Abstract
Background
The majority of clavicle fractures are midshaft injuries, although fractures of the distal or medial fragment also occur. The aim of this study was to review the current evidence on these injuries to help inform future treatment plans.
Methods
We searched for studies comparing interventions for medial, midshaft, or distal clavicle fractures; however, we did not identify any comparative studies on medial fractures and performed a secondary search on this topic. We conducted Bayesian network meta-analyses, although this was not feasible with studies on medial fractures and we described their results qualitatively.
Results
For midshaft fractures, we found statistically significant improvements in function and time to radiographic union with plating, an elastic stable intramedullary nail (ESIN), and the Sonoma CRx intramedullary nail over nonoperative treatments. Both plating and an ESIN also showed significantly lower risks of nonunion and malunion relative to nonoperative methods. For distal fractures, a locking plate (LP) with or without coracoclavicular (CC) suturing yielded significantly better outcomes over K-wires with or without tension bands, CC suturing alone, an LP with a CC screw, a hook plate, and a sling. For medial fractures, plating may result in more favorable functional and union-related outcomes, although implant irritation may occur. In addition, K-wires, tension bands, and a screw with sutures demonstrated success when plating was technically not feasible in a few cases, whereas treatment with a sling may result in reduced function and a higher risk of complications relative to surgery.
Conclusion
This study can provide guidance on the management of medial, midshaft, and distal clavicle fractures. The current evidence suggests that plating, an ESIN, and a CRx intramedullary nail are all good options for midshaft fractures; an LP with or without CC suturing should be preferred for distal fractures; and plating is also acceptable for medial fractures, provided that the patient is deemed suitable for surgery and has the adequate bone stock and sufficiently sized medial fragment necessary to implant the device. Patient preferences for certain outcomes should be considered, which may result in different treatment recommendations.
Keywords: Clavicle, fracture, nonoperative, operative, systematic review, meta-analysis
Clavicle fractures are common, comprising 2%-4% of all fractures.36 The majority are midshaft fractures; however, injuries to the distal or medial fragment also occur.64,110 Clavicle fractures mostly occur in male individuals younger than 30 years, with an increased incidence, regardless of sex, above age 70 years.36 Historically, nonoperative methods were used to treat these injuries, as they were seen to have low rates of nonunion.61,70,92 However, some studies have shown unsatisfactory results with such treatments, including pain, cosmetic complaints, and brachial plexus irritation.27,42 Recent studies have suggested that surgery shows certain benefits, such as a quicker return of function, increased patient satisfaction, and fewer complications.55,80,110 Given the expected increase in the population of higher-risk groups, identifying an optimal treatment plan will become of greater importance.52
Multiple interventions are available to treat clavicle fractures, and options can vary depending on the location of the injury (ie, medial, midshaft, or distal).28,47,62,80 Determining the best approach is a complex decision, as both patient-reported and clinical outcomes are important to consider. Past trials and reviews have compared different operative techniques with each other or compared surgery with nonoperative protocols28,31,32; however, there exist few reviews that have examined these specific interventions all at once.
The aim of this systematic review and meta-analysis was to compare management options for medial, midshaft, and distal clavicle fractures to help inform future treatment plans.
Methods
Literature search
We searched the Embase, MEDLINE, and Cochrane databases (Supplementary Appendix S1), from database inception to March 14, 2019. We also identified a recent review on distal fractures with similar methodology and eligibility criteria7 and performed an update of their search on March 15, 2019. After article screening, we did not identify any comparative studies on medial fractures; therefore, we performed another search (Supplementary Appendix S2) on April 9, 2019, for studies on this injury.
Eligibility criteria
Initially, we included studies that (1) were comparative, examining at least 2 treatments for medial, midshaft, or distal clavicle fractures; (2) had an experimental or observational study design; (3) focused on skeletally mature patients; and (4) were published in English. As stated earlier, after article screening, we did not find any comparative studies on medial clavicle fractures. We performed another search for such studies using similar eligibility criteria, except that these studies were case series or case reports.
Article selection
Two reviewers screened titles, abstracts, and full-text articles, with discrepancies resolved through discussion.
Data extraction
We extracted study characteristics (ie, author, location, study length, and inclusion and exclusion criteria), patient characteristics (ie, age, sex, and fracture type), and outcome data (ie, patient-reported pain or function, time to union or return to work, and complications).
Statistical analysis
For midshaft and distal fractures, we conducted random-effects Bayesian network meta-analyses, with 95% credible intervals (CrIs). We calculated risk ratios for dichotomous variables and mean differences for continuous data. We represented heterogeneity as I2 values and calculated the surface area under the cumulative ranking curve (SUCRA) values.53 We conducted analyses using the “gemtc” package in R (version 3.5.0 [2018]; R Foundation for Statistical Computing, Vienna, Austria). For medial fracture studies, we described their results qualitatively.
Results
Search results
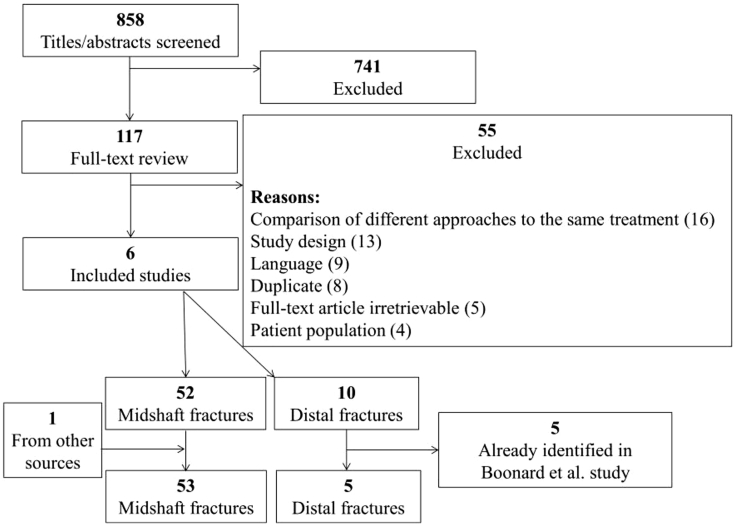
Our search retrieved 983 references, but 125 were duplicates. We included 117 for full-text review. We then deemed 62 articles eligible, with 52 on midshaft fractures and 10 on distal fractures; however, for distal fractures, we already identified 5 of them from the prior review, leaving 5 new studies on distal fractures. In addition, another study on midshaft fractures was identified by one of us from another source, leaving 53 included articles on midshaft fractures in this review (Fig. 1).1, 2, 3, 4,6,9,11, 12, 13, 14, 15,17,19,20,24, 25, 26,34,35,37,38,40,41,43,44,46,50,54,56, 57, 58, 59, 60,65,68,71,73,75,77,79,80,83,84,87,91,93,94,97,100, 101, 102, 103,108 One article was a secondary publication of a study, so we included 52 unique studies.73
Figure 1.
Flow diagram of included studies from initial search.
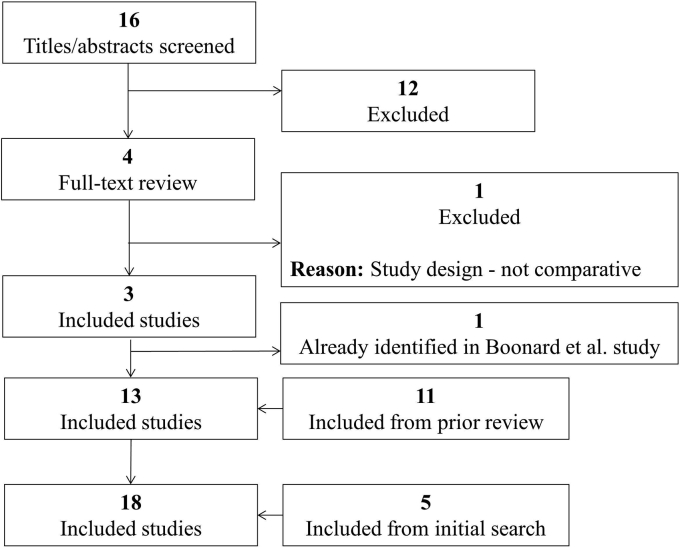
From the study by Boonard et al7 on distal fractures, we included 11 studies. After updating their search, we retrieved 18 references for screening but 2 were duplicates. We included 4 for full-text review. We then deemed 3 articles eligible, although 1 was a duplicate of an already included study, so only 2 were new studies. Thus, in addition to the 5 studies from our first search, we identified 18 studies on distal fractures (Fig. 2).10,18,21,22,29,30,39,45,48,69,74,82,85,86,90,104,106,107
Figure 2.
Flow diagram of included studies from distal clavicle fracture search.
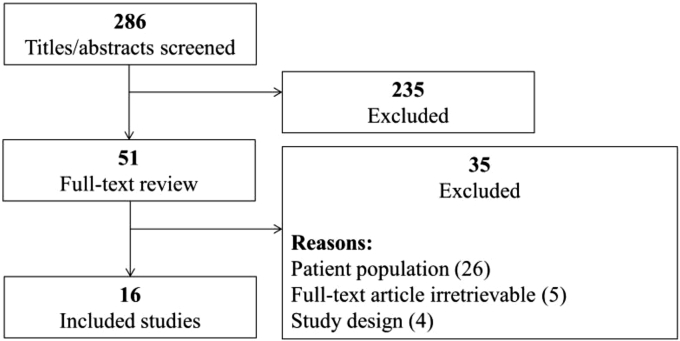
From the medial fracture search, we retrieved 354 references; however, 8 were duplicates and 60 were conference abstracts or reviews. We included 51 articles for full-text review and deemed 16 eligible for inclusion (Fig. 3).5,8,23,49,51,63,67,76,78,81,88,89,95,99,105,109
Figure 3.
Flow diagram of included studies from medial clavicle fracture search.
Study characteristics
The characteristics of the studies on midshaft fractures are shown in Table I. The studies were published from 1987 to 2019, and sample sizes ranged from 22 to 302 patients. Six interventions were identified: elastic stable intramedullary nail (ESIN), intramedullary pin (IMP), Sonoma CRx intramedullary nail (CRx; Sonoma Orthopedic Products, Santa Rosa, CA, USA), plating, figure-of-8 bandage (F8B), and sling. Some studies evaluated the use of an F8B and sling in combination. In terms of patient demographic characteristics, the average age across studies ranged from 24 to 60 years (median, 36 years) and the proportion of male patients ranged from 10% to 100% (median, 79%). The outcomes reported on that we analyzed were as follows: pain and function (at ≤4, 6, 12, 24, 52, and >52 weeks), time to radiographic union, time to return to work, delayed union, malunion, nonunion, refracture, revision, and symptoms.
Table I.
