e460–e464. doi: 10.3928/01477447-20170208-04. [DOI] [PubMed] [Google Scholar]
- 37.Smith C.D., Booker S.J., Uppal H.S., Kitson J., Bunker T.D. Anatomy of the terminal branch of the posterior circumflex humeral artery: relevance to the deltopectoral approach to the shoulder. Bone Joint J. 2016;98-B:1395–1398. doi: 10.1302/0301-620X.98B10.38011. [DOI] [PubMed] [Google Scholar]
- 38.Torrens C., Corrales M., Melendo E., Solano A., Rodríguez-Baeza A., Cáceres E. The pectoralis major tendon as a reference for restoring humeral length and retroversion with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2008;17:947–950. doi: 10.1016/j.jse.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 39.Wolfe S.W., Wikiewicz T.L., Cavanaugh J.T. Rupture of the pectoralis major muscle. An anatomic and clinical analysis. Am J Sports Med. 1992;20:587–593. doi: 10.1177/036354659202000517. [DOI] [PubMed] [Google Scholar]
- 40.Yu J., Zhang C., Horner N., Ayeni O.R., Leroux T., Alolabi B., et al Outcomes and return to sport after pectoralis major tendon repair: a systematic review. Sports Health. 2019;11:134–141. doi: 10.1177/1941738118818060. [DOI] [PMC free article] [PubMed] [Google Scholar]