Abstract
Background.
The use of electronic cigarettes (e-cigarette) offers potential to facilitate cigarette smoking cessation, yet potentially increases risk of cigarette smoking initiation. This relationship has been primarily modeled in mathematical ways that often do not represent real-world complexities, which could inform decisions regarding local prevention programs or policies.
Aims.
To develop a model of cigarette and e-cigarette use that combines current research on tobacco use and incorporates real-world geographic and demographic data.
Method.
We used a platform for developing agent-based models with demographic information representative of the population in Pennsylvania. We developed three models of cigarette and e-cigarette use. The primary outcome for each was the total number of users for cigarette, e-cigarette, and total nicotine. The first model applied current cigarette and e-cigarette data, the second tested the effect of implementing a program of e-cigarette education and policies, and the third considered a social contagion factor, where local schools functioned as a transmission vector.
Results.
The baseline and social contagion models found an overall decline in cigarette use but an increase in e-cigarette and total nicotine use. The education/policies model had declines in all categories. Sensitivity analysis suggested the importance of nuanced e-cigarette/cigarette interactions when modeling tobacco use.
Discussion.
Public health campaigns that focus on reducing youth e-cigarette usage can have a large effect. Social contagion should be strongly considered when studying e-cigarette spread.
Conclusion.
Targeted public health campaigns focused on reducing school prevalence of e-cigarette use may be particularly valuable.
Keywords: agent-based model, cigarette, e-cigarette, nicotine, population model, social contagion
The U.S. Food and Drug Administration (FDA) recently announced results from the 2018 National Youth Tobacco Survey, highlighting a 78% increase in electronic cigarette (e-cigarette) use among high school students from the previous year (FDA, 2018a). This increase, along with a small uptick in cigarette use (7.6% to 8.1%), reversed years of decline in overall youth tobacco product use and prompted the U.S. Surgeon General to declare e-cigarette use among youth a national epidemic (Stein, 2018). Among young adults, ever e-cigarette use increased from 2014 to 2016 (Bao, Xu, Lu, Snetselaar, & Wallace, 2018). Analyses of data from the 2016 Behavioral Risk Factor Surveillance System found a prevalence of 1.4% for sole e-cigarette use (i.e., never used cigarettes), which translated to 1.9 million sole e-cigarette users, 17.7% of whom reported daily e-cigarette use (Mirbolouk et al., 2019).
The use of e-cigarettes is a controversial public health topic. On one hand, recent studies suggest that e-cigarettes may facilitate cigarette cessation among adult smokers (Berry et al., 2018; Hajek et al., 2019). The efficacy of e-cigarettes as a cessation aid may be due to higher levels of satisfaction and self-reported helpfulness as compared with nicotine replacement products currently approved by the FDA (Hajek et al., 2019). This appears to be more pronounced for daily e-cigarette users as compared with less frequent users. For example, analysis of the first two waves (2013–2015) of the Population Assessment of Tobacco and Health Study found that daily e-cigarette use is associated with a 7.88 greater odds of 30-day cigarette cessation, while individuals who experimented with e-cigarettes had a decreased odds (adjusted odds ratio = 0.51, 95% confidence interval = [0.07, 1.47]) of 30-day cigarette cessation (Berry et al., 2018).
However, other research suggests that e-cigarettes may actually increase the risk of traditional cigarette initiation among otherwise never-smoking youth and young adults (Barrington-Trimis et al., 2016; Primack et al., 2018; Primack, Soneji, Stoolmiller, Fine, & Sargent, 2015; Soneji et al., 2017; Spindle et al., 2017). For example, a large nationally representative study found that for youth considered at low risk for smoking initiation, e-cigarette use was associated with 8.57 greater odds of cigarette initiation (Berry et al., 2019).
Given the possibility for e-cigarettes to facilitate both cigarette smoking initiation and cessation, the question remains as to the potential impact of e-cigarettes at a population level. Quantifying the balance of population benefits and harms is challenging, as it requires accounting for both the number of current adult cigarette smokers who will successfully quit traditional cigarettes using e-cigarettes as well as the number of never-smoking youth and older individuals who will initiate cigarette smoking through the use of e-cigarettes. Since e-cigarette use is a relatively new phenomenon, there is a lack of robust, longitudinal empirical data to answer this question. One possible solution is to use computational models that can provide insight by projecting possible outcomes under varying scenarios. Such models are particularly useful for population health problems such as tobacco use, where dynamic interrelations exist between individual and environmental influences (Diez Roux, 2011). Moreover, the Institute of Medicine recently published a report highlighting the potential of agent-based models as an essential tool to inform decision making around tobacco related educational programming and policies (Institute of Medicine, 2015a).
Previous models examining population-level benefits and harms of e-cigarette use have yielded mixed results. A Monte Carlo stochastic simulation model suggested more population-level harm than benefit from e-cigarette use. This model estimated that an additional 2,070 cigarette smoking adults would quit smoking through the use of e-cigarettes in 2015, but 168,000 never-cigarette smoking adolescents and young adults who had ever used e-cigarettes would initiate smoking in 2015 and eventually become daily cigarette smokers. The model also estimated that the net increase in daily cigarette smokers would lead to 1,510,000 years of life lost due to e-cigarette use in 2014 (Soneji, Sung, Primack, Pierce, & Sargent, 2018). Other studies using a decision-theoretic model, systems dynamics approach, or agent-based model suggested more population-level benefit than harm, as defined by a decrease in the number of smokers or a decrease in smoking-attributable deaths (Cherng, Tam, Christine, & Meza, 2016; Hill & Camacho, 2017; Levy, Borland, et al., 2017). Specifically, Levy, Cummings, et al. (2017) used a decision-theoretic model with a cohort of individuals born in 1997 to calculate a 21% decrease in smoking-attributable deaths by the year 2083 due to the introduction of e-cigarettes. Monte Carlo simulations of seven different use scenarios found population-level benefits only when most e-cigarette users are either current smokers interested in cessation or when youth would have become smokers even in the absence of e-cigarettes (Kalkhoran & Glantz, 2015).