Study characteristics of midshaft clavicle fracture studies
| Authors, year | Location of study | Study design | Sample size | Treatments evaluated | Length of study follow-up | Age, yr | Male sex, % |
|---|---|---|---|---|---|---|---|
| Ahrens et al,1 2017 | United Kingdom | Randomized trial | 302 | Plate | 9 mo | Mean, 36 ± 12 | 86 |
| Sling | Mean, 36 ± 12 | 88 | |||||
| Andersen et al,2 1987 | Denmark | Randomized trial | 61 | F8B | 3 mo | Median, 19 (range, 14-81) | NR |
| Sling | Median, 19 (range, 14-66) | ||||||
| Andrade-Silva et al,3 2015 | Brazil | Randomized trial | 59 | Plate | 12 mo | Mean, 31 ± 12 | 85 |
| ESIN | Mean, 28 ± 9 | 73 | |||||
| Assobhi,4 2011 | Finland | Randomized trial | 38 | Plate | 12 mo | Mean, 33 ± 6 (range, 26-49) | 89 |
| ESIN | Mean, 30 ± 5 (range, 24-45) | 84 | |||||
| Bhardwaj et al,6 2018 | India | Randomized trial | 69 | Plate | 24 mo | Mean, 32 | 22 |
| Sling | Mean, 32 | 39 | |||||
| Calbiyik et al,9 2017 | Turkey | Randomized trial | 75 | CRx | 12 mo | Mean, 42 ± 14 | 60 |
| Plate | Mean, 39 ± 7 | 63 | |||||
| Chen et al,11 2018 | China | Randomized trial | 54 | Plate | Mean, 15 mo (range, 12-24 mo) | Mean, 38 ± 11 | 59 |
| ESIN | Mean, 39 ± 11 | 56 | |||||
| Chen et al,12 2011 | China | Randomized trial | 60 | ESIN | Mean, 15 mo (range, 10-20 mo) | Mean, 39 ± 12 | 53 |
| Sling | Mean, 38 ± 13 | 53 | |||||
| Chen et al,13 2012 | China | Observational | 141 | ESIN | 24 mo | Mean, 34 (range, 20-59) | 72 |
| Plate | Mean, 37 (range, 19-63) | 73 | |||||
| Chu et al,14 2018 | Taiwan | Observational | 120 | Plate | 6 mo | Mean, 46 ± 17 | 63 |
| F8B | Mean, 50 ± 15 | 73 | |||||
| Coppa et al,15 2017 | Italy | Observational | 58 | IMP | Mean, 47 mo (range, 23-74 mo) | Mean, 40 ± 16 | 93 |
| F8B | Mean, 37 ± 16 | 83 | |||||
| Eden et al,17 2015 | Germany | Observational | 102 | F8B | 12 mo | Mean, 41 ± 18 | NR |
| Plate | Mean, 38 ± 15 | ||||||
| ESIN | Mean, 34 ± 15 | ||||||
| Ersen et al,19 2015 | Turkey | Randomized trial | 60 | F8B | Mean, 8 mo (range, 6-12 mo) | Mean, 34 (range, 16-75) | 79 |
| Sling | Mean, 29 (range, 15-72) | 83 | |||||
| Ferran et al,20 2010 | United Kingdom | Quasi-randomized | 32 | IMP | 12 mo | Mean, 24 (range, 13-42) | 82 |
| Plate | Mean, 35 (range, 16-53) | 87 | |||||
| Fu et al,24 2012 | Taiwan | Observational | 103 | IMP | Mean, 15 mo (range, 12-153 mo) | Mean, 35 ± 15 | 72 |
| Plate | Mean, 40 ± 15 | 66 | |||||
| Fuglesang et al,25 2017 | Norway | Randomized trial | 123 | Plate | 12 mo | Mean, 35 (range, 16-59) | 81 |
| ESIN | Mean, 36 (range, 16-57) | 90 | |||||
| Hanselman et al,26 2016 | United States | Observational | 157 | Plate | Up to 5 yr | NR | NR |
| IMP | |||||||
| Jones et al,34 2014 | United Kingdom | Observational | 57 | Plate | Mean, 30 mo (range, 12-54 mo) | Mean, 27 ± 8 | 84 |
| ESIN | |||||||
| Judd et al,35 2009 | United States | Randomized trial | 70 | IMP | 12 mo | Mean, 28 (range, 19-40) | 93 |
| Sling | Mean, 25 (range, 17-41) | 89 | |||||
| Khorami et al,37 2014 | Iran | Randomized trial | 87 | F8B | 6 mo | Mean, 32 | 77 |
| Plate | Mean, 31 | 71 | |||||
| King et al,38 2019 | Turkey | Randomized trial | 87 | CRx | 15 mo | Mean, 29 ± 14 | 74 |
| Plate | Mean, 35 ± 12 | 54 | |||||
| Kleweno et al,40 2011 | United States | Observational | 32 | IMP | Mean, 8 mo (range, 3-28 mo) | Mean, 35 (range, 16-56) | 71 |
| Plate | Mean, 17 mo (range, 4-58 mo) | Mean, 28 (range, 16-46) | 83 | ||||
| Kulshrestha et al,41 2011 | India | Observational | 73 | Plate | 18 mo | Mean, 32 ± 6 | 96 |
| Sling | Mean, 33 ± 5 | 86 | |||||
| Lechler et al,43 2016 | Germany | Observational | 47 | ESIN | Mean, 38 mo | Mean, 36 ± 15 | 72 |
| Plate | Mean, 39 ± 15 | 64 | |||||
| Lee et al,44 2008 | Taiwan | Quasi-randomized | 103 | IMP | 12 mo | Mean, 40 | 66 |
| Plate | Mean, 38 | 63 | |||||
| Lee et al,46 2007 | Taiwan | Quasi-randomized | 69 | IMP | 30 mo | Mean, 60 (range, 50-81) | 59 |
| Plate | Mean, 57 (range, 52-79) | 57 | |||||
| Liu et al,50 2010 | Taiwan | Observational | 110 | ESIN | Mean, 18 mo (range, 12-27 mo) | Mean, 34 ± 14 (range, 16-65) | 63 |
| Plate | Mean, 32 ± 10 (range, 17-58) | 49 | |||||
| McKee et al,54 2007; Schemitsch et al,73 2011 | Canada | Randomized trial | 132 | Sling | 12 mo | Mean, 34 | 69 |
| Plate | Mean, 34 | 86 | |||||
| Melean et al,56 2015 | Chile | Randomized trial | 76 | Sling | 12 mo | Mean, 37 ± 11 | NR |
| Plate | Mean, 38 ± 13 | ||||||
| Mirzatolooei,57 2011 | Iran | Randomized trial | 60 | Sling | 12 mo | Mean, 35 | 10 |
| Plate | Mean, 36 | 21 | |||||
| Napora et al,58 2018 | United States | Observational | 138 | Sling | ≥12 mo | Range, 16-71 | NR |
| Plate | Range, 16-71 | ||||||
| Narsaria et al,59 2014 | India | Randomized trial | 66 | Plate | 24 mo | Mean, 40 ± 11 (range, 18-64) | 79 |
| ESIN | Mean, 39 ± 9 (range, 20-62) | 73 | |||||
| Naveen et al,60 2017 | India | Nonrandomized controlled trial | 60 | F8B and sling | 6 mo | Mean, 35 | 90 |
| Plate | Mean, 32 | 87 | |||||
| Qvist et al,65 2018 | Denmark | Randomized trial | 150 | Sling | 12 mo | Mean, 39 (range, 18-60) | 92 |
| Plate | Mean, 40 (range, 18-60) | 100 | |||||
| Robinson et al,68 2013 | United Kingdom | Randomized trial | 200 | Sling | 12 mo | Mean, 33 ± 13 | 88 |
| Plate | Mean, 32 ± 11 | 87 | |||||
| Saha et al,71 2014 | India | Quasi-randomized | 80 | Plate | 24 mo | Mean, 33 ± 13 (range, 15-58) | NR |
| ESIN | Mean, 33 ± 12 (range, 15-55) | ||||||
| Shetty et al,75 2017 | India | Randomized trial | 30 | F8B and sling | 6 mo | NR | NR |
| Plate | |||||||
| Silva et al,77 2011 | Brazil | Randomized trial | 22 | Plate | 6 mo | NR | NR |
| ESIN | |||||||
| Smekal et al,79 2011 | Austria | Randomized trial | 120 | Sling | 24 mo | Mean, 38 ± 15 | 85 |
| ESIN | Mean, 37 ± 13 | 90 | |||||
| Smekal et al,80 2009 | Austria | Randomized trial | 60 | Sling | 24 mo | Mean, 40 ± 15 | 87 |
| ESIN | Mean, 36 ± 12 | 87 | |||||
| Tabatabaei and Shalamzari,83 2011 | Iran | Nonrandomized controlled trial | 68 | IMP | Mean, 14 mo | Mean, 29 | 84 |
| Plate | Mean, 27 | 84 | |||||
| Tamaoki et al,84 2017 | Brazil | Randomized trial | 117 | F8B | 12 mo | Mean, 35 ± 13 | 81 |
| Plate | Mean, 31 ± 10 | 90 | |||||
| Tarng et al,87 2012 | Taiwan | Observational | 57 | Plate | 12 mo | Mean, 47 (IQR, 37-59) | 56 |
| ESIN | Mean, 38 (IQR, 27-58) | 40 | |||||
| Tutuhatunewa et al,91 2017 | The Netherlands | Observational | 278 | Sling | Median, 26 mo (range, 15-41 mo) | Median, 42 (IQR, 26-56) | 78 |
| Plate | Median, 27 mo (range, 18-37 mo) | Median, 40 (IQR, 24-50) | 86 | ||||
| van der Meijden et al,93 2015 | The Netherlands | Randomized trial | 120 | Plate | 12 mo | Mean, 38 ± 15 | 91 |
| ESIN | Mean, 40 ± 13 | 97 | |||||
| Van Der Ven Denise et al,94 2015 | The Netherlands | Observational | 97 | Sling | Mean, 60 mo | Mean, 41 ± 15 | 85 |
| Plate | Mean, 41 ± 13 | 90 | |||||
| Virtanen et al,97 2012 | Finland | Randomized trial | 60 | Sling | 12 mo | Mean, 33 ± 12 | 88 |
| Plate | Mean, 41 ± 11 | 86 | |||||
| Wang et al,100 2015 | Taiwan | Observational | 55 | Plate | 12 mo | Mean, 35 (range, 16-60) | 70 |
| ESIN | Mean, 42 (range, 16-66) | 68 | |||||
| Wenninger et al,101 2013 | United States | Observational | 65 | IMP | 12 mo | Mean, 25 (range, 18-51) | 97 |
| Plate | Mean, 27 (range, 20-49) | 90 | |||||
| Wijdicks et al,102 2012 | The Netherlands | Observational | 90 | Plate | Median, 8 mo (IQR, 2-13) | Mean, 39 ± 14 | 77 |
| ESIN | Median, 6 mo (IQR, 5-12) | Mean, 33 ± 16 | 70 | ||||
| Woltz et al,103 2017 | The Netherlands | Randomized trial | 160 | Sling | 12 mo | Mean, 37 ± 13 | 89 |
| Plate | Mean, 38 ± 13 | 93 | |||||
| Zehir et al,108 2015 | Turkey | Randomized trial | 45 | CRx | Mean, 12 mo | Mean, 33 ± 9 | 58 |
| Plate | Mean, 14 mo | Mean, 32 ± 8 | 57 |
F8B, figure-of-eight bandage; NR, not reported; ESIN, elastic stable intramedullary nail; CRx, Sonoma CRx intramedullary nail; IMP, intramedullary pin; IQR, interquartile range.
The studies on distal fractures were published between 2002 and 2018, and sample sizes ranged from 15 to 116 patients (Table II). The interventions compared in the studies were as follows: coracoclavicular suturing (CCSu) alone, CCSu with a locking plate (CCSu-LP), CCSu with K-wires (CCSu-KW), coracoclavicular screw fixation with an LP (CCSc-LP), a hook plate (HP), K-wires (KW) alone, a locking plate (LP) alone, tension bands with K-wires (TB-KW), and a sling. The average age of patients ranged from 34 to 51 years (median, 42 years), and the percentage of male patients ranged from 45% to 95% (median, 68%). In terms of fracture classification, patients predominantly had Neer type II fractures, with rates ranging from 60% to 100% of patients (median, 100%) across studies, but a small proportion sustained Neer type V fractures (range, 0%-40%; median, 0%). The studies provided sufficient data on function (at 3 months, 6 months, and ≥1 year of follow-up); time to radiographic union; and the risks of hardware problems, nonunion, refracture, revision, and symptoms.
Table II.
Study characteristics of distal clavicle fracture studies
| Authors, year | Study location | Study design | Sample size | Interventions | Length of follow-up | Age, yr | Male sex, % |
|---|---|---|---|---|---|---|---|
| Chen et al,10 2014 | Taiwan | Observational | 94 | CC suture | Mean, 38 mo (range, 24-64 mo) | Mean, 43 (range, 18-75) | 70 |
| Hook plate | Mean, 37 mo (range, 24-68 mo) | Mean, 48 (range, 28-78) | 57 | ||||
| Erdle et al,18 2017 | Germany | Observational | 32 | Hook plate | Mean, 54 mo (range, 25-111 mo) | Mean, 44 ± 15 | 88 |
| Locking plate | Mean, 44 ± 14 | 88 | |||||
| Flinkkila et al,22 2002 | Finland | Observational | 39 | Hook plate | Mean, 2 yr (range, 1-2 yr) | Mean, 43 (range, 18-71) | 94 |
| K-wire | Mean, 6 yr (range, 3-12 yr) | Mean, 35 (range, 17-68) | 73 | ||||
| Flinkkila et al,21 2015 | Finland | Observational | 40 | CC suture | Mean, 32 mo | Mean, 39 ± 14 | 95 |
| Hook plate | Mean, 62 mo | Mean, 45 ± 13 | 68 | ||||
| Hsu et al,30 2010 | Taiwan | Randomized trial | 65 | Hook plate | 6 mo | Mean, 43 ± 13 (range, 22-67) | 60 |
| TB and K-wire | Mean, 41 ± 14 (range, 22-67) | 77 | |||||
| Hsu et al,29 2018 | Taiwan | Observational | 72 | CC suture | 12 mo | Mean, 42 ± 16 | 70 |
| Hook plate | Mean, 48 ± 20 | 59 | |||||
| Klein et al,39 2010 | United States | Observational | 38 | CC suture and locking plate | Mean, 12 mo (range, 2-47 mo) | Mean, 43 | 61 |
| Hook plate | Mean, 43 | ||||||
| Lee et al,45 2009 | Taiwan | Observational | 66 | Hook plate | Mean, 26 mo (range, 12-64 mo) | Mean, 43 (range, 18-70) | 56 |
| TB and K-wire | Mean, 36 (range, 18-70) | 45 | |||||
| Leu et al,48 2012 | Taiwan | Observational | 45 | Hook plate | Mean, 15 mo (range, 12-25 mo) | Mean, 41 ± 18 | 52 |
| TB and K-wire | Mean, 41 ± 14 | 50 | |||||
| Rokito et al,69 2003 | United States | Observational | 30 | Sling | Mean, 54 mo (range, 30-90 mo) | Mean, 47 (range, 26-68) | 63 |
| CC suture | Mean, 60 mo (range, 12-107 mo) | Mean, 36 (range, 22-47) | 57 | ||||
| Seyhan et al,74 2015 | Turkey | Observational | 36 | CC suture and locking plate | 24 mo | Mean, 38 (range, 20-55) | 71 |
| CC screw and locking plate | Mean, 36 (range, 34-41) | 75 | |||||
| TB and K-wire | Mean, 34 (range, 26-44) | 60 | |||||
| Souza Vilela et al,82 2015 | Brazil | Observational | 15 | CC suture and K-wire | Two different sets of values reported: Mean, 23 mo (range, 14-32 mo) Mean, 27 mo (range, 18-36 mo) |
Mean, 34 (range, 19-57) | 69 |
| Locking plate | Mean, 34 (range, 19-57) | ||||||
| Tan et al,85 2012 | China | Observational | 42 | Hook plate | Mean, 22 mo (range, 12-48 mo) | Mean, 42 ± 11 (range, 21-65) | 65 |
| Locking plate | Mean, 22 mo (range, 12-48 mo) | Mean, 40 ± 10 (range, 22-61) | 68 | ||||
| Tang et al,86 2018 | China | Observational | 40 | CC suture and locking plate | Mean, 16 mo (range, 12-27 mo) | Mean, 43 ± 6 | NR |
| Locking plate | Mean, 43 ± 5 | ||||||
| Tsuei et al,90 2010 | Taiwan | Randomized trial | 29 | K-wire | Mean, 45 mo (range, 10-85 mo) | Mean, 39 ± 15 (range, 23-56) | 64 |
| TB and K-wire | Mean, 39 ± 14 (range, 21-61) | 73 | |||||
| Wu et al,104 2011 | Taiwan | Observational | 116 | Hook plate | Mean, 23 mo | Mean, 49 ± 16 | 60 |
| TB and K-wire | Mean, 26 mo | Mean, 51 ± 18 | 71 | ||||
| Xiong et al,106 2018 | China | Observational | 58 | CC suture | Mean, 57 mo (range, 7-160 mo) | Mean, 42 ± 14 | NR |
| Hook plate | Mean, 47 ± 16 | ||||||
| Locking plate | Mean, 38 ± 15 | ||||||
| Yan et al,107 2017 | China | Randomized trial | 72 | CC suture | 24 mo | Mean, 38 (range, 20-55) | 71 |
| Hook plate | Mean, 35 (range, 21-56) | 67 |
CC, coracoclavicular; TB, tension band; NR, not reported.
The studies on medial fractures were published between 2004 and 2019 (Table III). The interventions were as follows: plating, tension bands (TB), KW, a screw and sutures, and a sling. Across the case reports, the age of patients ranged from 17 to 63 years, and among the remaining studies, the mean age ranged from 34 to 56 years. The patients were predominantly men, as the subjects of 5 of the 6 case reports were men and, across the remaining studies, the proportion of men ranged from 64% to 100%. The outcomes reported on were pain and function, radiographic union, return to prior activities, and various complications.
Table III.
