Abstract
The first case of the new coronavirus, COVID-19, was reported in China on 17 November 2019. By the end of March 2020, the rapid global spread of infection affected over 1 million people. Italy is one of the countries most impacted, with over 100,000 positive cases identified. The first detected cases were reported on 21 February 2020 in two Italian towns: Vo’ Euganeo in the Province of Padua, Veneto region, and Codogno, in the Province of Lodi, Lombardy. In the next weeks the epidemic spread quickly across the country but mainly in the north of Italy. The two regions: Veneto and Lombardy, implemented different strategies to control the viral spread. In Veneto, health personnel tested both symptomatic and asymptomatic subjects, while in Lombardy only symptomatic cases were investigated. We analyzed the evolution of the epidemic in these regions and showed that testing both symptomatic and asymptomatic cases is a more effective strategy to mitigate the epidemic impact. We strongly recommend that decision-makers:
ensure early isolation of symptomatic patients and rapid identification of their contacts;
maximize testing rapidly, especially among people with multiple daily contacts with infected populations, high exposure to the public in essential services;
rapidly increase diagnostic capacity by mobilizing trained personnel capable of performing rRT-PCR on respiratory samples;
equip the population with protective masks.
Keywords: COVID-19, Pandemic, Virus spread
Introduction
The earliest known case of the coronavirus disease 2019, now abbreviated as COVID-19 (‘CO’ stands for ‘corona,’ ‘VI’ for ‘virus,’ and ‘D’ for disease; formerly, this disease was referred to as “2019 novel coronavirus” or “2019-nCoV”), occurred on the 17 of November 2019 in Wuhan, the capital of the Hubei province in China. The appearance of this new coronavirus was made known by the Chinese authorities a few weeks later, in December 2019 [1]. Infection from the virus can be asymptomatic or develop into flu-like symptoms, including fever, cough, and shortness of breath [2, 3]. In some cases, the disease progresses to a severe acute respiratory syndrome, pneumonia, multi-organ failure, and death [4]. The virus spreads mainly via respiratory droplets from coughs and sneezes [5]. The standard method of testing the presence of infection with COVID-19 is real-time reverse transcription polymerase chain reaction (rRT-PCR) performed on respiratory samples obtained by nasopharyngeal swab or sputum samples [6, 7], with results of the test becoming available within a few hours to two days. Following its appearance in China, the COVID-19 infection rapidly spread to countries close to China, including South Korea, Singapore, and others. Due to its high infectivity, it has now spread globally, resulting in the 2019–2020 coronavirus pandemic [4].
The Italian experience
The disease appeared for the first time in Italy in the small city of Codogno (Lombardy) in a young man of 38 years, who was defined by health personnel as Patient 1. He went to the hospital emergency room of Codogno at least twice on 18 and 19 February with flu-like symptoms but staff did not recognize his infection as COVID-19. Thus, he spread the infection to many people present in the emergency room, including medical personnel, before being hospitalized because his condition became very severe. On 21 February 2020, the authorities of Lombardy declared a lockdown for the area of Codogno, Lodi, and Casalpusterlengo, then named a “red zone.” At the same time, symptomatic infected people also appeared in the small village of Vò Euganeo, close to Padua in the region of Veneto. That village quickly imposed complete restriction of movement. Beginning at this time, the strategies to prevent the spread of infection in the regions of Lombardy and Veneto diverged. Lombardy tested only symptomatic people for the COVID-19 infection; in Vò Euganeo, health personnel screened and tested the entire population, whether people were symptomatic or not.
These different strategies determined the impact of infection in the two regions. In Lombardy, where medics tested only symptomatic subjects by nasopharyngeal swab or sputum sample, the number of infected persons rapidly increased and many patients developed severe respiratory disease, requiring intensive care. Then, another unfortunate and mismanaged case of infection in the hospital emergency room of Alzano Lombardo, a village of Lombardy, triggered an even greater virus spread through the city of Bergamo. On 21 March 2020—about one month after the discovery of Patient 1 in Codogno—the total number of symptomatic patients in Lombardy exceeded 17,000, more than 5000 of those recovered, and about 3500 had died. We attribute this incredibly high rate of lethality, exceeding 20%, to several factors. To some extent, high mortality could be due to the age of the population and a long average lifespan in Italy. However, the main reason is likely to be the lack of mass testing and miscalculation by health authorities of how many infected people were asymptomatic.