These mixed results may in part be explained by the input parameters used in previous studies. Models that projected an overall decrease in the number of cigarette smokers assumed a low odds of youth e-cigarette users transitioning to cigarette smoking and used older data to approximate the prevalence of youth cigarette and e-cigarette use. For example, using data from the 1965–2012 National Health Interview Surveys, the Levy, Borland, et al. (2017) model predicted that 12.6% of males and 8.5% of females in the 1997 birth cohort would smoke cigarettes at age 18 years. However, the 2015 National Health Interview Survey (the year these individuals would be 18) found that 6.6% of 18-year-old males and 3.6% of 18-year-old females were current cigarette smokers. This short-term prediction error has led other researchers to express concern about the accuracy of this model (Soneji, Sung, Primack, Pierce, & Sargent, 2018). Thus, there is a need for updated modeling using more recent data.
In addition, prior efforts were primarily mathematical models that did not necessarily represent real-world complexities, for example, number of vape shops in a neighborhood. These models provide a comprehensive view of high-level outcomes but do not account for the nuanced nature of e-cigarette use, which can vary significantly based on location and demographics. E-cigarette models that apply nationally or internationally representative data can find results that show mean effects without accounting for trends in demographics (e.g., cities with high densities of subpopulations vulnerable to smoking). Most modeling efforts also do not present e-cigarette trends in the context of overall effects on cigarette or total nicotine use. Examining the effect of e-cigarettes on total nicotine use may be particularly valuable in light of previous research suggesting that exposure to nicotine through e-cigarettes or nicotine replacement therapy may affect adolescent brain development and elevate the risk for cardiovascular disease in adults (Mills, Thorlund, Eapen, Wu, & Prochaska, 2014; Yuan, Cross, Loughlin, & Leslie, 2015). Most important, individual behaviors affected by other people in shared proximities, school locations, and actions of other people are rarely modeled at all. Given that youth who report ever use of e-cigarettes identified “use by friend or family member” as the top reason for their own use (Tsai et al., 2018), it may be particularly valuable to include information regarding social contagion in e-cigarette susceptibility.
Thus, there is a need to conduct research that can provide information regarding potential population-level harm in a localized geographic area, which can allow for proper resource allocation and targeted primary prevention efforts. This may prove more useful than estimating state or local scenarios based on data from national or international sources, which may not consider nuanced complexities in a narrower scope. The primary objective of this study is to address that need by developing a model of cigarette and e-cigarette use that combines current research on tobacco use and incorporates real-world geographic and demographic data.
Method
Modeling Framework
To develop our model, we used the Framework for Reconstructing Epidemiological Dynamics (FRED; Grefenstette et al., 2013). FRED is a tool for creating agent-based models, and not a model in and of itself. Agent-based modeling is a simulation modeling technique that uses a collection of individual “agents” who follow simple rules (Bonabeau, 2002; Epstein & Axtell, 1996). As the simulation unfolds, agents interact with one another, with the consequence of each interaction governed by each agent’s behavioral rules and previous actions. Often, agents represent humans, and their behavioral rules may be based on the characteristics associated with each agent, such as age, gender, and location. The actions and interactions of individual agents result in population-level phenomena. Agent-based models use a population of agents with individualized behavior and activities to model complex and emergent behavior on a population level. Agent-based models can incorporate a range of geographical and spatiotemporal heterogeneities that may be impractical or intractable for purely mathematical models (Bonabeau, 2002).
In FRED, agents represent humans. FRED uses a census derived synthetic population (based on the 2010 U.S. Census) to allocate household, workplace, and school locations to every member of any U.S. geographic area (Wheaton, 2014). FRED agents are encoded with demographic information representative of the real population in the geographic area, including age, gender, race, income, and employment and school locations (Grefenstette et al., 2013). This demographic data, along with the behavior and actions of other agents, can be used to influence the behavior of each agent.
FRED has previously been used to investigate a range of public health topics, including the benefits of paid sick leave and vaccination policies, positioning of health care facilities after natural disasters, and asthma and heat stroke risks during severe pollution events (Grefenstette & Schaper, 2017; Guclu et al., 2016; Liu et al., 2015). This study leverages FRED to investigate cigarette and e-cigarette use over time. FRED’s unique ability to represent the U.S. population at a fine grained level can reveal trends unavailable to other models. For example, FRED contains real school locations, with enrollment linked to demographic information (e.g., richer households are more likely to have their children at private schools, while public school students attend a school near their home). These factors provide the ability to incorporate strong social and spatial determinants of cigarette and e-cigarette use into our model. By utilizing these capabilities, we will be able to better understand population-level behavior and provide results that can affect policy and programs.
Model Conditions and States
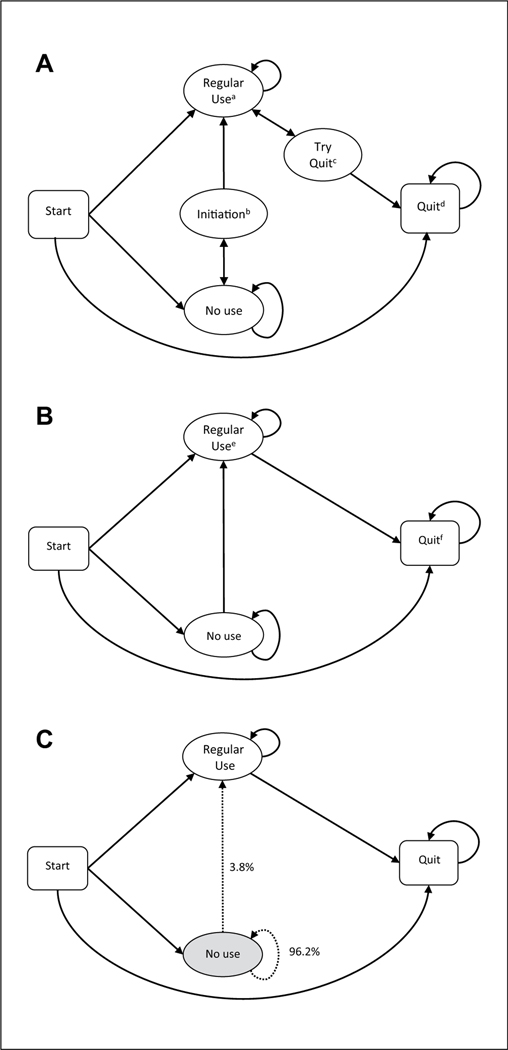
Our model consisted of two conditions—cigarette and e-cigarette use—through which agents move simultaneously and autonomously (Figure 1). For both conditions, agents enter the model in one of three states: regular use, no use, or quit based on prevalence data. Due to the availability of data, the cigarette condition included two additional states: (1) initiate use and (2) try quit. An agent may move between different states in both the cigarette and e-cigarette models based on data from existing research (Table 1); that is, we apply probabilistic data of tobacco use from existing research to determine the likelihood that an agent transitions between tobacco use states. For example, an agent who represents a 14-year-old youth who does not use cigarettes or e-cigarettes has a 3.8% chance of initiating e-cigarette use, moving from e-cigarette no use to e-cigarette regular use (Figure 1). The frequency of transitions, that is, how often an agent applies the probabilities to change their behavior, occurs annually, with the exact date randomly chosen from the 365-day period.