Study characteristics of medial clavicle fracture studies
| Authors, year | Study location | Study design | Sample size | Interventions | Length of follow-up | Age, yr | Male sex, % |
|---|---|---|---|---|---|---|---|
| Bartonicek et al,5 2010 | Czech Republic | Case series | 4 | Tension band, sling | Range, 12-24 mo | Mean, 45 | 100 |
| Bourghli and Fabre,8 2012 | France | Case report | 1 | K-wires | 8 mo | 29 | 100 |
| Frima et al,23 2018 | Switzerland | Case series | 15 | Locking plate | Mean, 39 mo (range, 9-79 mo) | Mean, 52 | 100 |
| Li et al,49 2019 | China | Case report | 1 | Locking plate | 6 mo | 56 | 100 |
| Low et al,51 2008 | Australia | Case series | 4 | Locking plate, screw and sutures | Mean, 3 yr (range, 8 mo to 10 yr) | Mean, 43 | 100 |
| Oe et al,63 2012 | Germany | Case series | 9 | Locking plate | Mean, 38 mo (range, 14-52 mo) | Mean, 36 | 89 |
| Robinson et al,67 2004 | United Kingdom | Case series | 24 | Sling | 24 wk | Median, 52 | 67 |
| Siebenlist et al,76 2013 | Germany | Case report | 1 | Locking plate | 1 yr | 63 | 100 |
| Singh et al,78 2012 | United Kingdom | Observational cohort | 4 | Sling | Range, 12-28 mo | NR | NR |
| Smelt et al,81 2017 | United Kingdom | Case report | 1 | Locking plate | 2 wk | 17 | 100 |
| Teng and Liu,88 2013 | Taiwan | Case report | 1 | Locking plate | 4 yr | 29 | 0 |
| Titchener et al,89 2019 | United Kingdom | Case series | 7 | Locking plate | Median, 31 mo (range, 24-45 mo) | Mean, 34 | 86 |
| Van Tongel et al,95 2018 | Belgium | Observational cohort | 55 | Sling | Mean, 49 mo (range, 6-101 mo) | Mean, 56 | 64 |
| Wang et al,99 2015 | China | Case report | 1 | Locking plate | 12 mo | 40 | 100 |
| Xie et al,105 2018 | China | Case series | 6 | Locking plate | Mean, 12 mo (range, 10-14 mo) | Mean, 46 | 83 |
| Zheng et al,109 2018 | China | Case series | 12 | Locking plate | Mean, 23 mo (range, 12-30 mo) | Mean, 44 | 83 |
NR, not reported.
Outcomes
Midshaft fractures
Pain
No statistically significant differences in pain were found between treatments at any follow-up visit. In terms of effect estimates, plating was ranked highest at ≤4, 6, and 12 weeks whereas the ESIN was highest at 24, 52, and >52 weeks (Table IV, Supplementary Fig. S1).
Table IV.
Effect estimates of all pair-wise comparisons for midshaft clavicle fractures
| Outcome | Comparison | MD or RR [95% CrI] |
|---|---|---|
| Pain score (0-100) at ≤4 wk | ESIN vs. F8B | MD, 0.61 [−11.75 to 12.77] |
| ESIN vs. plate | MD, 9.49 [−2.53 to 21.63] | |
| ESIN vs. sling | MD, 2.09 [−11.99 to 16.18] | |
| F8B vs. plate | MD, 8.91 [−1.09 to 18.86] | |
| F8B vs. sling | MD, 1.45 [−7.85 to 11.33] | |
| Plate vs. sling | MD, −7.42 [−17.4 to 3.17] | |
| Pain score (0-100) at 6 wk | ESIN vs. F8B | MD, −9.18 [−42.54 to 24.17] |
| ESIN vs. plate | MD, 3.07 [−30.08 to 36.55] | |
| ESIN vs. sling | MD, 3.14 [−46.86 to 52.71] | |
| F8B vs. plate | MD, 12.36 [−8.65 to 33.27] | |
| F8B vs. sling | MD, 12.31 [−30.14 to 54.83] | |
| Plate vs. sling | MD, 0.05 [−36.96 to 36.81] | |
| Pain score (0-100) at 12 wk | ESIN vs. F8B | MD, −1.04 [−25.69 to 23.38] |
| ESIN vs. plate | MD, 6.03 [−18.98 to 30.30] | |
| ESIN vs. sling | MD, 4.67 [−25.81 to 34.93] | |
| F8B vs. plate | MD, 7.09 [−7.63 to 21.26] | |
| F8B vs. sling | MD, 5.71 [−14.61 to 26.08] | |
| Plate vs. sling | MD, −1.32 [−21.51 to 18.99] | |
| Pain score (0-100) at 24 wk | ESIN vs. F8B | MD, −5.60 [−20.91 to 9.60] |
| ESIN vs. plate | MD, −1.46 [−16.74 to 13.55] | |
| F8B vs. plate | MD, 4.14 [−5.03 to 13.16] | |
| Pain score (0-100) at 52 wk | ESIN vs. F8B | MD, −2.78 [−10.79 to 5.34] |
| ESIN vs. plate | MD, −3.29 [−11.24 to 4.88] | |
| ESIN vs. sling | MD, −7.26 [−18.80 to 4.32] | |
| F8B vs. plate | MD, −0.51 [−5.25 to 4.23] | |
| F8B vs. sling | MD, −4.49 [−14.19 to 5.22] | |
| Plate vs. sling | MD, −3.95 [−12.41 to 4.52] | |
| Pain score (0-100) at >52 wk | ESIN vs. plate | MD, −9.98 [−23.86 to 4.04] |
| ESIN vs. sling | MD, −7.96 [−26.96 to 10.83] | |
| Plate vs. sling | MD, 2.00 [−11.11 to 14.97] | |
| Function score (0-100) at ≤4 wk | ESIN vs. F8B | MD, 5.40 [−23.72 to 34.69] |
| ESIN vs. IMP | MD, 15.17 [−30.04 to 60.34] | |
| ESIN vs. plate | MD, −2.72 [−24.36 to 20.11] | |
| ESIN vs. sling | MD, 28.63 [−2.71 to 60.30] | |
| F8B vs. IMP | MD, 9.70 [−44.29 to 63.45] | |
| F8B vs. plate | MD, −8.04 [−36.92 to 21.63] | |
| F8B vs. sling | MD, 23.21 [−20.15 to 66.15] | |
| IMP vs. plate | MD, −17.86 [−67.07 to 32.03] | |
| IMP vs. sling | MD, 13.39 [−19.27 to 46.33] | |
| Plate vs. sling | MD, 31.33 [−7.71 to 69.54] | |
| Function score (0-100) at 6 wk | CRx vs. ESIN | MD, 9.46 [−12.59 to 30.83] |
| CRx vs. F8B | MD, 17.05 [−7.41 to 41.30] | |
| CRx vs. F8B + sling | MD, 17.93 [−7.07 to 42.87] | |
| CRx vs. IMP | MD, 10.36 [−20.38 to 40.70] | |
| CRx vs. plate | MD, 11.04 [−9.78 to 31.58 ] | |
| CRx vs. sling | MD, 20.16 [−1.61 to 42.08] | |
| ESIN vs. F8B | MD, 7.67 [−6.13 to 21.53] | |
| ESIN vs. F8B + sling | MD, 8.54 [−7.37 to 24.26] | |
| ESIN vs. IMP | MD, 0.87 [−22.86 to 24.60] | |
| ESIN vs. plate | MD, 1.60 [−5.31 to 8.51] | |
| ESIN vs. sling∗ | MD, 10.73 [1.21 to 20.35] | |
| F8B vs. F8B + sling | MD, 0.90 [−18.47 to 20.27] | |
| F8B vs. IMP | MD, −6.72 [−32.91 to 19.45] | |
| F8B vs. plate | MD, −6.07 [−19.06 to 7.05] | |
| F8B vs. sling | MD, 3.09 [−11.74 to 17.99] | |
| F8B + sling vs. IMP | MD, −7.54 [−34.40 to 19.18] | |
| F8B + sling vs. plate | MD, −6.91 [−21.04 to 7.39] | |
| F8B + sling vs. sling | MD, 2.23 [−13.68 to 18.32] | |
| IMP vs. plate | MD, 0.69 [−22.26 to 23.48] | |
| IMP vs. sling | MD, 9.79 [−11.73 to 31.50] | |
| Plate vs. sling∗ | MD, 9.12 [1.66 to 16.66] | |
| Function score (0-100) at 12 wk | CRx vs. ESIN | MD, 7.88 [−5.32 to 21.12] |
| CRx vs. F8B∗ | MD, 14.89 [0.22 to 29.65] | |
| CRx vs. F8B + sling∗ | MD, 17.86 [1.07 to 34.49] | |
| CRx vs. IMP | MD, 5.16 [−16.23 to 26.52] | |
| CRx vs. plate | MD, 9.98 [−2.42 to 22.53] | |
| CRx vs. sling | MD, 12.88 [−0.16 to 26.24] | |
| ESIN vs. F8B | MD, 7.07 [−1.27 to 15.43] | |
| ESIN vs. F8B + sling | MD, 9.96 [−1.83 to 21.96] | |
| ESIN vs. IMP | MD, −2.66 [−20.27 to 15.17] | |
| ESIN vs. plate | MD, 2.12 [−2.25 to 6.65] | |
| ESIN vs. sling | MD, 5.03 [−0.49 to 10.74] | |
| F8B vs. F8B + sling | MD, 2.92 [−10.79 to 16.62] | |
| F8B vs. IMP | MD, −9.74 [−28.31 to 8.90] | |
| F8B vs. plate | MD, −4.95 [−12.88 to 3.11] | |
| F8B vs. sling | MD, −2.03 [−9.98 to 5.98] | |
| F8B + sling vs. IMP | MD, −12.63 [−33.22 to 7.97] | |
| F8B + sling vs. plate | MD, −7.82 [−18.99 to 3.37] | |
| F8B + sling vs. sling | MD, −4.90 [−16.65 to 6.84] | |
| IMP vs. plate | MD, 4.79 [−12.59 to 22.03] | |
| IMP vs. sling | MD, 7.69 [−9.03 to 24.55] | |
| Plate vs. sling | MD, 2.91 [−1.16 to 7.01] | |
| Function score (0-100) at 24 wk | CRx vs. ESIN | MD, 8.01 [−1.56 to 17.68] |
| CRx vs. F8B∗ | MD, 14.65 [4.70 to 24.79] | |
| CRx vs. F8B + sling∗ | MD, 13.39 [2.04 to 24.53] | |
| CRx vs. IMP∗ | MD, 12.18 [1.16 to 23.34] | |
| CRx vs. plate∗ | MD, 9.99 [0.87 to 19.27] | |
| CRx vs. sling∗ | MD, 14.59 [4.97 to 24.49] | |
| ESIN vs. F8B∗ | MD, 6.65 [1.90 to 11.39] | |
| ESIN vs. F8B + sling | MD, 5.35 [−1.74 to 12.25] | |
| ESIN vs. IMP | MD, 4.13 [−2.53 to 10.96] | |
| ESIN vs. plate | MD, 1.97 [−0.81 to 4.79] | |
| ESIN vs. sling∗ | MD, 6.58 [2.60 to 10.65] | |
| F8B vs. F8B + sling | MD, −1.30 [−9.04 to 6.16] | |
| F8B vs. IMP | MD, −2.54 [−9.93 to 4.96] | |
| F8B vs. plate∗ | MD, −4.68 [−8.75 to −0.57] | |
| F8B vs. sling | MD, −0.09 [−5.19 to 5.14] | |
| F8B + sling vs. IMP | MD, −1.23 [−10.03 to 7.92] | |
| F8B + sling vs. plate | MD, −3.37 [−9.63 to 3.24] | |
| F8B + sling vs. sling | MD, 1.22 [−5.77 to 8.52] | |
| IMP vs. plate | MD, −2.14 [−8.40 to 4.00] | |
| IMP vs. sling | MD, 2.47 [−3.93 to 8.84] | |
| Plate vs. sling∗ | MD, 4.60 [1.45 to 7.86] | |
| Function score (0-100) at 52 wk | CRx vs. ESIN | MD, 2.53 [−3.42 to 8.43] |
| CRx vs. F8B | MD, 4.27 [−2.62 to 11.20] | |
| CRx vs. IMP | MD, 3.52 [−3.48 to 10.63] | |
| CRx vs. plate | MD, 2.84 [−2.01 to 7.70] | |
| CRx vs. sling∗ | MD, 5.82 [0.31 to 11.47] | |
| ESIN vs. F8B | MD, 1.72 [−3.81 to 7.37] | |
| ESIN vs. IMP | MD, 0.99 [−5.07 to 7.08] | |
| ESIN vs. plate | MD, 0.28 [−3.00 to 3.74] | |
| ESIN vs. sling | MD, 3.29 [−0.87 to 7.67] | |
| F8B vs. IMP | MD, −0.72 [−7.68 to 6.28] | |
| F8B vs. plate | MD, −1.42 [−6.36 to 3.55] | |
| F8B vs. sling | MD, 1.56 [−3.55 to 6.85] | |
| IMP vs. plate | MD, −0.70 [−5.72 to 4.34] | |
| IMP vs. sling | MD, 2.30 [−2.89 to 7.61] | |
| Plate vs. sling∗ | MD, 3.00 [0.33 to 5.73] | |
| Function score (0-100) at >52 wk | ESIN vs. F8B | MD, 0.98 [−12.32 to 14.47] |
| ESIN vs. IMP | MD, −0.85 [−9.71 to 8.16] | |
| ESIN vs. plate | MD, 0.11 [−2.43 to 2.92] | |
| ESIN vs. sling∗ | MD, 4.75 [1.56 to 8.04] | |
| F8B vs. IMP | MD, −1.85 [−11.78 to 8.15] | |
| F8B vs. plate | MD, −0.82 [−14.06 to 12.27] | |