Figure 1.
FRED (Framework for Reconstructing Epidemiological Dynamics) state-transition diagrams. (A) Cigarette states and potential transitions. (B) E-cigarette states and potential transitions. (C) An example of a state transition: A 14-year-old e-cigarette nonuser has a 3.8% chance of becoming an e-cigarette regular user and a 96.2% chance of remaining a nonuser. Note. State definitions include apast 30-day use; bpast year first-time use; cat least one quit attempt past year; dnot smoked for 6+ months; epast 30-day use; fnot current user.
Table 1.
Definitions and Sources for All State Transitions in Cigarette and E-Cigarette Models.
| Transition | Source | Citation |
|---|---|---|
| Cigarette | ||
| Start → regular use Start → no use Start → quit |
(<18) CDC YRBS data; PA prevalence (18+) CDC BRFSS data; PA prevalence |
Centers for Disease Control and Prevention. (2018). Morbidity and Mortality Weekly Report Surveillance Summaries, 67(8). Retrieved from https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/ss6708.pdf Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. (2015). BRFSS prevalence & trends data. Retrieved from https://www.cdc.gov/brfss/brfssprevalence/ |
| No use ↔ initiation (e-cigarette nonuser) | 2017 National Survey on Drug Use and Health | https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf |
| No use ↔ regular use (e-cigarette user) | Systematic review | Soneji, S. S., Barrington-Trimis, J. L., Wills, T. A., Leventhal, A. M., Unger, J. B., Gibson, L. A., . . . Sargent, J. D. (2017). Association between |
| Initiation → regular use | initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults. JAMA Pediatrics, 171, 788–797. doi:10.1001/jamapediatrics.2017.14882017 | |
| Regular use → try quit | National Health Interview Surveys (2001–2010) | Centers for Disease Control and Prevention. (2011, November 11). Quitting smoking among adults—United States, 2001–2010. MMWR Morbidity and Mortality Weekly Report, 60(44). Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6044a2.htm |
| Try quit → QuitWithVape | Nationally representative survey (2014–2016) | Caraballo, R. S., Shafer, P. R., Patel, D., Davis, K. C., & McAfee, T. A. (2017). Quit methods used by U.S. adult cigarette smokers, 2014–2016. Preventing |
| Try quit → | Chronic Disease, 14, E32. doi:10.5888/pcd14.160600 | |
| QuitWithoutVape QuitWithVape → Quit |
Systematic review | Rahman, M. A., Hann, N., Wilson, A., Mnatzaganian, G., Worrall-Carter, L. (2015). E-cigarettes and smoking cessation: Evidence from a systematic review and meta-analysis. PloS One, 10, e0122544. |
| QuitWithoutVape → quit | CDC 2001–2010 National Health Interview Surveys | https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6044a2.htm |
| E-cigarette | ||
| Start → regular use Start → no use Start → quit |
(<18) CDC YRBS data; PA prevalence (18+) CDC BRFSS data; PA prevalence |
Centers for Disease Control and Prevention. (2018). Surveillance summaries. Morbidity and Mortality Weekly Report, 67(8). Retrieved from https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/ss6708.pdf Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. (2015). BRFSS prevalence & trends data. Retrieved from https://www.cdc.gov/brfss/brfssprevalence/ |
| No use ↔ regular use | (<18) PATH (18+) nationally representative longitudinal online survey of U.S. adults aged ≥18 years |
(<18) Stanton, C. A., Bansal-Travers, M., Johnson, A. L., Sharma, E., Katz, L., Ambrose, B. K., . . . Pearson, J. L. (2019). Longitudinal e-cigarette and cigarette use among US youth in the PATH Study (2013–2015). JNCI Journal of the National Cancer Institute, djz006. doi:10.1093/jnci/djz006 (18+) Agaku, I. T., Davis, K., Patel, D., Shafer, P., Cox, S., Ridgeway, W., & King, B. A. (2017). A longitudinal study of the relationship between receptivity to e-cigarette advertisements and e-cigarette use among baseline non-users of cigarettes and e-cigarettes, United States. Tobacco Induced Diseases, 15, Article 42. doi:10.1186/s12971-017-0145-8 |
| Regular use → quit | PATH | Coleman, B., Rostron, B., Johnson, S. E., Persoskie, A., Pearson, J., Stanton, C., . . . Hyland, A. (2019). Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, Waves 1 and 2 (2013–2015). Tobacco Control, 28, 50–59. |
Note. YRBS = Youth Risk Behavior Surveillance System; BRFSS = Behavioral Risk Factor Surveillance System; PATH = Population Assessment of Tobacco and Health; PA = Pennsylvania; CDC = Centers for Disease Control and Prevention.
Data
This study was conducted using data for the state of Pennsylvania (PA). Historically, PA has represented a politically and demographically diverse microcosm of the United States, with its counties exemplifying recent demographic shifts in urban, suburban, and rural communities (Frey & Teixeira, 2008; Parker et al., 2018). PA also has established tobacco control advocacy groups as well as tobacco manufacturers/processors (Colditz, Ton, James, & Primack, 2017). Moreover, PA currently does not spend any money on advertising campaigns and public service announcements to alert parents, teachers, and youth about the dangers of e-cigarette use (Scheck, 2018). In fiscal year 2019, PA received approximately $1.7 billion in tobacco revenue yet spent only $15.5 million on tobacco prevention, far below the Centers for Disease Control and Prevention recommendation of $140 million (Campaign for Tobacco Free Kids, 2018). This is in contrast to the approximately $380 million spent on marketing by tobacco companies in PA (Campaign for Tobacco Free Kids, 2018).
Simulation Models
We developed three simulation models of cigarette and e-cigarette use in FRED to help evaluate how factors in e-cigarette education and social contagion might affect tobacco use. In each model, the primary outcome was the total number of users for cigarette, e-cigarette, and total nicotine (the sum of cigarette and e-cigarette users). The first model (“baseline model”) applied current cigarette and e-cigarette data to establish baseline outcomes. The second model (“education/policy enhanced model”) tested the effect of successfully implementing a program of e-cigarette education and policies. For example, assuming that the success of the programs matches what tobacco control has been able to achieve with youth cigarette programs and policies, we modified youth e-cigarette uptake to match the lower youth cigarette uptake. The third model (“social contagion model”) considered a social contagion factor, where risk of e-cigarette uptake was affected by local school prevalence. No literature currently exists to guide how to model this effect. We assumed that if greater than 10% of the agents enrolled at each school were currently e-cigarette users, this would represent a normalization of e-cigarette use in that school, with the effect of encouraging initiation among nonusers (owing to factors such as peer pressure and easier access to e-cigarettes). We therefore doubled each agent’s odds of e-cigarette initiation if they attended a school where greater than 10% of the students used e-cigarettes, relative to the baseline scenario. Similarly, if fewer than 10% of the agents at a school were e-cigarette users, we assumed that this would halve the odds of e-cigarette initiation, relative to the baseline scenario, as factors such as peer pressure, cultural normalization and access to e-cigarettes. Models were run for a simulated 20-year period to allow adequate time for new agents to enter the simulation (i.e., births) and progress through adolescence, but not so long as to overextend projections across multigenerational lifespans. The simulations were run using the FRED synthetic population for the state of Pennsylvania.
Model Assumptions
There are several assumptions and simplifications made when constructing the models. First, total nicotine users will be inflated, as we are overcounting agents who use cigarettes and e-cigarettes (dual users) and also assume that e-cigarettes will always contain nicotine. Literature on activities of dual users are limited and do not provide enough data for us to accurately model their specific behaviors; therefore, we explicitly delineated these activities for conceptual reasons. Next, we assume that quitting is a terminal state, where there is no relapse. Our models consider a successful quit attempt as having no use for a year, widely considered as having a low chance of relapse. Last, cigarette cessation attempts are a complex topic, both in how often attempts are made as well as the methods used (Caraballo, Shafer, Patel, Davis, & McAfee, 2017). With regard to using e-cigarettes as a cessation aid, we choose a moderate characterization by defining an e-cigarette aided cessation attempt as an agent switching entirely from cigarettes to e-cigarettes, but potentially using other cessation support (e.g., nicotine gum) as well.
Sensitivity Analyses
To assess the robustness of our results and address potential bias, we conducted a sensitivity analysis on the use of e-cigarettes as a cigarette cessation aid. Quitting traditional cigarettes can vary not only by which aids are used but also by the combination of methods (Caraballo et al., 2017). Therefore, in addition to the baseline measure (switching completely to e-cigarettes, alone, or in combination with other methods), we also modeled results ranging from the strictest (switching completely to e-cigarettes as the only method) to the most lenient (partially switching to e-cigarettes, alone, or in combination with other methods) definitions.
Results
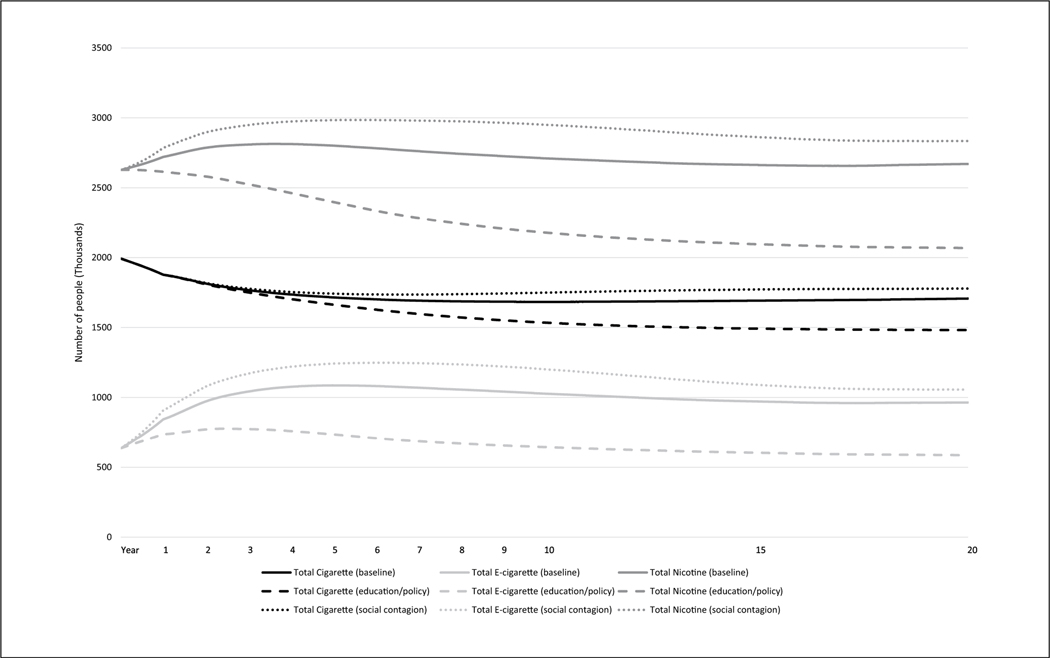
Figure 2 shows the trends of each model over 20 years; Table 2 represents the data in tabular format. The baseline model found an overall decline in cigarette use; e-cigarette use initially increases but levels off, resulting in a 51% increase from current prevalence; total nicotine follows a similar trajectory of initial increase followed by a plateau. The education/policy enhanced model had declines in all categories, both compared against today’s rates of use as well as the baseline model after 20 years. The social contagion model found an overall decline in cigarette use but an increase in e-cigarette and total nicotine use compared with today’s prevalence; however, when compared against the baseline model at 20 years, there are increases in all categories.