| F8B vs. sling | MD, 3.81 [−9.82 to 17.15] | |
| IMP vs. plate | MD, 0.99 [−7.46 to 9.57] | |
| IMP vs. sling | MD, 5.63 [−3.47 to 14.56] | |
| Plate vs. sling∗ | MD, 4.63 [1.56 to 7.54] | |
| Time to radiographic union, wk | CRx vs. ESIN | MD, −4.50 [−10.33 to 1.61] |
| CRx vs. F8B∗ | MD, −10.44 [−19.73 to −1.04] | |
| CRx vs. IMP | MD, −4.73 [−12.23 to 2.78] | |
| CRx vs. plate | MD, −5.38 [−10.73 to 0.00] | |
| CRx vs. sling∗ | MD, −11.37 [−17.79 to −4.73] | |
| ESIN vs. F8B | MD, −5.96 [−14.21 to 1.94] | |
| ESIN vs. IMP | MD, −0.24 [−6.32 to 5.51] | |
| ESIN vs. plate | MD, −0.89 [−3.63 to 1.63] | |
| ESIN vs. sling∗ | MD, −6.88 [−10.55 to −3.27] | |
| F8B vs. IMP | MD, 5.70 [−3.50 to 14.86] | |
| F8B vs. plate | MD, 5.08 [−2.54 to 12.69] | |
| F8B vs. sling | MD, −0.91 [−9.22 to 7.71] | |
| IMP vs. plate | MD, −0.63 [−5.89 to 4.61] | |
| IMP vs. sling∗ | MD, −6.62 [−12.93 to −0.05] | |
| Plate vs. sling∗ | MD, −5.99 [−9.67 to −2.15] | |
| Time to return to work, wk | ESIN vs. F8B | MD, −2.80 [−6.16 to 0.37] |
| ESIN vs. plate | MD, −1.30 [−4.04 to 1.48] | |
| ESIN vs. sling | MD, −2.44 [−5.77 to 0.76] | |
| F8B vs. plate | MD, 1.49 [−0.64 to 3.90] | |
| F8B vs. sling | MD, 0.35 [−2.16 to 3.00] | |
| Plate vs. sling | MD, −1.14 [−3.10 to 0.71] | |
| Delayed union | CRx vs. ESIN | RR, 1.21 [0.00 to 473] |
| CRx vs. F8B | RR, 1.63 [0.00 to 1097] | |
| CRx vs. IMP | RR, 0.41 [0.00 to 270] | |
| CRx vs. plate | RR, 2.80 [0.02 to 523] | |
| CRx vs. sling | RR, 1.30 [0.01 to 408] | |
| ESIN vs. F8B | RR, 1.34 [0.03 to 183] | |
| ESIN vs. IMP | RR, 0.34 [0.00 to 50] | |
| ESIN vs. plate | RR, 2.32 [0.11 to 81] | |
| ESIN vs. sling | RR, 1.06 [0.08 to 22] | |
| F8B vs. IMP | RR, 0.25 [0.00 to 40] | |
| F8B vs. plate | RR, 1.77 [0.03 to 50] | |
| F8B vs. sling | RR, 0.81 [0.01 to 37] | |
| IMP vs. plate | RR, 6.82 [0.13 to 804] | |
| IMP vs. sling | RR, 3.11 [0.06 to 463] | |
| Plate vs. sling | RR, 0.46 [0.04 to 5.15] | |
| Malunion | ESIN vs. F8B + sling∗ | RR, 0.11 [0.00 to 0.93] |
| ESIN vs. IMP | RR, 1.09 [0.16 to 6.30] | |
| ESIN vs. plate | RR, 2.27 [0.84 to 6.11] | |
| ESIN vs. sling | RR, 0.59 [0.21 to 1.65] | |
| F8B + sling vs. IMP | RR, 10 [0.83 to 395] | |
| F8B + sling vs. plate∗ | RR, 20 [3.19 to 679] | |
| F8B + sling vs. sling | RR, 5.40 [0.75 to 183] | |
| IMP vs. plate | RR, 2.08 [0.46 to 11] | |
| IMP vs. sling | RR, 0.54 [0.11 to 3.32] | |
| Plate vs. sling∗ | RR, 0.26 [0.14 to 0.49] | |
| Nonunion | ESIN vs. F8B∗ | RR, 0.26 [0.06 to 0.91] |
| ESIN vs. F8B + sling∗ | RR, 0.00 [0.00 to 0.13] | |
| ESIN vs. IMP | RR, 0.69 [0.20 to 2.18] | |
| ESIN vs. plate | RR, 1.67 [0.89 to 3.39] | |
| ESIN vs. sling∗ | RR, 0.38 [0.19 to 0.79] | |
| F8B vs. F8B + sling∗ | RR, 0.00 [0.00 to 0.51] | |
| F8B vs. IMP | RR, 2.66 [0.63 to 13] | |
| F8B vs. plate∗ | RR, 6.36 [2.18 to 24] | |
| F8B vs. sling | RR, 1.46 [0.46 to 5.78] | |
| IMP vs. F8B + sling∗ | RR, 0.00 [0.00 to 0.18] | |
| Plate vs. F8B + sling∗ | RR, 0.00 [0.00 to 0.08] | |
| Sling vs. F8B + sling∗ | RR, 0.00 [0.00 to 0.34] | |
| IMP vs. plate | RR, 2.41 [0.96 to 6.89] | |
| IMP vs. sling | RR, 0.55 [0.20 to 1.68] | |
| Plate vs. sling∗ | RR, 0.23 [0.15 to 0.35] | |
| Refracture | ESIN vs. IMP | RR, 1.73 [0.13 to 32] |
| ESIN vs. plate | RR, 1.03 [0.23 to 5.87] | |
| ESIN vs. sling | RR, 2.77 [0.38 to 37] | |
| IMP vs. plate | RR, 0.59 [0.06 to 5.42] | |
| IMP vs. sling | RR, 1.60 [0.15 to 21] | |
| Plate vs. sling | RR, 2.69 [0.56 to 20] | |
| Revision | ESIN vs. F8B | RR, 3.16 [0.29 to 104] |
| ESIN vs. IMP | RR, 0.17 [0.00 to 2.44] | |
| ESIN vs. plate | RR, 1.09 [0.37 to 3.35] | |
| ESIN vs. sling | RR, 0.83 [0.23 to 2.90] | |
| F8B vs. IMP | RR, 0.05 [0.00 to 1.60] | |
| F8B vs. plate | RR, 0.34 [0.01 to 3.86] | |
| F8B vs. sling | RR, 0.26 [0.01 to 3.07] | |
| IMP vs. plate | RR, 6.30 [0.61 to 189] | |
| IMP vs. sling | RR, 4.72 [0.40 to 144] | |
| Plate vs. sling | RR, 0.76 [0.38 to 1.37] | |
| Symptoms | CRx vs. ESIN | RR, 0.32 [0.00 to 58] |
| CRx vs. F8B | RR, 0.90 [0.00 to 245] | |
| CRx vs. IMP | RR, 0.86 [0.00 to 118] | |
| CRx vs. plate | RR, 0.43 [0.00 to 46] | |
| CRx vs. sling | RR, 2.04 [0.01 to 608] | |
| ESIN vs. F8B | RR, 2.80 [0.07 to 145] | |
| ESIN vs. IMP | RR, 2.69 [0.17 to 46] | |
| ESIN vs. plate | RR, 1.35 [0.13 to 14] | |
| ESIN vs. sling | RR, 6.30 [0.22 to 372] | |
| F8B vs. IMP | RR, 0.96 [0.04 to 20] | |
| F8B vs. plate | RR, 0.48 [0.02 to 9.49] | |
| F8B vs. sling | RR, 2.24 [0.05 to 193] | |
| IMP vs. plate | RR, 0.50 [0.11 to 2.20] | |
| IMP vs. sling | RR, 2.31 [0.13 to 85] | |
| Plate vs. sling | RR, 4.62 [0.38 to 121] |
MD, mean difference; RR, risk ratio; CrI, credible interval; ESIN, elastic stable intramedullary nail; F8B, figure-of-eight bandage; CRx, Sonoma CRx intramedullary nail; IMP, intramedullary pin.
Statistically significant.
Function
No statistically significant differences in function were found between treatments at ≤4 weeks, although plating was ranked highest (Table IV, Supplementary Fig. S2). For function at 6 weeks, both the ESIN and plating had significantly higher scores compared with the sling (Table IV; Fig. 4, a). At 12 weeks, scores were significantly higher with the CRx relative to the F8B (Table IV; Fig. 4, b). Function at 24 weeks was significantly lower with both the sling and F8B compared with the CRx, ESIN, and plating (Table IV; Fig. 4, c); the CRx also demonstrated significantly higher scores than the F8B-sling combination, IMP, and plating at this follow-up point. Both the CRx and plating showed significantly greater function than the sling at 52 weeks (Table IV; Fig. 4, d). At visits at >52 weeks, both the ESIN and plating showed significantly improved function relative to the sling (Table IV; Fig. 4, e).
Figure 4.
Forest plot of function at 6 weeks (a), 12 weeks (b), 24 weeks (c), 52 weeks (d), and >52 weeks (e) for midshaft clavicle fractures. CrI, credible interval; CRx, Sonoma CRx intramedullary nail; ESIN, elastic stable intramedullary nail; F8B, figure-of-8 bandage; F8B Sling, figure-of-8 bandage with sling; IMP, intramedullary pin.
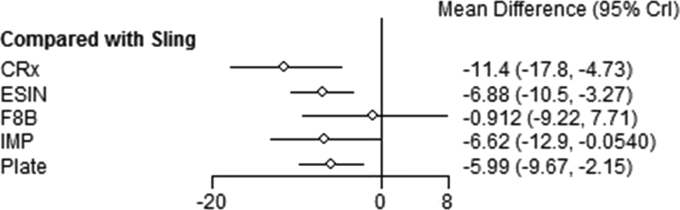
Time to radiographic union
The sling demonstrated a significantly later time to radiographic union relative to the CRx, ESIN, plating, and IMP (Table IV; Fig. 5). In addition, the CRx showed a significantly earlier time to union than the F8B.
Figure 5.
Forest plot of time to radiographic union for midshaft clavicle fractures. CrI, credible interval; CRx, Sonoma CRx intramedullary nail; ESIN, elastic stable intramedullary nail; F8B, figure-of-8 bandage; IMP, intramedullary pin.
Time to return to work
The ESIN was ranked highest for the outcome of time to return to work, but we did not find any statistically significant differences between the ESIN, F8B, plating, and sling (Table IV, Supplementary Fig. S3).
Delayed union
For delayed union, none of the pair-wise comparisons in this analysis were statistically significant, but plating was ranked highest (Table IV, Supplementary Fig. S4).
Malunion
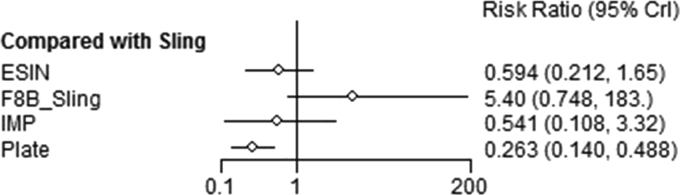
Plating demonstrated a significantly lower risk of malunion compared with both the sling and F8B-sling combination, whereas the ESIN had a significantly lower risk relative to the F8B-sling combination only (Table IV, Fig. 6).
Figure 6.
Forest plot of malunion for midshaft clavicle fractures. CrI, credible interval; ESIN, elastic stable intramedullary nail; F8B Sling, figure-of-8 bandage with sling; IMP, intramedullary pin.
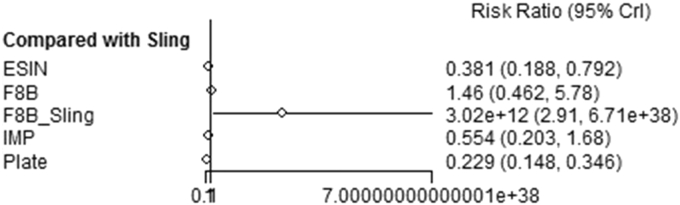
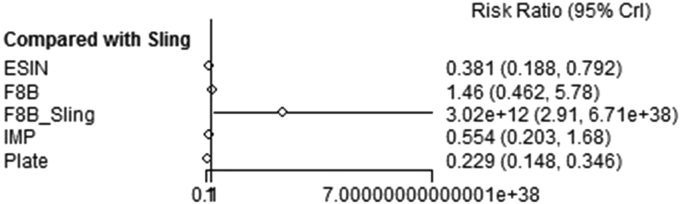
Nonunion
Both plating and the ESIN showed a significantly reduced risk of nonunion compared with the sling, F8B, and F8B-sling combination (Table IV, Fig. 7); plating was ranked highest. The IMP, sling alone, and F8B alone all had a significantly lower risk relative to the F8B-sling combination.
Figure 7.
Forest plot of nonunion for midshaft clavicle fractures. CrI, credible interval; ESIN, elastic stable intramedullary nail; F8B, figure-of-8 bandage; F8B Sling, figure-of-8 bandage with sling; IMP, intramedullary pin.
Refracture
We found no significant differences between the ESIN, IMP, plating, and sling for the incidence of refracture (Table IV, Supplementary Fig. S5).
Revision
There were no statistically significant differences between the ESIN, F8B, IMP, and plating in the risk of revision (Table IV, Supplementary Fig. S6).
Symptoms
In terms of persistent symptoms following treatment, no statistically significant differences were found between the CRx, ESIN, F8B, IMP, plating, and sling (Table IV, Supplementary Fig. S7).
Distal fractures
Function
We found no statistically significant results between interventions in functional scores at 3 months (Table V, Supplementary Fig. S8). CCSu was ranked highest, followed by the HP, CCSu-LP, LP, TB-KW, and finally, CCSc-LP.
Table V.