Figure 2.
FRED (Framework for Reconstructing Epidemiological Dynamics) tobacco model simulations over 20 years.
Table 2.
Change in Cigarette, E-Cigarette, and Nicotine Users in Each Model After 20 Years.
| Tobacco use | Current | Baseline (%) | Education/policy enhanced (%) | Social contagion (%) |
|---|---|---|---|---|
| Total cigarette | 1,992,197 (ref) | −285,549 (−14.33) | −510,098 (−25.6) | −213,555 (−10.72) |
| Total e-cigarette | 636,230 (ref) | 327,848 (+51.53) | −50,280 (−7.9) | 419,773 (+65.98) |
| Total nicotine | 2,628,427 (ref) | 42,299 (+1.61) | −560,378 (−21.32) | 206,218 (+7.85) |
| Total cigarette | 1,706,648 (ref) | −224,549 (−13.16) | 71,994 (+4.22) | |
| Total e-cigarette | 964,079 (ref) | −378,129 (−39.22) | 91,925 (+9.54) | |
| Total nicotine | 2,670,727 (ref) | −602,678 (−21.63) | 163,919 (+6.14) |
Note. Percent change is compared with current (Day 0) values in top half and compared with baseline model in bottom half. ref = reference.
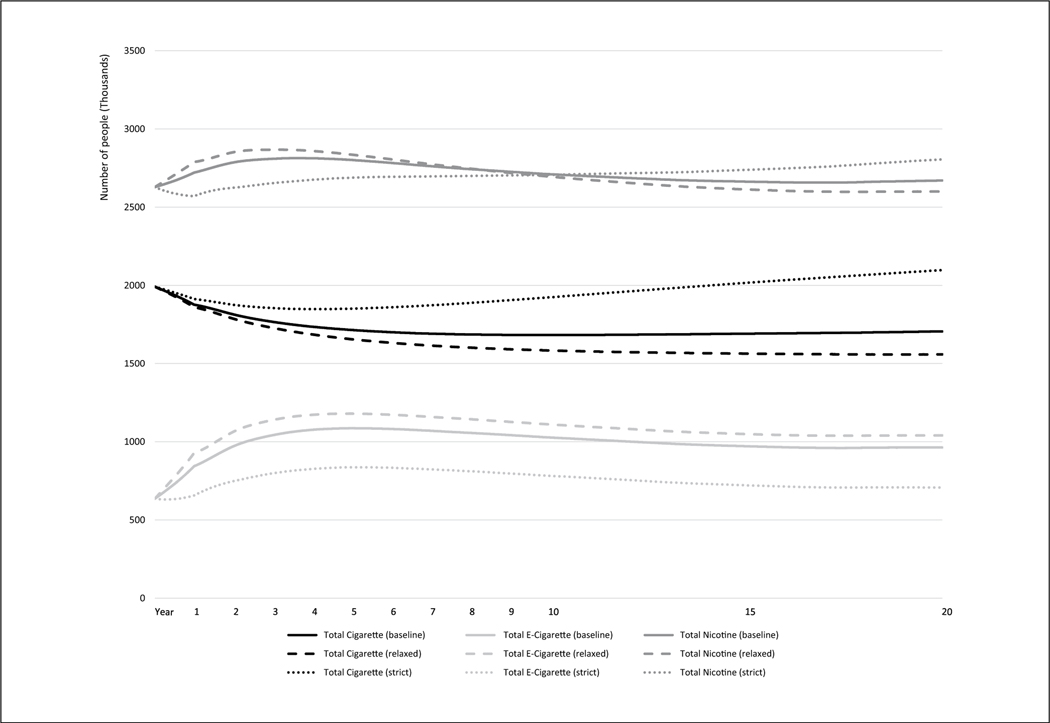
The sensitivity analysis (Figure 3) found that the lenient definition of using e-cigarettes as a cigarette cessation aid resulted in more e-cigarette use but lower cigarette and total nicotine use. The strict definition resulted in fewer e-cigarette users but higher cigarette and total nicotine users. While total cigarette and e-cigarette users were consistent in both cases, the lenient model’s total nicotine use began higher for several years before declining to less than the strict model’s total nicotine use around halfway through the timeline.
Figure 3.
FRED (Framework for Reconstructing Epidemiological Dynamics) sensitivity analysis.
Discussion
In this study, we modeled cigarette and e-cigarette trends using agent-based simulation modeling in a synthetic PA population based on census data. Projecting current prevalence over 20 years based on current research on cigarette and e-cigarette initiation and cessation, we found an increase in e-cigarette use as well as an increase in total nicotine use. It is important to note the effect by which youth e-cigarette use has negatively affected the decline in traditional cigarette use—seen in both real and modeled data (FDA, 2018a). It is likely that the baseline model is representing conservative trends, as they do not account for the sharp uptick in e-cigarette use by youths in 2018 (FDA, 2018a), as these data were unavailable at the time of our study.
The education/policy enhanced model resulted in large declines in all three tobacco categories. This change suggests that public health campaigns that focus primarily on reducing youth e-cigarette usage (e.g., prevention programs, advertisement regulations, age restrictions, etc.) can have a large effect. These targeted interventions would still allow e-cigarettes to be used as a cigarette cessation device, which can be seen by the decrease in cigarette use compared with the baseline model (Figure 2).
The social contagion model showed a net increase in all tobacco use categories when compared with baseline. These results have two important implications. First, even a conservative risk adjustment by school e-cigarette prevalence can result in notable increases in cigarette and total nicotine use. Second, the outcome demonstrates that social contagion should be strongly considered when modeling e-cigarette use. Research has consistently shown that youth smoking behavior is strongly affected by perceived use of tobacco products by their peers or other forms of normalization of behaviors (Alexander, Piazza, Mekos, & Valente, 2001; Ali & Dwyer, 2009). These factors can be difficult to represent in models that do not have the ability to include social and spatial variables. A synthetic population (such as the one used by FRED) that incorporates the location and enrollment sizes of schools, as well as the age of population members, allows school-based behaviors and policies to be modeled with increased specificity.
The findings from our baseline model of an overall decline in cigarette use with an associated increase in e-cigarette use are consistent with several previous modeling studies (Cherng et al., 2016; Hill & Camacho, 2017; Levy, Borland, et al., 2017). The results of our education/policy model are also consistent with a previous study suggesting that population-level benefits from most e-cigarette users are adult current smokers interested in cessation (Kalkhoran & Glantz, 2015).
These models suggest that targeted public health campaigns focused on reducing overall school prevalence of e-cigarette use may be particularly valuable. Approximately 80% of youth do not think that regular e-cigarette use is harmful (Miech et al., 2018), and only 37% of 15- to 24-yearolds who used the e-cigarette JUUL—which owns over 70% of the e-cigarette market—in the past 30 days knew that its cartridges always contain nicotine (Willett et al., 2019). Focus groups have also found that most adults are generally unaware of the ingredients in e-cigarettes (Coleman et al., 2016). Although 88% of high school teachers and administrators reported being somewhat or very concerned about e-cigarette use by students, 34% of schools reported no formal communication from the school to parents about e-cigarette use (Truth Initiative, 2019). In 2018, the FDA launched “The Real Cost” Youth E-Cigarette Prevention Campaign to educate youth about the risks of using e-cigarettes. The campaign targets youth through social media, digital platform ads, and prevention materials in high school bathrooms (FDA, 2018b). Massachusetts recently became the first state to launch a coordinated education campaign for parents and adults who work with youth (e.g. teachers, school administrators) about e-cigarettes (Massachusetts Tobacco Cessation and Prevention Program, 2019). The Massachusetts Department of Public Health is also working to develop materials specific to youth for use in schools (Bharel & Riley, 2018). Although data on the effectiveness of these campaigns are not yet available, it may be valuable for state and local leaders in PA to mirror these efforts. Our methodology would be particularly relevant to these efforts, given FRED’s ability to account for age-specific demographics in different states and counties.
The sensitivity analysis results were unsurprising: A lenient definition of using e-cigarettes to quit led to more e-cigarette smokers and fewer cigarette users, while a strict definition resulted in fewer e-cigarette users and more cigarette smokers. The total nicotine use displayed an interesting trend where the lenient definition began with higher levels of total nicotine use than the strict definition, but the trend lines would cross after approximately 10 years. This is likely a combination of two factors: (1) more smokers continuing to try and quit—this will have a short-term inflation of e-cigarette use for the first few years of the simulation and (2) the sizable difference in successful quit rates that were applied—as more people continue transitioning to e-cigarettes, total cigarette use will have continuous declines over time. The sensitivity analysis suggests that when developing models of tobacco use, the nuanced interactions between e-cigarettes and cigarettes should always be considered.
The results of this study also have important implications for policy measures. In 2015, the IOM published substantial evidence for raising the purchasing age of tobacco products from 18 to 21 years. The report estimated that raising the purchasing age to 21 years nationwide would reduce smoking initiation among 15- to 17-year-olds and 18- to 20-yearolds by 25% and 15%, respectively (Institute of Medicine, 2015b). Current reports suggest that in Needham, Massachusetts, the tobacco 21 initiative resulted in a substantial decrease in smoking among high school youth compared with those in surrounding communities–high school smoking rates fell 6% from 2006 to 2010, compared with only a 3% drop in surrounding communities (Schneider, Buka, Dash, Winickoff, & O’Donnell, 2016). Although FDA regulations now prohibit the sale of e-cigarettes to those younger than 18 years nationwide, PA remains one of the few states to not have a specific law banning their sale to minors (U.S. Centers for Disease Control and Prevention, 2018). Given FRED’s ability to leverage local demographic data, one future direction is to analyze how policies might affect states with different demographics. More data from states that have implemented tobacco 21 could be used to simulate effects in states with large youth populations but lower age restrictions. Results from other local initiatives (e.g., vape shop limits, outdoor tobacco use) could also be modeled in cities or counties that do not have such policies.
This study also provides an opportunity to utilize FRED or other innovative modeling techniques in order to further advance understanding the effects of new technologies or disruptions in health such as e-cigarettes in tobacco. For example, the FRED models can be extended beyond total nicotine use to incorporate specific health outcomes, for example, tobacco-related cancers. Given more current census data and updated tobacco trend studies, additional complexities can also be included in the social contagion model, for example, household cigarette smokers and direct health effects of e-cigarettes.
We note several limitations in our study. While FRED is capable of modeling complex health phenomena, the models are limited by reliance on comprehensive data about incidence of and transitions among specific health states in a population. In the current model, for example, we relied on data from several studies that rely on different surveys and time periods. The models may have performed differently if more comprehensive, nationally representative data were available in this context. Additionally, the richness of our models is limited by the availability of smoking data. For example, the role of e-cigarettes as a cessation device in continued regular e-cigarette use may be a valuable addition for future models as these data become available. It is also important to note that projections such as these cannot necessarily account for large-scale social or policy shifts, such as if the FDA restricts specific types or flavors of vape liquid, although this model could be used to estimate the impacts of such policy shifts. That is, the present FRED model projects a natural progression of conditions as they unfold in a social vacuum. However, future models might include additional complexity to model social processes within a framework of “contagion” or “inoculation,” which would have clear implications for testing potential health education interventions. We also note that one model assumes that e-cigarette prevention efforts will have the same impact as prior cigarette efforts. While the assumption served to provide a baseline to our model, there are no current studies that have been conducted on the long-term effects of e-cigarette prevention programs.