Effect estimates of all pair-wise comparisons for distal clavicle fractures
| Outcome | Comparison | MD or RR [95% CrI] |
|---|---|---|
| Function score (0-100) at 3 mo | CCSc-LP vs. CCSu | MD, −17.08 [−40.91 to 6.50] |
| CCSc-LP vs. CCSu-LP | MD, −10.00 [−23.05 to 2.90] | |
| CCSc-LP vs. HP | MD, −12.03 [−31.93 to 8.05] | |
| CCSc-LP vs. LP | MD, −9.33 [−27.77 to 9.04] | |
| CCSc-LP vs. TB-KW | MD, −5.60 [−19.25 to 8.05] | |
| CCSu vs. CCSu-LP | MD, 7.04 [−16.60 to 30.85] | |
| CCSu vs. HP | MD, 5.11 [−7.67 to 17.91] | |
| CCSu vs. LP | MD, 7.71 [−19.13 to 34.49] | |
| CCSu vs. TB-KW | MD, 11.50 [−7.82 to 30.75] | |
| CCSu-LP vs. HP | MD, −1.99 [−21.90 to 17.80] | |
| CCSu-LP vs. LP | MD, 0.66 [−12.30 to 13.56] | |
| CCSu-LP vs. TB-KW | MD, 4.39 [−9.25 to 18.02] | |
| HP vs. LP | MD, 2.65 [−20.93 to 26.38] | |
| HP vs. TB-KW | MD, 6.40 [−8.04 to 20.75] | |
| LP vs. TB-KW | MD, 3.72 [−15.07 to 22.30] | |
| Function score (0-100) at 6 mo | CCSc-LP vs. CCSu | MD, −8.14 [−22.79 to 6.63] |
| CCSc-LP vs. CCSu-LP | MD, −3.69 [−11.43 to 4.07] | |
| CCSc-LP vs. HP | MD, −4.51 [−17.27 to 8.09] | |
| CCSc-LP vs. TB-KW | MD, 1.01 [−7.95 to 9.91] | |
| CCSu vs. CCSu-LP | MD, 4.48 [−10.29 to 19.00] | |
| CCSu vs. HP | MD, 3.70 [−3.77 to 11.19] | |
| CCSu vs. TB-KW | MD, 9.15 [−2.42 to 20.70] | |
| CCSu-LP vs. HP | MD, −0.76 [−13.46 to 11.85] | |
| CCSu-LP vs. TB-KW | MD, 4.69 [−4.25 to 13.70] | |
| HP vs. TB-KW | MD, 5.47 [−3.49 to 14.36] | |
| Function score (0-100) at ≥1 yr | CCSc-LP vs. CCSu | MD, −3.09 [−12.00 to 5.57] |
| CCSc-LP vs. CCSu-KW | MD, 2.13 [−10.47 to 14.45] | |
| CCSc-LP vs. CCSu-LP | MD, −4.42 [−11.57 to 2.44] | |
| CCSc-LP vs. HP | MD, 0.15 [−7.83 to 8.09] | |
| CCSc-LP vs. KW | MD, 6.91 [−2.65 to 16.58] | |
| CCSc-LP vs. LP | MD, −4.92 [−13.41 to 3.41] | |
| CCSc-LP vs. TB-KW | MD, 1.45 [−6.13 to 8.70] | |
| CCSu vs. CCSu-KW | MD, 5.22 [−5.83 to 16.34] | |
| CCSu vs. CCSu-LP | MD, −1.37 [−8.69 to 6.01] | |
| CCSu vs. HP | MD, 3.22 [−0.55 to 7.20] | |
| CCSu vs. KW∗ | MD, 9.98 [2.86 to 17.52] | |
| CCSu vs. LP | MD, −1.78 [−8.35 to 4.68] | |
| CCSu vs. TB-KW | MD, 4.52 [−1.05 to 10.10] | |
| CCSu-KW vs. CCSu-LP | MD, −6.61 [−17.63 to 4.25] | |
| CCSu-KW vs. HP | MD, −1.99 [−12.37 to 8.52] | |
| CCSu-KW vs. KW | MD, 4.75 [−7.10 to 17.00] | |
| CCSu-KW vs. LP | MD, −7.03 [−16.11 to 1.90] | |
| CCSu-KW vs. TB-KW | MD, −0.72 [−11.64 to 10.23] | |
| CCSu-LP vs. HP | MD, 4.60 [−1.51 to 10.83] | |
| CCSu-LP vs. KW∗ | MD, 11.36 [3.11 to 19.84] | |
| CCSu-LP vs. LP | MD, −0.44 [−6.61 to 5.65] | |
| CCSu-LP vs. TB-KW | MD, 5.89 [−0.19 to 11.97] | |
| HP vs. KW∗ | MD, 6.74 [0.58 to 13.06] | |
| HP vs. LP | MD, −5.04 [−10.41 to 0.13] | |
| HP vs. TB-KW | MD, 1.32 [−2.84 to 5.14] | |
| KW vs. LP∗ | MD, −11.80 [−20.02 to −3.95] | |
| KW vs. TB-KW | MD, −5.45 [−12.11 to 0.95] | |
| LP vs. TB-KW∗ | MD, 6.36 [0.26 to 12.49] | |
| Time to radiographic union, wk | CCSc-LP vs. CCSu | MD, −7.57 [−27.81 to 12.10] |
| CCSc-LP vs. CCSu-LP | MD, 3.37 [−8.06 to 14.90] | |
| CCSc-LP vs. HP | MD, −3.75 [−20.40 to 12.78] | |
| CCSc-LP vs. KW | MD, −3.94 [−20.40 to 12.48] | |
| CCSc-LP vs. LP | MD, −4.53 [−24.85 to 12.72] | |
| CCSc-LP vs. TB-KW | MD, −3.34 [−15.76 to 9.03] | |
| CCSu vs. CCSu-LP | MD, 10.93 [−8.75 to 31.22] | |
| CCSu vs. HP | MD, 3.82 [−7.16 to 14.76] | |
| CCSu vs. KW | MD, 3.61 [−15.39 to 22.86] | |
| CCSu vs. LP | MD, 3.27 [−12.59 to 15.56] | |
| CCSu vs. TB-KW | MD, 4.26 [−11.30 to 19.90] | |
| CCSu-LP vs. HP | MD, −7.09 [−23.77 to 9.37] | |
| CCSu-LP vs. KW | MD, −7.28 [−23.67 to 9.13] | |
| CCSu-LP vs. LP | MD, −7.86 [−28.23 to 9.75] | |
| CCSu-LP vs. TB-KW | MD, −6.67 [−18.90 to 5.60] | |
| HP vs. KW | MD, −0.16 [−15.58 to 15.25] | |
| HP vs. LP | MD, −0.52 [−11.23 to 6.73] | |
| HP vs. TB-KW | MD, 0.45 [−10.65 to 11.36] | |
| KW vs. LP | MD, −0.36 [−19.96 to 15.57] | |
| KW vs. TB-KW | MD, 0.61 [−10.44 to 11.35] | |
| LP vs. TB-KW | MD, 1.00 [−11.49 to 16.90] | |
| Hardware complications | CCSu vs. CCSu-LP | RR, 1.43 [0.00 to 523] |
| CCSu vs. HP | RR, 2.03 [0.02 to 217] | |
| CCSu vs. KW | RR, 0.10 [0.00 to 24] | |
| CCSu vs. LP | RR, 1.45 [0.00 to 545] | |
| CCSu vs. TB-KW | RR, 0.73 [0.00 to 145] | |
| CCSu-LP vs. HP | RR, 1.40 [0.04 to 59] | |
| CCSu-LP vs. KW | RR, 0.07 [0.00 to 7.77] | |
| CCSu-LP vs. LP | RR, 1.03 [0.03 to 39] | |
| CCSu-LP vs. TB-KW | RR, 0.50 [0.01 to 43] | |
| HP vs. KW∗ | RR, 0.05 [0.00 to 0.93] | |
| HP vs. LP | RR, 0.72 [0.02 to 29] | |
| HP vs. TB-KW | RR, 0.35 [0.05 to 3.71] | |
| KW vs. LP | RR, 14 [0.13 to 1510] | |
| KW vs. TB-KW | RR, 6.69 [0.48 to 179] | |
| LP vs. TB-KW | RR, 0.49 [0.01 to 41] | |
| Nonunion | CCSc-LP vs. CCSu | RR, 0.76 [0.01 to 68] |
| CCSu-LP vs. CCSc-LP∗ | RR, 0.00 [0.00 to 0.97] | |
| CCSc-LP vs. HP | RR, 2.05 [0.03 to 156] | |
| CCSc-LP vs. KW | RR, 4.06 [0.03 to 608] | |
| LP vs. CCSc-LP∗ | RR, 0.00 [0.00 to 0.51] | |
| CCSc-LP vs. TB-KW | RR, 0.84 [0.02 to 44] | |
| CCSu-LP vs. CCSu∗ | RR, 0.00 [0.00 to 0.90] | |
| CCSu vs. HP | RR, 2.66 [0.64 to 15] | |
| CCSu vs. KW | RR, 5.26 [0.35 to 120] | |
| LP vs. CCSu∗ | RR, 0.00 [0.00 to 0.14] | |
| CCSu vs. TB-KW | RR, 1.12 [0.10 to 15] | |
| CCSu-LP vs. HP | RR, 0.00 [0.00 to 2.32] | |
| CCSu-LP vs. KW | RR, 0.00 [0.00 to 6.23] | |
| CCSu-LP vs. LP | RR, 6.36 [0.00 to 2.29 × 1020] | |
| CCSu-LP vs. TB-KW∗ | RR, 0.00 [0.00 to 0.77] | |
| HP vs. KW | RR, 1.95 [0.19 to 26] | |
| LP vs. HP∗ | RR, 0.00 [0.00 to 0.09] | |
| HP vs. TB-KW | RR, 0.42 [0.06 to 10] | |
| LP vs. KW∗ | RR, 0.00 [0.00 to 0.93] | |
| KW vs. TB-KW | RR, 0.21 [0.01 to 4.48] | |
| LP vs. TB-KW∗ | RR, 0.00 [0.00 to 0.19] | |
| Refracture | CCSu vs. CCSu-LP | RR, 2.44 [0.08 to 144] |
| CCSu vs. HP | RR, 0.76 [0.13 to 4.10] | |
| KW vs. CCSu∗ | RR, 0.00 [0.00 to 0.85] | |
| LP vs. CCSu∗ | RR, 0.00 [0.00 to 0.52] | |
| TB-KW vs. CCSu∗ | RR, 0.00 [0.00 to 0.00] | |
| CCSu-LP vs. HP | RR, 0.32 [0.01 to 5.53] | |
| KW vs. CCSu-LP | RR, 0.00 [0.00 to 4.26] | |
| LP vs. CCSu-LP | RR, 0.00 [0.00 to 1.82] | |
| TB-KW vs. CCSu-LP∗ | RR, 0.00 [0.00 to 0.00] | |
| KW vs. HP∗ | RR, 0.00 [0.00 to 0.57] | |
| LP vs. HP∗ | RR, 0.00 [0.00 to 0.34] | |
| TB-KW vs. HP∗ | RR, 0.00 [0.00 to 0.00] | |
| LP vs. KW | RR, 0.00 [0.00 to 9.55 × 109] | |
| TB-KW vs. KW∗ | RR, 0.00 [0.00 to 0.38] | |
| TB-KW vs. LP | RR, 0.00 [0.00 to 1.07 × 1015] | |
| Revision | CCSu vs. CCSc-LP | RR, 0.07 [0.00 to 40] |
| CCSu-LP vs. CCSc-LP∗ | RR, 0.00 [0.00 to 0.01] | |
| HP vs. CCSc-LP | RR, 0.08 [0.00 to 25] | |
| KW vs. CCSc-LP | RR, 0.11 [0.00 to 116] | |
| TB-KW vs. CCSc-LP | RR, 0.31 [0.01 to 13] | |
| CCSu-LP vs. CCSu∗ | RR, 0.00 [0.00 to 0.45] | |
| CCSu vs. HP | RR, 0.85 [0.04 to 14] | |
| CCSu vs. KW | RR, 0.64 [0.00 to 91] | |
| CCSu vs. TB-KW | RR, 0.23 [0.00 to 38] | |
| CCSu-LP vs. HP∗ | RR, 0.00 [0.00 to 0.28] | |
| CCSu-LP vs. KW∗ | RR, 0.00 [0.00 to 0.28] | |
| CCSu-LP vs. TB-KW∗ | RR, 0.00 [0.00 to 0.05] | |
| HP vs. KW | RR, 0.76 [0.01 to 45] | |
| HP vs. TB-KW | RR, 0.28 [0.00 to 21] | |
| KW vs. TB-KW | RR, 0.36 [0.00 to 130] | |
| Symptoms | CCSc-LP vs. CCSu∗ | RR, 0.00 [0.00 to 0.18] |
| CCSu-LP vs. CCSc-LP∗ | RR, 0.00 [0.00 to 0.01] | |
| CCSc-LP vs. HP | RR, 4.26 [0.12 to 198] | |
| CCSc-LP vs. TB-KW | RR, 1.80 [0.10 to 39] | |
| CCSu-LP vs. CCSu∗ | RR, 0.00 [0.00 to 0.00] | |
| HP vs. CCSu∗ | RR, 0.00 [0.00 to 0.03] | |
| TB-KW vs. CCSu∗ | RR, 0.00 [0.00 to 0.08] | |
| CCSu-LP vs. HP∗ | RR, 0.00 [0.00 to 0.07] | |
| CCSu-LP vs. TB-KW∗ | RR, 0.00 [0.00 to 0.03] | |
| HP vs. TB-KW | RR, 0.42 [0.05 to 3.32] |
MD, mean difference; RR, risk ratio; CrI, credible interval; CCSc, coracoclavicular screw fixation; LP, locking plate; CCSu, coracoclavicular suturing; HP, hook plate; TB, tension band; KW, K-wires.
Statistically significant.
For function at 6 months, we found no statistically significant differences between interventions (Table V, Supplementary Fig. S8). CCSu was again ranked highest, followed by CCSu-LP, the HP, CCSc-LP, and TB-KW.
For function at follow-up ≥ 1 year, we noted statistically significant findings between some of the pair-wise comparisons (Table V, Fig. 8). KW demonstrated significantly worse outcomes than CCSu, CCSu-LP, the HP, and the LP; the LP was also significantly better than TB-KW. The corresponding SUCRA values were 87% for the LP, 83% for CCSu-LP, 73% for CCSu, 45% for CCSc-LP, 43% for the HP, 32% for CCSu-KW, 31% for TB-KW, and 5% for KW.
Figure 8.
Forest plot of function at ≥1 year for distal clavicle fractures. CrI, credible interval; CCSu, coracoclavicular suturing; CCSc, coracoclavicular screw fixation; LP, locking plate; KW, K-wires; HP, hook plate; TB, tension band.
Time to radiographic union
We did not find any significant differences in the time to radiographic union between treatments (Table V, Supplementary Fig. S9). CCSu-LP was ranked highest for this outcome, followed by CCSc-LP, TB-KW, the HP, KW, the LP, and finally, CCSu.
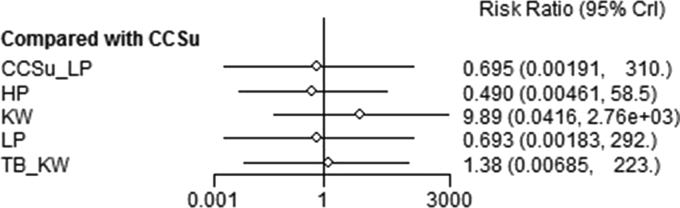
Hardware complications
There was 1 statistically significant comparison, demonstrating that KW resulted in a greater risk of hardware complications than the HP (Table V, Fig. 9). The corresponding SUCRA values were 73% for the HP, 60% for the LP, 60% for CCSu-LP, 53% for CCSu, 45% for TB-KW, and 10% for KW.
Figure 9.
Forest plot of hardware complications for distal clavicle fractures. CrI, credible interval; CCSu, coracoclavicular suturing; LP, locking plate; HP, hook plate; KW, K-wires; TB, tension band.
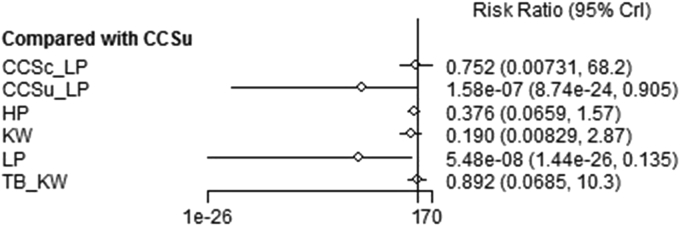
Nonunion
Both the LP and CCSu-LP had significantly lower risks of nonunion compared with each of the following: CCSc-LP, TB-KW, HP, CCSu, and sling (Table V, Fig. 10). Only the LP showed a significantly lower risk of this event relative to KW. The LP and CCSu-LP had the highest SUCRA values, at 91% and 88%, respectively, followed by KW (55%), the HP (45%), CCSc-LP (30%), TB-KW (22%), and finally, CCSu (19%).
Figure 10.
Forest plot of nonunion for distal clavicle fractures. CrI, credible interval; CCSu, coracoclavicular suturing; CCSc, coracoclavicular screw fixation; LP, locking plate; HP, hook plate; KW, K-wires; TB, tension band.
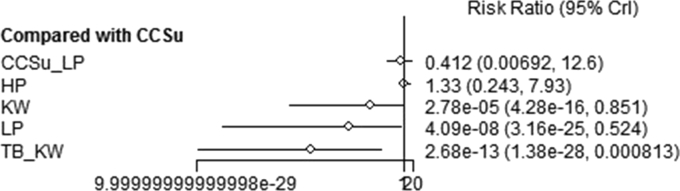
Refracture
TB-KW demonstrated a significantly lower risk of refracture compared with CCSu, CCSu-LP, the HP, and KW; both the LP and KW had significantly lower risks relative to CCSu and the HP (Table V, Fig. 11). The SUCRA values were 94% for TB-KW, 77% for the LP, 65% for KW, 32% for CCSu-LP, 19% for CCSu, and 12% for the HP.