Acknowledgments
We acknowledge Michelle Woods for editorial assistance.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Cancer Institute (K07CA222338, PI: Chu; R01CA225773, PI: Primack). The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Alexander C, Piazza M, Mekos D, & Valente T (2001). Peers, schools, and adolescent cigarette smoking. Journal of Adolescent Health, 29, 22–30. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11429302 [DOI] [PubMed] [Google Scholar]
- Ali MM, & Dwyer DS (2009). Estimating peer effects in adolescent smoking behavior: A longitudinal analysis. Journal of Adolescent Health, 45, 402–408. doi: 10.1016/j.jadohealth.2009.02.004 [DOI] [PubMed] [Google Scholar]
- Bao W, Xu G, Lu J, Snetselaar LG, & Wallace RB (2018). Changes in electronic cigarette use among adults in the United States, 2014–2016. JAMA Journal of the American Medical Association, 319, 2039–2041. doi: 10.1001/jama.2018.4658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, . . . McConnell R (2016). E-cigarettes and future cigarette use. Pediatrics, 138, e20160379. doi: 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry KM, Fetterman JL, Benjamin EJ, Bhatnagar A, Barrington-Trimis JL, Leventhal AM, & Stokes A (2019). Association of electronic cigarette use with subsequent initiation of tobacco cigarettes in U.S. youths. JAMA Network Open, 2, e187794. doi: 10.1001/jamanetworkopen.2018.7794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry KM, Reynolds LM, Collins JM, Siegel MB, Fetterman JL, Hamburg NM, . . . Stokes A (2018). E-cigarette initiation and associated changes in smoking cessation and reduction: The Population Assessment of Tobacco and Health Study, 2013–2015. Tobacco Control, 28, 42–49. doi: 10.1136/tobaccocontrol-2017-054108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharel M, & Riley J (2018). DPH DESE letter. Retrieved from https://www.mass.gov/files/documents/2018/10/18/DPHDESE-letter.pdf
- Bonabeau E (2002). Agent-based modeling: Methods and techniques for simulating human systems. Proceedings of the National Academy of Sciences, USA, 99(Suppl. 3), 7280–7287. doi: 10.1073/pnas.082080899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campaign for Tobacco Free Kids. (2018). Broken promises to our children: A state-by-state look at the 1998 tobacco settlement 20 years later. Retrieved from https://www.tobaccofreekids.org/what-we-do/us/statereport
- Caraballo RS, Shafer PR, Patel D, Davis KC, & McAfee TA (2017). Quit methods used by U.S. adult cigarette smokers, 2014–2016. Preventing Chronic Disease, 14, E32. doi: 10.5888/pcd14.160600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherng ST, Tam J, Christine PJ, & Meza R (2016). Modeling the effects of e-cigarettes on smoking behavior. Epidemiology, 27, 819–826. doi: 10.1097/EDE.0000000000000497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colditz JB, Ton JN, James AE, & Primack BA (2017). Toward effective water pipe tobacco control policy in the United States: Synthesis of federal, state, and local policy texts. American Journal of Health Promotion, 31, 302–309. doi: 10.4278/ajhp.150218-QUAL-736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman BN, Johnson SE, Tessman GK, Tworek C, Alexander J, Dickinson DM, . . .Green KM (2016). “It’s not smoke. It’s not tar. It’s not 4000 chemicals. Case closed”: Exploring attitudes, beliefs, and perceived social norms of e-cigarette use among adult users. Drug and Alcohol Dependence, 159, 80–85. doi: 10.1016/j.drugalcdep.2015.11.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV (2011). Complex systems thinking and current impasses in health disparities research. American Journal of Public Health, 101, 1627–1634. doi: 10.2105/AJPH.2011.300149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein JM, & Axtell R (1996). Growing artificial societies: Social science from bottom up. Washington, DC: Brookings Institution Press. [Google Scholar]
- Frey WH, & Teixeira RA (2008). The political geography of Pennsylvania: Not another Rust Belt stat. Washington, DC: Brookings Institution Press. [Google Scholar]
- Grefenstette JJ, Brown ST, Rosenfeld R, DePasse J, Stone NT, Cooley PC, . . . Burke DS (2013). FRED (A Framework for Reconstructing Epidemic Dynamics): An open-source software system for modeling infectious diseases and control strategies using census-based populations. BMC Public Health, 13, 940. doi: 10.1186/1471-2458-13-940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grefenstette JJ, & Schaper JS (2017). Using FRED and optima predict to simulate a health emergency in Pittsburgh. Presented at the OnePGH: Resilient Pittsburgh Air Quality Disaster Modeling Workshop, Pittsburgh, PA. [Google Scholar]
- Guclu H, Kumar S, Galloway D, Krauland M, Sood R, Bocour A, . . . Potter M (2016). An agent-based model for addressing the impact of a disaster on access to primary care services. Disaster Medicine and Public Health Preparedness, 10, 386–393. doi: 10.1017/dmp.2016.44 [DOI] [PubMed] [Google Scholar]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, . . . McRobbie HJ (2019). A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine, 380, 629–637. doi: 10.1056/NEJMoa1808779 [DOI] [PubMed] [Google Scholar]
- Hill A, & Camacho OM (2017). A system dynamics modelling approach to assess the impact of launching a new nicotine product on population health outcomes. Regulatory Toxicology and Pharmacology, 86, 265–278. doi: 10.1016/J.YRTPH.2017.03.012 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2015a). Assessing the use of agent-based models for tobacco regulation. In Wallace R, Geller A, Ogawaallace VA, Geller A, & Ogaw VA (Eds.). Washington, DC: National Academies Press. doi: 10.17226/19018 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2015b). Public health implications of raising the minimum age of legal access to tobacco products lowering initiation rates. Washington, DC: National Academies Press. doi: 10.17226/18997 [DOI] [PubMed] [Google Scholar]