Figure 11.
Forest plot of refracture for distal clavicle fractures. CrI, credible interval; CCSu, coracoclavicular suturing; LP, locking plate; HP, hook plate; KW, K-wires; TB, tension band.
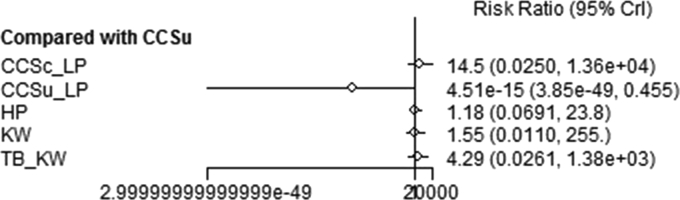
Revision
Regarding the risk of revision, CCSu-LP demonstrated a significantly lower risk than all other interventions included in the analysis (Table V, Fig. 12). The SUCRA values were 99% for CCSu-LP, 55% for CCSu, 52% for the HP, 46% for KW, 33% for TB-KW, and 14% for CCSc-LP.
Figure 12.
Forest plot of revision for distal clavicle fractures. CrI, credible interval; CCSu, coracoclavicular suturing; CCSc, coracoclavicular screw fixation; LP, locking plate; HP, hook plate; KW, K-wires; TB, tension band.
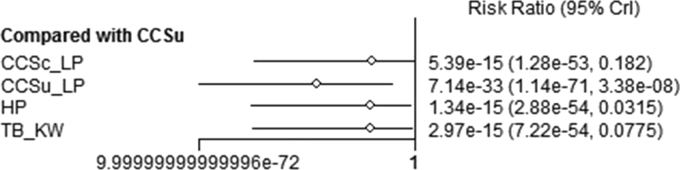
Symptoms
In the analysis of persistent symptoms, CCSu-LP showed a significantly lower risk than CCSc-LP, CCSu, the HP, and TB-KW; CCSc-LP, the HP, and TB-KW each had a significantly lower risk compared with CCSu only (Table V, Fig. 13). The corresponding SUCRA values were 99% for CCSu-LP, 69% for the HP, 47% for TB-KW, 33% for CCSc-LP, and 0.3% for CCSu.
Figure 13.
Forest plot of symptoms for distal clavicle fractures. CrI, credible interval; CCSu, coracoclavicular suturing; CCSc, coracoclavicular screw fixation; LP, locking plate; HP, hook plate; TB, tension band; KW, K-wires.
Medial fractures
Across all studies on patients with medial fractures, 85 patients were managed with a sling, 57 were treated with plating, 2 received TB, 1 was treated with KW, and 1 received a screw and suturing.
Pain
The visual analog scale (VAS) scores for pain on activity following nonoperative therapy in the study by Bartonicek et al5 were 1 of 10 for 1 patient and 2 of 10 for the other patient at 18 and 13 months, respectively. Regarding plating, in the case reports by Li et al49, 81, 88 and Smelt et al49, 81, 88, the patients reported no pain at 2 and 8 weeks, respectively, whereas the patient in the report by Teng and Liu49, 81, 88 still had pain at 6 months, although a nonunion was also diagnosed in this patient. Low et al51, 109 showed an average VAS score for pain on activity of 0.75 of 10 at a mean follow-up of 3.3 years (range, 8 months to 10 years) for patients treated with plating, whereas Zheng et al51, 109 reported average scores of 3.4, 3, and 2.1 at 3, 6, and 12 months, respectively. The final VAS score was 0 for both patients who had TB in the study by Bartonicek et al5. The patient treated with KW in the report by Bourghli and Fabre8 had no pain by 3 months. The patient treated with a screw and sutures had a VAS score of 0.75 at latest follow-up.51
Function
The 2 patients managed nonoperatively in the study by Bartonicek et al5 had Disabilities of the Arm, Shoulder and Hand (DASH) scores of 27.1 at 18 months and 33.3 at 13 months. Among studies that examined plating, 1 case report found a DASH score of 23.33 at 8 weeks49 whereas the average DASH and QuickDASH (short version of DASH questionnaire) scores at later follow-up assessments (approximately 1 year or later) ranged from 8.6 to 13.551,63,105 and from 0.66 to 0.81,23,89 respectively.; The DASH scores of the 2 patients treated with TB were 25.8 (at 2 years) and 24.2 (at 18 months).5 The patient treated with a screw and sutures had a DASH score of 9 at latest follow-up.51
Return to work or activities
Studies investigating plating reported that all patients returned to their preinjury level of work or activity following treatment.51,76,89,99 The patient treated with KW was able to return to work by 8 months.8 The patient treated with a screw and suturing also returned to the previous occupation and activity level.51
Radiographic union
Regarding patients managed nonoperatively, Robinson et al67, 95 found a nonunion in 2 of 24 patients at the 24-week follow-up, and there were 4 nonunions and 1 malunion among the 55 patients investigated by Van Tongel et al67, 95; however, all 4 patients in the study of Singh et al78 had a successfully united fracture. Most plating studies reported successful union among all patients,23,51,76,89,99,105,109 but there were 2 exceptions: The patient in the report by Teng and Liu63, 88 experienced a nonunion at 6 months after plating, and a nonunion occurred in 1 of 9 patients in the study by Oe et al63, 88. The patient treated with KW had complete union by 3 months.8 The case treated with a screw and suturing had successful union as well.51
Other complications
Bartonicek et al5 reported 1 case of clavicle shortening in a patient treated nonoperatively. In the study by Frima et al23, plating caused implant irritation in 8 of 15 patients, leading to implant removal in 7, and there was also 1 case of implant failure and deep infection that required revision surgery. The patient treated with a plate in the case report by Teng and Liu88, 109 underwent revision for nonunion with a partial claviculectomy, and Zheng et al88, 109 encountered a redislocation of the sternoclavicular joint in 1 patient (of 12), but this occurred after plate removal. In contrast, other studies on plating revealed no complications or revisions following the procedure.51,76,89,105 Bartonicek et al also reported slight hypertrophy of the medial clavicle in a patient managed with TB at the 2-year follow-up. No complications were reported in the case treated with a screw and suturing.51
Discussion
Midshaft fractures
Operative interventions showed significant improvements over nonoperative methods in terms of early and long-term function, time to radiographic union, and reduction in certain complications. Specifically, plating, the ESIN, and the CRx consistently demonstrated more favorable function than nonoperative therapies over time; the IMP also showed greater function than nonoperative treatments from 6 weeks onward, but its effects were never statistically significant. Moreover, operative treatments demonstrated a significantly earlier time to radiographic union than the sling. Therefore, for patients who seek a quicker recovery, operating would be the best approach. Plating, the IMP, and the ESIN also showed lower risks of nonunion and malunion relative to nonoperative therapies, but only plating had a statistically significant effect compared with each nonoperative treatment. Of note, there were no data for the CRx to include in the analyses of nonunion and malunion. Though not statistically significant, our analysis also revealed that although plating was associated with an increase in ongoing symptoms, except compared with the ESIN, it also had the least risk of a delayed union and revision surgery. Plating showed significant improvements in the greatest number of comparisons across multiple outcomes, followed by the ESIN. The CRx also showed promise as a treatment; however, there is currently limited evidence on this method. Although the IMP similarly showed some statistically significant findings, its effects were not as impressive.
Prior reviews have also demonstrated that operative interventions show improvements over nonoperative treatments in terms of functional outcomes, time to union, and fewer complications, such as nonunion.16,66,96 Virtanen et al96 found that the results of surgery showed better function and a lower likelihood of delayed union and nonunion. Duan et al16 suggested that plating results in fewer complications and more satisfaction than use of a sling. More recently, Rehn et al66 found that nonoperatively treated patients had more nonunions but that operative intervention may increase the risk of minor complications.
In a review, Wang et al98 suggested that treatment with intramedullary (IM) implants, compared with plating and nonoperative treatment, is the optimal approach. However, they grouped all nonoperative therapies (ie, sling and F8B) and all the various IM devices (ie, IMP and ESIN), and these conclusions were based on nonunion and infection rates, which were higher with plating than with IM fixation but not statistically significant. Jiang et al33 conducted a network meta-analysis on function and also suggested that IM fixation resulted in more favorable outcomes, but they grouped treatments in a similar fashion to Wang et al (ie, any IM device) and only included studies that used the Constant-Murley score.
Distal fractures
We found that functional improvement at earlier visits may be best achieved with CCSu, although these results were not statistically significant. At ≥1 year, functional scores were significantly worse with KW than with CCSu, CCSu-LP, the HP, and the LP, whereas functional scores with TB-KW were significantly worse than with the LP only. Of note, CCSu-LP was ranked third and second at 3 and 6 months, respectively, and there were no functional data for the LP at 6 months. No significant findings were observed for time to radiographic union, but CCSu-LP showed the earliest time to union and CCSu alone resulted in the longest time. The HP demonstrated the least risk of hardware problems, but this was only significant compared with KW, and the LP and CCSu-LP were ranked second and third, respectively, in this analysis. The risk of a nonunion was most favorable with the LP and CCSu-LP, whereas the sling and CCSu were ranked lowest for this outcome. The LP was ranked second, after TB-KW, for the risk of refracture, whereas CCSu and the HP were ranked lowest. For both the risk of reoperation and symptomatic hardware, CCSu-LP was ranked highest with significantly lower risks than with all other interventions (there were no data for locked plating alone to include in these analyses); CCSu was ranked lowest and had a significantly higher risk of symptomatic hardware compared with all other treatments. Such results suggest that, for early and sustained functional improvement and limited complications, the LP with or without CCSu may provide the most optimal outcome. CCSu alone and the HP may be viable alternatives as well, although CCSu alone appears to be associated with union-related issues and continued symptoms, and both CCSu alone and the HP may have a higher likelihood of refracture.
The network meta-analysis by Boonard et al7 on distal fractures included 11 studies and evaluated (1) coracoclavicular (CC) fixation, (2) an HP, (3) an LP, (4) TB, and (5) KW. Similarly to our analysis, the authors concluded that CC fixation and the LP were better than both the HP and TB for function and that the LP was associated with a lower risk of complications. Although we came to the same general conclusions, there were some differences in our methodology. First, Boonard et al did not consider some treatments as combination therapies, such as CC fixation with an LP and TB with KW. We considered each combination therapy a treatment node to ensure the effects were exclusively attributed to each unique therapy. Second, Boonard et al analyzed different functional measures separately (ie, Constant-Murley and UCLA scores) and did not evaluate function across different time points. We converted functional measures to a common scale and analyzed these data at 3 months, 6 months, and ≥1 year to determine differences occurred over time. Finally, Boonard et al evaluated the risk of any complication, whereas we assessed specific complications to determined whether particular events were more—or less—likely following a particular treatment.
Medial fractures
Plating appears to be associated with better functional scores than both the sling and TB. In addition, plating, a screw and suturing, and KW were positively associated with a patient's return to his or her previous occupation or activity level; however, the latter 2 treatments were limited to evidence from case reports. Surgical intervention also appears to lessen the risk of nonunion and malunion relative to nonoperative therapy. With plating, the most common complaint in 1 study was implant irritation, which led to subsequent implant removal, and there were also 2 cases that underwent revision; however, other studies reported no complications or revisions following plating. The authors of some studies indicated why they selected certain treatments, suggesting that they may have preferred another treatment under other circumstances. Bourghli and Fabre8 stated that they used KW instead of plating because the fracture was too severely comminuted. Low et al51 used a screw and suturing instead of plating because the patient had poor bone stock. The patients treated nonoperatively in the study by Bartonicek et al5 were deemed unfit for surgery: Both patients were elderly, and 1 underwent a prior coronary bypass and the other was a heavy drinker. In other cases, the surgeon chose TB instead of plating because the medial fragment in these patients was too short and there was inadequate bone stock.
The evidence on medial fractures is very limited. Part of the reason for this may be its extremely low prevalence, representing <3% of clavicle fractures.72 Our review suggests that plating, given the proper indications, offers the best outcome; however, implant irritation can occur, which is usually resolved with implant removal. Other surgical procedures (ie, TB, KW, screws and suturing) seem to perform well too, but these options may only be preferred in situations in which plating is contraindicated, and the evidence on these treatments is limited to just a few case reports.
Strengths and limitations
Our review differentiated between clavicle fracture types (ie, midshaft, distal, and medial) as they are not the same injury. We conducted a comprehensive comparative analysis, for midshaft and distal fractures, of various interventions. We also examined numerous outcomes to best inform treatment decisions when weighing the risks and benefits of these therapies. We were very specific in our categorization of interventions, including combination therapies, so that our results were less likely to be confounded by variations in treatment techniques or characteristics.
A disadvantage of our study is that it includes mostly low-quality studies; however, this is reflective of the current state of the evidence and highlights the need for more high-quality trials. Moreover, because of the limited data, the precision around the effect estimates was very low, and the inclusion of additional evidence in the future may impact the results. In addition, for medial fractures, we found no studies directly comparing treatments, meaning that our conclusions were based on case series and case reports and we could not compare these treatments via a meta-analysis. Another consideration is that fracture characteristics (pattern, stability, amount of displacement, and so on) can play a role in treatment decisions; thus, these data may not be applicable to every patient who sustains a clavicle fracture. The availability of or preference for some of these interventions in certain geographic regions can also influence the applicability of our results. For example, none of the studies evaluating the ESIN for midshaft fractures were conducted in North America. Hence, it is difficult to determine whether the ESIN would be a viable option for North American patients, as their physical characteristics and behaviors may be different from those of patients from other countries; North American surgeons may see less promising results with the ESIN in their patients. Finally, we only included articles published in English and therefore may have missed studies published in other languages.
Conclusion
This study provides evidence to inform treatment decisions for midshaft, distal, and medial clavicle fractures; however, additional high-quality evidence would be impactful. More specifically, future studies should be large (ie, greater sample sizes), multicenter randomized trials. The current evidence suggests that surgery with plating, surgery with an ESIN, and surgery with a CRx are all good options for midshaft fractures; an LP with or without CC suturing should be preferred for distal fractures; and plating is also acceptable for medial fractures, provided that the patient is deemed suitable for surgery and has the adequate bone stock and sufficiently sized medial fragment necessary to implant the device. Patient preferences for certain outcomes should be considered, which may result in different treatment recommendations.
Disclaimer
This study was funded by a research grant from Acumed.
Christopher Vannabouathong is an employee of OrthoEvidence, which received the grant.
Mohit Bhandari receives consulting fees from Acumed.
Michael D. McKee receives royalties from Stryker
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this systematic review.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2020.01.010.