- Kalkhoran S, & Glantz SA (2015). Modeling the health effects of expanding e-cigarette sales in the United States and United Kingdom. JAMA Internal Medicine, 175, 1671. doi: 10.1001/jamainternmed.2015.4209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, Borland R, Villanti AC, Niaura R, Yuan Z, Zhang Y, . . . Abrams DB (2017). The application of a decision-theoretic model to estimate the public health impact of vaporized nicotine product initiation in the United States. Nicotine & Tobacco Research, 19, 149–159. doi: 10.1093/ntr/ntw158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, Cummings KM, Villanti AC, Niaura R, Abrams DB, Fong GT, & Borland R (2017). A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction, 112, 8–17. doi: 10.1111/add.13394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu F, Enanoria WTA, Zipprich J, Blumberg S, Harriman K, Ackley SF, . . . Porco TC (2015). The role of vaccination coverage, individual behaviors, and the public health response in the control of measles epidemics: An agentbased simulation for California. BMC Public Health, 15, 447. doi: 10.1186/s12889-015-1766-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massachusetts Tobacco Cessation and Prevention Program. (2019). Get outraged: The new look of micotine addiction. Retrieved from http://makesmokinghistory.org/dangers-of-vaping/
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the future: National survey results on drug use, 1975–2017: Vol. 1. Secondary school students. Retrieved from http://monitoringthefuture.org/pubs/monographs/mtf-vol1_2017.pdf
- Mills EJ, Thorlund K, Eapen S, Wu P, & Prochaska JJ (2014). Cardiovascular events associated with smoking cessation pharmacotherapies: A network meta-analysis. Circulation, 129, 28–41. doi: 10.1161/CIRCULATIONAHA.113.003961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirbolouk M, Charkhchi P, Orimoloye OA, Uddin SMI, Kianoush S, Jaber R, . . . Blaha MJ (2019). E-cigarette use without a history of combustible cigarette smoking among U.S. adults: Behavioral risk factor surveillance system, 2016. Annals of Internal Medicine, 170, 76–79. doi: 10.7326/M18-1826 [DOI] [PubMed] [Google Scholar]
- Parker K, Horowitz JM, Brown A, Fry R, Cohn D, & Igielnik R (2018). What unites and divides urban, suburban and rural communities. In Social & Demographic Trends Report. Retrieved from https://www.pewsocialtrends.org/2018/05/22/what-unites-and-divides-urban-suburban-andrural-communities/ [Google Scholar]
- Primack BA, Shensa A, Sidani JE, Hoffman BL, Soneji S, Sargent JD, . . . Fine MJ (2018). Initiation of traditional cigarette smoking after electronic cigarette use among tobacco naïve US young adults. American Journal of Medicine, 131, 443.e1–443.e9. doi: 10.1016/j.amjmed.2017.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Soneji S, Stoolmiller M, Fine MJ, & Sargent JD (2015). Progression to traditional cigarette smoking after electronic cigarette use among U.S. adolescents and young adults. JAMA Pediatrics, 169, 1018–1023. doi: 10.1001/jamapediatrics.2015.1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheck T (2018, September 17). Most states have done little to stop e-cigarette use among kids despite risk of nicotine addiction. APM Reports. Retrieved from https://www.apmreports.org/story/2018/09/17/most-states-have-done-nothing-to-prevent-e-cigarette-use-among-youth [Google Scholar]
- Schneider SK, Buka SL, Dash K, Winickoff JP, & O’Donnell L (2016). Community reductions in youth smoking after raising the minimum tobacco sales age to 21. Tobacco Control, 25, 355–359. doi: 10.1136/TOBACCOCONTROL-2014-052207 [DOI] [PubMed] [Google Scholar]
- Soneji SS, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, . . . Sargent JD (2017). Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults. JAMA Pediatrics, 171, 788–797. doi: 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji SS, Sung H, Primack BA, Pierce JP, & Sargent JD (2018). Quantifying population-level health benefits and harms of e-cigarette use in the United States. PLoS One, 13, e0193328. doi: 10.1371/journal.pone.0193328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindle TR, Hiler MM, Cooke ME, Eissenberg T, Kendler KS, & Dick DM (2017). Electronic cigarette use and uptake of cigarette smoking: A longitudinal examination of U.S. college students. Addictive Behaviors, 67, 66–72. doi: 10.1016/J.ADDBEH.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein R (2018). Vaping “epidemic” among youths declared by U.S. Surgeon General. Retrieved from https://www.npr.org/sections/health-shots/2018/12/18/677755266/surgeon-generalwarns-youth-vaping-is-now-an-epidemic
- Truth Initiative. (2019). How are schools responding to the youth e-cigarette epidemic? Retrieved from https://truthinitiative.org/news/how-are-schools-responding-juul-and-youth-e-cigarette-epidemic
- Tsai J, Walton K, Coleman BN, Sharapova SR, Johnson SE, Kennedy SM, & Caraballo RS (2018). Reasons for electronic cigarette use among middle and high school students: National Youth Tobacco Survey, United States, 2016. Morbidity and Mortality Weekly Report, 67, 196–200. doi: 10.15585/mmwr.mm6706a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention. (2018). CDC STATE System E-Cigarette Legislation - Tax. Retrieved from https://chronicdata.cdc.gov/Legislation/CDC-STATE-SystemE-Cigarette-Legislation-Tax/kwbr-syv2/data
- U.S. Food and Drug Administration. (2018a). Youth tobacco use: Results from the National Youth Tobacco Survey. Retrieved from https://www.fda.gov/TobaccoProducts/PublicHealthEducation/ProtectingKidsfromTobacco/ucm405173.htm
- U.S. Food and Drug Administration. (2018b, October 18). FDA launches new campaign: “The real cost” youth e-cigarette prevention campaign. Retrieved from https://www.fda.gov/TobaccoProducts/PublicHealthEducation/PublicEducationCampaigns/TheRealCostCampaign/ucm620783.htm
- Wheaton WD (2014). U.S. synthetic population database 2010: Quick start guide. Retrieved from https://www.epimodels.org/10_Midas_Docs/SynthPop/2010_synth_pop_ver1_quickstart.pdf
- Willett JG, Bennett M, Hair EC, Xiao H, Greenberg MS, Harvey E, . . . Vallone D (2019). Recognition, use and perceptions of JUUL among youth and young adults. Tobacco Control, 28, 115–116. doi: 10.1136/tobaccocontrol-2018-054273 [DOI] [PubMed] [Google Scholar]
- Yuan M, Cross SJ, Loughlin SE, & Leslie FM (2015). Nicotine and the adolescent brain. Journal of Physiology, 593, 3397–3412. doi: 10.1113/JP270492 [DOI] [PMC free article] [PubMed] [Google Scholar]