Supplementary Data
References
- 1.Ahrens P.M., Garlick N.I., Barber J., Tims E.M. The clavicle trial: a multicenter randomized controlled trial comparing operative with nonoperative treatment of displaced midshaft clavicle fractures. J Bone Joint Surg Am. 2017;99:1345–1354. doi: 10.2106/JBJS.16.01112. [DOI] [PubMed] [Google Scholar]
- 2.Andersen K., Jensen P.O., Lauritzen J. Treatment of clavicular fractures. Figure-of-eight bandage versus a simple sling. Acta Orthop Scand. 1987;58:71–74. doi: 10.3109/17453678709146346. [DOI] [PubMed] [Google Scholar]
- 3.Andrade-Silva F.B., Kojima K.E., Joeris A., Santos Silva J., Mattar R. Single, superiorly placed reconstruction plate compared with flexible intramedullary nailing for midshaft clavicular fractures: a prospective, randomized controlled trial. J Bone Joint Surg Am. 2015;97:620–626. doi: 10.2106/JBJS.N.00497. [DOI] [PubMed] [Google Scholar]
- 4.Assobhi J.E. Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures. J Orthop Traumatol. 2011;12:185–192. doi: 10.1007/s10195-011-0158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartonicek J., Fric V., Pacovsky V. Displaced fractures of the medial end of the clavicle: report of five cases. J Orthop Trauma. 2010;24:e31–e35. doi: 10.1097/BOT.0b013e3181aa5505. [DOI] [PubMed] [Google Scholar]
- 6.Bhardwaj A., Sharma G., Patil A., Rahate V. Comparison of plate osteosynthesis versus non-operative management for mid-shaft clavicle fractures—a prospective study. Injury. 2018;49:1104–1107. doi: 10.1016/j.injury.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Boonard M., Sumanont S., Arirachakaran A., Sikarinkul E., Ratanapongpean P., Kanchanatawan W. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28:1065–1078. doi: 10.1007/s00590-018-2187-x. [DOI] [PubMed] [Google Scholar]
- 8.Bourghli A., Fabre A. Proximal end clavicle fracture from a parachute jumping injury. Orthop Traumatol Surg Res. 2012;98:238–241. doi: 10.1016/j.otsr.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Calbiyik M., Ipek D., Taskoparan M. Prospective randomized study comparing results of fixation for clavicular shaft fractures with intramedullary nail or locking compression plate. Int Orthop. 2017;41:173–179. doi: 10.1007/s00264-016-3192-5. [DOI] [PubMed] [Google Scholar]
- 10.Chen C.Y., Yang S.W., Lin K.Y., Lin K.C., Tarng Y.W., Renn J.H. Comparison of single coracoclavicular suture fixation and hook plate for the treatment of acute unstable distal clavicle fractures. J Orthop Surg Res. 2014;9:42. doi: 10.1186/1749-799x-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen L., Chen H., Nisar M., Chen H., Pan J., Peng L. A retrospective comparison of minimally invasive percutaneous plate osteosynthesis (MIPPO) and minimally invasive percutaneous titanium elastic nail osteosynthesis (MIPTENO) for midshaft clavicle fracture. Int J Clin Exp Med. 2018;11:870–876. [Google Scholar]
- 12.Chen Q.Y., Kou D.Q., Cheng X.J., Zhang W., Wang W., Lin Z.Q. Intramedullary nailing of clavicular midshaft fractures in adults using titanium elastic nail. Chin J Traumatol. 2011;14:269–276. [PubMed] [Google Scholar]
- 13.Chen Y.-F., Wei H.-F., Zhang C., Zeng B.-F., Zhang C.-Q., Xue J.-F. Retrospective comparison of titanium elastic nail (TEN) and reconstruction plate repair of displaced midshaft clavicular fractures. J Shoulder Elbow Surg. 2012;21:495–501. doi: 10.1016/j.jse.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Chu J.Y., Yeh K.T., Lee R.P., Yu T.C., Chen I.H., Peng C.H. Open reduction and internal fixation with plating is beneficial in the early recovery stage for displaced midshaft clavicular fractures in patients aged 30-65 years old. Tzu Chi Med J. 2018;30:242–246. doi: 10.4103/tcmj.tcmj_25_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coppa V., Dei Giudici L., Cecconi S., Marinelli M., Gigante A. Midshaft clavicle fractures treatment: threaded Kirschner wire versus conservative approach. Strategies Trauma Limb Reconstr. 2017;12:141–150. doi: 10.1007/s11751-017-0293-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duan X., Zhong G., Cen S., Huang F., Xiang Z. Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2011;20:1008–1015. doi: 10.1016/j.jse.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 17.Eden L., Ziegler D., Gilbert F., Fehske K., Fenwick A., Meffert R.H. Significant pain reduction and improved functional outcome after surgery for displaced midshaft clavicular fractures. J Orthop Surg Res. 2015;10:190. doi: 10.1186/s13018-015-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erdle B., Izadpanah K., Jaeger M., Jensen P., Konstantinidis L., Zwingmann J. Comparative analysis of locking plate versus hook plate osteosynthesis of Neer type IIB lateral clavicle fractures. Arch Orthop Trauma Surg. 2017;137:651–662. doi: 10.1007/s00402-017-2645-7. [DOI] [PubMed] [Google Scholar]
- 19.Ersen A., Atalar A.C., Birisik F., Saglam Y., Demirhan M. Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures: a randomised controlled study. Bone Joint J. 2015;97-B:1562–1565. doi: 10.1302/0301-620X.97B11.35588. [DOI] [PubMed] [Google Scholar]
- 20.Ferran N.A., Hodgson P., Vannet N., Williams R., Evans R.O. Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg. 2010;19:783–789. doi: 10.1016/j.jse.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Flinkkila T., Heikkila A., Sirnio K., Pakarinen H. TightRope versus clavicular hook plate fixation for unstable distal clavicular fractures. Eur J Orthop Surg Traumatol. 2015;25:465–469. doi: 10.1007/s00590-014-1526-9. [DOI] [PubMed] [Google Scholar]
- 22.Flinkkila T., Ristiniemi J., Hyvonen P., Hamalainen M. Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand. 2002;73:50–53. doi: 10.1080/000164702317281404. [DOI] [PubMed] [Google Scholar]
- 23.Frima H., Houwert R.M., Sommer C. Displaced medial clavicle fractures: operative treatment with locking compression plate fixation. Eur J Orthop Surg Traumatol. 2018;11:11. doi: 10.1007/s00068-018-1024-6. [DOI] [PubMed] [Google Scholar]
- 24.Fu T.H., Tan B.L., Liu H.C., Wang J.W. Anatomical reduction for treatment of displaced midshaft clavicular fractures: Knowles pinning vs reconstruction plating. Orthopedics. 2012;35:e23–e30. doi: 10.3928/01477447-20111122-05. [DOI] [PubMed] [Google Scholar]
- 25.Fuglesang H.F.S., Flugsrud G.B., Randsborg P.H., Oord P., Benth J., Utvåg S.E. Plate fixation versus intramedullary nailing of completely displaced midshaft fractures of the clavicle: a prospective randomised controlled trial. Bone Joint J. 2017;99-B:1095–1101. doi: 10.1302/0301-620X.99B8.BJJ-2016-1318.R1. [DOI] [PubMed] [Google Scholar]
- 26.Hanselman A.E., Murphy T.R., Bal G.K., McDonough E.B. Operative cost comparison: plating versus intramedullary fixation for clavicle fractures. Orthopedics. 2016;39:e877–e882. doi: 10.3928/01477447-20160517-04. [DOI] [PubMed] [Google Scholar]
- 27.Hill J.M., McGuire M.H., Crosby L.A. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537–539. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 28.Houwert R.M., Smeeing D.P.J., Ahmed Ali U., Hietbrink F., Kruyt M.C., van der Meijden O.A. Plate fixation or intramedullary fixation for midshaft clavicle fractures: a systematic review and meta-analysis of randomized controlled trials and observational studies. J Shoulder Elbow Surg. 2016;25:1195–1203. doi: 10.1016/j.jse.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 29.Hsu K.-H., Tzeng Y.-H., Chang M.-C., Chiang C.-C. Comparing the coracoclavicular loop technique with a hook plate for the treatment of distal clavicle fractures. J Shoulder Elbow Surg. 2018;27:224–230. doi: 10.1016/j.jse.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 30.Hsu T.L., Hsu S.K., Chen H.M., Wang S.T. Comparison of hook plate and tension band wire in the treatment of distal clavicle fractures. Orthopedics. 2010;33:879. doi: 10.3928/01477447-20101021-04. [DOI] [PubMed] [Google Scholar]
- 31.Hulsmans M.H., van Heijl M., Houwert R.M., Burger B.J., Verleisdonk E.J.M., Veeger D.J. Surgical fixation of midshaft clavicle fractures: a systematic review of biomechanical studies. Injury. 2018;49:753–765. doi: 10.1016/j.injury.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 32.Hussain N., Sermer C., Prusick P.J., Banfield L., Atrey A., Bhandari M. Intramedullary nailing versus plate fixation for the treatment displaced midshaft clavicular fractures: a systematic review and meta-analysis. Sci Rep. 2016;6:34912. doi: 10.1038/srep34912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang W., Wang H., Li Y.S., Zhou T.J., Hu X.J. Meta-analysis of differences in Constant-Murley scores for three mid-shaft clavicular fracture treatments. Oncotarget. 2017;8:83251–83260. doi: 10.18632/oncotarget.18456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jones L.D., Grammatopoulos G., Kambouroglou G. Titanium elastic nails, open reduction internal fixation and non-operative management for middle third clavicle fractures: a comparative study. Eur J Orthop Surg Traumatol. 2014;24:323–329. doi: 10.1007/s00590-013-1191-4. [DOI] [PubMed] [Google Scholar]
- 35.Judd D.B., Pallis M.P., Smith E., Bottoni C.R. Acute operative stabilization versus nonoperative management of clavicle fractures. Am J Orthop (Belle Mead NJ) 2009;38:341–345. [PubMed] [Google Scholar]
- 36.Khan L.A., Bradnock T.J., Scott C., Robinson C.M. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91:447–460. doi: 10.2106/jbjs.h.00034. [DOI] [PubMed] [Google Scholar]
- 37.Khorami M., Fakour M., Mokarrami H., Arti H.R., Nasab A.M., Shahrivar F. The comparison of results of treatment of midshaft clavicle fracture between operative treatment with plate and non-operative treatment. Arch Bone Joint Surg. 2014;2:210–214. [PMC free article] [PubMed] [Google Scholar]
- 38.King P.R., Ikram A., Eken M.M., Lamberts R.P. The effectiveness of a flexible locked intramedullary nail and an anatomically contoured locked plate to treat clavicular shaft fractures: a 1-year randomized control trial. J Bone Joint Surg Am. 2019;101:628–634. doi: 10.2106/jbjs.18.00660. [DOI] [PubMed] [Google Scholar]
- 39.Klein S.M., Badman B.L., Keating C.J., Devinney D.S., Frankle M.A., Mighell M.A. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19:1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 40.Kleweno C.P., Jawa A., Wells J.H., O'Brien T.G., Higgins L.D., Harris M.B. Midshaft clavicular fractures: comparison of intramedullary pin and plate fixation. J Shoulder Elbow Surg. 2011;20:1114–1117. doi: 10.1016/j.jse.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 41.Kulshrestha V., Roy T., Audige L. Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. J Orthop Trauma. 2011;25:31–38. doi: 10.1097/BOT.0b013e3181d8290e. [DOI] [PubMed] [Google Scholar]
- 42.Lazarides S., Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg. 2006;15:191–194. doi: 10.1016/j.jse.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 43.Lechler P., Sturm S., Boese C.K., Bockmann B., Schwarting T., Ruchholtz S. Surgical complications following ESIN for clavicular mid-shaft fractures do not limit functional or patient-perceived outcome. Injury. 2016;47:899–903. doi: 10.1016/j.injury.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 44.Lee Y.S., Huang H.L., Lo T.Y., Hsieh Y.F., Huang C.R. Surgical treatment of midclavicular fractures: a prospective comparison of Knowles pinning and plate fixation. Int Orthop. 2008;32:541–545. doi: 10.1007/s00264-007-0352-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee Y.S., Lau M.J., Tseng Y.C., Chen W.C., Kao H.Y., Wei J.D. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33:1401–1405. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee Y.S., Lin C.C., Huang C.R., Chen C.N., Liao W.Y. Operative treatment of midclavicular fractures in 62 elderly patients: Knowles pin versus plate. Orthopedics. 2007;30:959–964. doi: 10.3928/01477447-20071101-13. [DOI] [PubMed] [Google Scholar]
- 47.Lenza M., Faloppa F. Surgical interventions for treating acute fractures or non-union of the middle third of the clavicle. Cochrane Database Syst Rev. 2015:CD007428. doi: 10.1002/14651858.CD007428.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leu T.H., Ho W.P., Wong P.K., Chuang T.Y., Wong C.C. Clavicular hook plate: a better implant choice for fixation of unstable distal clavicle fractures? J Exp Clin Med. 2012;4:270–274. doi: 10.1016/j.jecm.2012.09.002. [DOI] [Google Scholar]
- 49.Li Z., Liu H., Chen D., Chen C., Zhang Y., Xue E. A new technique for medial-end comminuted clavicle fractures. Injury. 2019;69:E82–E87. doi: 10.1016/j.injury.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 50.Liu H.H., Chang C.H., Chia W.T., Chen C.H., Tarng Y.W., Wong C.Y. Comparison of plates versus intramedullary nails for fixation of displaced midshaft clavicular fractures. J Trauma. 2010;69:E82–E87. doi: 10.1097/TA.0b013e3181e03d81. [DOI] [PubMed] [Google Scholar]
- 51.Low A.K., Duckworth D.G., Bokor D.J. Operative outcome of displaced medial-end clavicle fractures in adults. J Shoulder Elbow Surg. 2008;17:751–754. doi: 10.1016/j.jse.2008.01.139. [DOI] [PubMed] [Google Scholar]
- 52.Martel L. Recent changes in demographic trends in Canada Government of Canada—Statistics Canada. 2017. https://www150.statcan.gc.ca/n1/pub/75-006-x/2015001/article/14240-eng.htm
- 53.Mbuagbaw L., Rochwerg B., Jaeschke R., Heels-Andsell D., Alhazzani W., Thabane L. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev. 2017;6:79. doi: 10.1186/s13643-017-0473-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McKee M.D., Kreder H.J., Mandel S., McCormack R., Reindl R., Pugh D.M.W. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 55.McKee R.C., Whelan D.B., Schemitsch E.H., McKee M.D. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94:675–684. doi: 10.2106/JBJS.J.01364. [DOI] [PubMed] [Google Scholar]
- 56.Melean P.A., Zuniga A., Marsalli M., Fritis N.A., Cook E.R., Zilleruelo M. Surgical treatment of displaced middle-third clavicular fractures: a prospective, randomized trial in a working compensation population. J Shoulder Elbow Surg. 2015;24:587–592. doi: 10.1016/j.jse.2014.11.041. [DOI] [PubMed] [Google Scholar]
- 57.Mirzatolooei F. Comparison between operative and nonoperative treatment methods in the management of comminuted fractures of the clavicle. Acta Orthop Traumatol Turc. 2011;45:34–40. doi: 10.3944/AOTT.2011.2431. [DOI] [PubMed] [Google Scholar]
- 58.Napora J.K., Grimberg D.C., Childs B.R., Vallier H.A. Results and outcomes after midshaft clavicle fracture: matched pair analysis of operative versus nonoperative management. Orthopedics. 2018;41:E689–E694. doi: 10.3928/01477447-20180724-04. [DOI] [PubMed] [Google Scholar]
- 59.Narsaria N., Singh A.K., Arun G.R., Seth R.R. Surgical fixation of displaced midshaft clavicle fractures: elastic intramedullary nailing versus precontoured plating. J Orthop Traumatol. 2014;15:165–171. doi: 10.1007/s10195-014-0298-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Naveen B.M., Joshi G.R., Harikrishnan B. Management of mid-shaft clavicular fractures: comparison between non-operative treatment and plate fixation in 60 patients. Strategies Trauma Limb Reconstr. 2017;12:11–18. doi: 10.1007/s11751-016-0272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Neer C.S., II Nonunion of the clavicle. JAMA. 1960;172:1006–1011. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 62.Ni M., Niu W., Wong D.W., Zeng W., Mei J., Zhang M. Finite element analysis of locking plate and two types of intramedullary nails for treating mid-shaft clavicle fractures. Injury. 2016;47:1618–1623. doi: 10.1016/j.injury.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 63.Oe K., Gaul L., Hierholzer C., Woltmann A., Miwa M., Kurosaka M. Operative management of periarticular medial clavicle fractures—report of 10 cases. J Trauma Acute Care Surg. 2012;72:E1–E7. doi: 10.1097/TA.0b013e31820d1354. [DOI] [PubMed] [Google Scholar]
- 64.Postacchini F., Gumina S., De Santis P., Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 65.Qvist A.H., Væsel M.T., Jensen C.M., Jensen S.L. Plate fixation compared with nonoperative treatment of displaced midshaft clavicular fractures: a randomized clinical trial. Bone Joint J. 2018;100-B:1385–1391. doi: 10.1302/0301-620X.100B10.BJJ-2017-1137.R3. [DOI] [PubMed] [Google Scholar]
- 66.Rehn C.-H., Kirkegaard M., Viberg B., Larsen M.S. Operative versus nonoperative treatment of displaced midshaft clavicle fractures in adults: a systematic review. Eur J Orthop Surg Traumatol. 2014;24:1047–1053. doi: 10.1007/s00590-013-1370-3. [DOI] [PubMed] [Google Scholar]
- 67.Robinson C.M., Court-Brown C.M., McQueen M.M., Wakefield A.E. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86:1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 68.Robinson C.M., Goudie E.B., Murray I.R., Jenkins P.J., Ahktar M.A., Foster C.J. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2013;95:1576–1584. doi: 10.2106/JBJS.L.00307. [DOI] [PubMed] [Google Scholar]
- 69.Rokito A.S., Zuckerman J.D., Shaari J.M., Eisenberg D.P., Cuomo F., Gallagher M.A. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Joint Dis. 2003;61:32–39. [PubMed] [Google Scholar]
- 70.Rowe C.R. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29–42. [PubMed] [Google Scholar]
- 71.Saha P., Datta P., Ayan S., Garg A.K., Bandyopadhyay U., Kundu S. Plate versus titanium elastic nail in treatment of displaced midshaft clavicle fractures: a comparative study. Indian J Orthop. 2014;48:587–593. doi: 10.4103/0019-5413.144227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Salipas A., Kimmel L.A., Edwards E.R., Rakhra S., Moaveni A.K. Natural history of medial clavicle fractures. Injury. 2016;47:2235–2239. doi: 10.1016/j.injury.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 73.Schemitsch L.A., Schemitsch E.H., Veillette C., Zdero R., McKee M.D. Function plateaus by one year in patients with surgically treated displaced midshaft clavicle fractures. Clin Orthop Relat Res. 2011;469:3351–3355. doi: 10.1007/s11999-011-1915-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Seyhan M., Kocaoglu B., Kiyak G., Gereli A., Turkmen M. Anatomic locking plate and coracoclavicular stabilization with suture Endo-button technique is superior in the treatment of Neer type II distal clavicle fractures. Eur J Orthop Surg Traumatol. 2015;25:827–832. doi: 10.1007/s00590-015-1617-2. [DOI] [PubMed] [Google Scholar]
- 75.Shetty S.K., Chandran R., Ballal A., Mathias L.J., Hegde A., Shetty A. To operate or not to operate the mid-shaft fractures of the clavicle: a comparative study of functional outcomes of the two methods of management. J Clin Diagn Res. 2017;11:RC01–RC03. doi: 10.7860/JCDR/2017/22052.9143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Siebenlist S., Sandmann G., Kirchhoff C., Biberthaler P., Neumaier M. Anatomically precontoured LCP for delayed union of a medial third clavicle fracture. Case report with review of the literature. Acta Chir Orthop Traumatol Cech. 2013;80:407–410. [PubMed] [Google Scholar]
- 77.Silva F.B., Kojima K.E., Silva J.S., Mattar Junior R. Comparison between plate and flexible intramedullary fixation in the treatment of midshaft clavicle fractures—preliminary results. Rev Bras Ortop. 2011;46:34–39. doi: 10.1590/S0102-36162011000700009. [DOI] [Google Scholar]
- 78.Singh R., Rambani R., Kanakaris N., Giannoudis P.V. A 2-year experience, management and outcome of 200 clavicle fractures. Injury. 2012;43:159–163. doi: 10.1016/j.injury.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 79.Smekal V., Irenberger A., Attal R.E., Oberladstaetter J., Krappinger D., Kralinger F. Elastic stable intramedullary nailing is best for mid-shaft clavicular fractures without comminution: results in 60 patients. Injury. 2011;42:324–329. doi: 10.1016/j.injury.2010.02.033. [DOI] [PubMed] [Google Scholar]
- 80.Smekal V., Irenberger A., Struve P., Wambacher M., Krappinger D., Kralinger F.S. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures—a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23:106–112. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 81.Smelt J., Khakha R.S., Harrison-Phipps K., Richards A., Bille A. An isolated traumatic medial third clavicular fracture requiring surgical fixation. Ann Thor Surg. 2017;103:e297–e298. doi: 10.1016/j.athoracsur.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 82.Souza Vilela J.C., de Andrade R.P., Jacques Goncalves L.B., Abreu Machado T.L., Correa Filho M.R., de Araujo I.D. Fractures of the distal clavicle: comparison between two surgical treatment methods. Rev Bras Ortop. 2015;50:136–141. doi: 10.1016/j.rboe.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tabatabaei S., Shalamzari S. Treatment of displaced midshaft clavicular fractures: a comparison between smooth pin and LCDCP and reconstruction plate fixation. Pak J Med Sci. 2011;27:1129–1134. [Google Scholar]
- 84.Tamaoki M.J.S., Matsunaga F.T., Costa A., Netto N.A., Matsumoto M.H., Belloti J.C. Treatment of displaced midshaft clavicle fractures: figure-of-eight harness versus anterior plate osteosynthesis: a randomized controlled trial. J Bone Joint Surg Am. 2017;99:1159–1165. doi: 10.2106/JBJS.16.01184. [DOI] [PubMed] [Google Scholar]
- 85.Tan H.L., Zhao J.K., Qian C., Shi Y., Zhou Q. Clinical results of treatment using a clavicular hook plate versus a T-plate in Neer type II distal clavicle fractures. Orthopedics. 2012;35:e1191–e1197. doi: 10.3928/01477447-20120725-18. [DOI] [PubMed] [Google Scholar]
- 86.Tang H., Yin Y., Han Q., Xu X., Li Y. Effectiveness of anatomical locking plate internal fixation combined with coracoclavicular ligament reconstruction for Neer type IIb distal clavicle fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32:1181–1186. doi: 10.7507/1002-1892.201803127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tarng Y.W., Yang S.W., Fang Y.P., Hsu C.J. Surgical management of uncomplicated midshaft clavicle fractures: a comparison between titanium elastic nails and small reconstruction plates. J Shoulder Elbow Surg. 2012;21:732–740. doi: 10.1016/j.jse.2011.08.065. [DOI] [PubMed] [Google Scholar]
- 88.Teng H.G., Liu A.L. Partial claviculectomy after non-union of proximal clavicle fracture. BMJ Case Rep. 2013;29:29. doi: 10.1136/bcr-2013-008874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Titchener A., See A., Van Rensburg L., Tytherleigh-Strong G. Displaced medial end clavicular fractures treated with an inverted distal clavicle plate contoured through 90 degrees. J Shoulder Elbow Surg. 2019;28:e97–e103. doi: 10.1016/j.jse.2018.08.047. [DOI] [PubMed] [Google Scholar]
- 90.Tsuei Y.C., Au M.K., Chu W. Comparison of clinical results of surgical treatment for unstable distal clavicle fractures by transacromial pins with and without tension band wire. J Chin Med Assoc. 2010;73:638–643. doi: 10.1016/s1726-4901(10)70139-8. [DOI] [PubMed] [Google Scholar]
- 91.Tutuhatunewa E.D., Stevens M., Diercks R.L. Clinical outcomes and predictors of patient satisfaction in displaced midshaft clavicle fractures in adults: results from a retrospective multicentre study. Injury. 2017;48:2788–2792. doi: 10.1016/j.injury.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 92.van der Meijden O.A., Gaskill T.R., Millett P.J. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2012;21:423–429. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 93.van der Meijden O.A., Houwert R.M., Hulsmans M., Wijdicks F.J., Dijkgraaf M.G., Meylaerts S.A. Operative treatment of dislocated midshaft clavicular fractures: plate or intramedullary nail fixation? A randomized controlled trial. J Bone Joint Surg Am. 2015;97:613–619. doi: 10.2106/JBJS.N.00449. [DOI] [PubMed] [Google Scholar]
- 94.Van Der Ven Denise J.C., Timmers T.K., Flikweert P.E., Van Ijseldijk A.L.A., Van Olden G.D.J. Plate fixation versus conservative treatment of displaced midshaft clavicle fractures: functional outcome and patients' satisfaction during a mean follow-up of 5 years. Injury. 2015;46:2223–2229. doi: 10.1016/j.injury.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 95.Van Tongel A., Toussaint A., Herregods S., Van Damme S., Marrannes J., De Wilde L. Anatomically based classification of medial clavicle fractures. Acta Orthop Belg. 2018;84:62–67. [PubMed] [Google Scholar]
- 96.Virtanen K.J., Malmivaara A.O.V., Remes V.M., Paavola M.P. Operative and nonoperative treatment of clavicle fractures in adults. Acta Orthop. 2012;83:65–73. doi: 10.3109/17453674.2011.652884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Virtanen K.J., Remes V., Pajarinen J., Savolainen V., Björkenheim J.M., Paavola M. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. J Bone Joint Surg Am. 2012;94:1546–1553. doi: 10.2106/JBJS.J.01999. [DOI] [PubMed] [Google Scholar]
- 98.Wang J., Meng X.H., Guo Z.M., Wu Y.H., Zhao J.G. Interventions for treating displaced midshaft clavicular fractures: a Bayesian network meta-analysis of randomized controlled trials. Medicine (Baltimore) 2015;94:e595. doi: 10.1097/md.0000000000000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wang Y., Jiang J., Dou B., Zhang P. Inverted distal clavicle anatomic locking plate for displaced medial clavicle fracture. Arch Orthop Trauma Surg. 2015;135:1241–1245. doi: 10.1007/s00402-015-2259-x. [DOI] [PubMed] [Google Scholar]
- 100.Wang Y.C., Fu Y.C., Chou S.H., Liu P.C., Tien Y.C., Lu C.C. Titanium Elastic Nail versus plate fixation of displaced midshaft clavicle fractures: a retrospective comparison study. Kaohsiung J Med Sci. 2015;31:473–479. doi: 10.1016/j.kjms.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 101.Wenninger J.J., Jr., Dannenbaum J.H., Branstetter J.G., Arrington E.D. Comparison of complication rates of intramedullary pin fixation versus plating of midshaft clavicle fractures in an active duty military population. J Surg Orthop Adv. 2013;22:77–81. doi: 10.3113/JSOA.2013.0077. [DOI] [PubMed] [Google Scholar]
- 102.Wijdicks F.J., Houwert M., Dijkgraaf M., De Lange D., Oosterhuis K., Clevers G. Complications after plate fixation and elastic stable intramedullary nailing of dislocated midshaft clavicle fractures: a retrospective comparison. Int Orthop. 2012;36:2139–2145. doi: 10.1007/s00264-012-1615-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Woltz S., Stegeman S.A., Krijnen P., van Dijkman B.A., van Thiel T.P., Schep N.W. Plate fixation compared with nonoperative treatment for displaced midshaft clavicular fractures: a multicenter randomized controlled trial. J Bone Joint Surg Am. 2017;99:106–112. doi: 10.2106/JBJS.15.01394. [DOI] [PubMed] [Google Scholar]
- 104.Wu K., Chang C.H., Yang R.S. Comparing hook plates and Kirschner tension band wiring for unstable lateral clavicle fractures. Orthopedics. 2011;34:e718–e723. doi: 10.3928/01477447-20110922-17. [DOI] [PubMed] [Google Scholar]
- 105.Xie W.P., Zhang Y.K., Chen Y.H., Wang S.L., Xu H.H., Bi R.X. A novel surgical method for treating medial-end clavicle fractures. Exp Ther Med. 2018;16:5390–5393. doi: 10.3892/etm.2018.6870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Xiong J., Chen J.H., Dang Y., Zhang D.Y., Fu Z.G., Zhang P.X. Treatment of unstable distal clavicle fractures (Neer type II): a comparison of three internal fixation methods. J Int Med Res. 2018;46:4678–4683. doi: 10.1177/030006051878824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yan H.W., Li L., Wang R.C., Yang Y., Xie Y., Tang J. Clinical efficacies of coracoclavicular ligament reconstruction using suture anchor versus hook plate in the treatment of distal clavicle fracture. Orthop Traumatol Surg Res. 2017;103:1287–1293. doi: 10.1016/j.otsr.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 108.Zehir S., Zehir R., Şahin E., Çalbıyık M. Comparison of novel intramedullary nailing with mini-invasive plating in surgical fixation of displaced midshaft clavicle fractures. Arch Orthop Trauma Surg. 2015;135:339–344. doi: 10.1007/s00402-014-2142-1. [DOI] [PubMed] [Google Scholar]
- 109.Zheng Y., Yuan X.H., Yin Y.H., Wang W.B., Fu Q.S., Pang Q.J. T-plate fixation for unstable proximal clavicula fractures. Acta Orthop Traumatol Turc. 2018;52:464–468. doi: 10.1016/j.aott.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zlowodzki M., Zelle B.A., Cole P.A., Jeray K., McKee M.D. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504–507. doi: 10.1097/01.bot.0000172287.44278.ef. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.