In the Vò Euganeo village, mass testing and isolation of the infected yet asymptomatic people resulted in the reduction of the infected people from 2.6 to 0.3% (more than ten times lower) and the rapid disappearance of the infection. A study performed by Dr. Andrea Crisanti clearly demonstrated that among Vò’s residents 43.2% were infected but asymptomatic. The study also shows, that an early isolation of symptomatic patients reduced the average duration of the disease (personal communication). The regional health authorities applied the early isolation strategy to all the cities of the Veneto region. On 21 March the number of infected people in this region had reached about 4500 and 170 had died. This lethality rate of 4% was much lower compared to Lombardy.
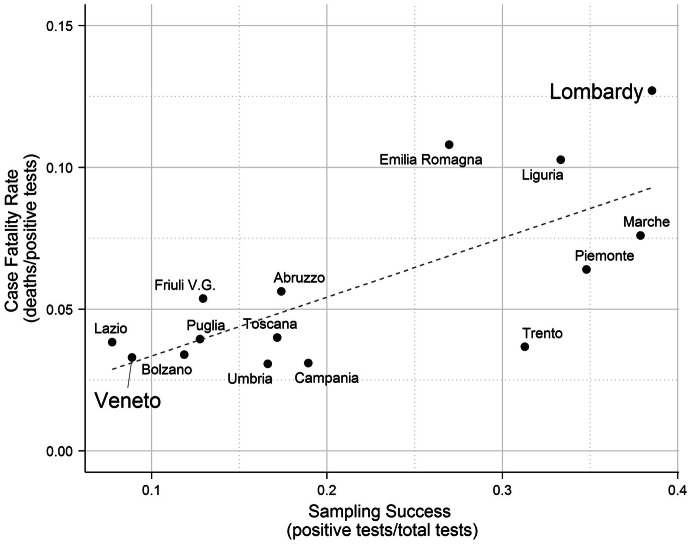
We compiled data on the number of tests performed, positive tests, deaths, testing success (a ratio of positive tests and total tested) and case fatality rate (CRF) (a ratio of deaths and positive tests) in 14 regions of Italy with more than 10 deaths due to COVID-19 as of 22 March 2020 (Table 1). We observed a strong relationship between the COVID-19 testing success, measured as a fraction of positive tests among all tested, and case fatality rate (CFR) (Spearman rank correlation coefficient ρ = 0.657; p < 0.01). Among 14 selected regions of Italy, the difference between Lombardy and Veneto regions in both sampling success and CFR is quite apparent (Fig. 1). While the population of Lombardy is twice of the Veneto (10 M vs 4.5 M), the number of tests per capita performed in Veneto was almost two times higher than in Lombardy. Similarly, the death rate due to COVID-19 in Veneto was two times lower than in Lombardy (181.3 and 344.9 cases per million population).
Table 1.
The number of tests, positive tests, deaths, testing success (a ratio of positive tests and total tested) and case fatality rate (CRF) (a ratio of deaths and positive tests) 15 regions of Italy and 21 countries with 10 or more cases of death due to COVID-19
| Locations | Date | Total tests | Positive tests | Deaths | Deaths/positive tests | Positive tests/total tests |
|---|---|---|---|---|---|---|
| 15 Italian regions (with > 10 deaths)a | ||||||
| Lombardy | 22.03.2020 | 70,598 | 27,206 | 3456 | 0.127 | 0.385 |
| Emilia Romagna | 22.03.2020 | 28,022 | 7555 | 816 | 0.108 | 0.270 |
| Veneto | 22.03.2020 | 57,671 | 5122 | 169 | 0.033 | 0.089 |
| Piemonte | 22.03.2020 | 12,701 | 4420 | 283 | 0.064 | 0.348 |
| Marche | 22.03.2020 | 6391 | 2421 | 184 | 0.076 | 0.379 |
| Toscana | 22.03.2020 | 13,264 | 2277 | 91 | 0.040 | 0.172 |
| Liguria | 22.03.2020 | 4995 | 1665 | 171 | 0.103 | 0.333 |
| Lazio | 22.03.2020 | 17,845 | 1383 | 53 | 0.038 | 0.078 |
| Campania | 22.03.2020 | 4943 | 936 | 29 | 0.031 | 0.189 |
| Friuli V.G. | 22.03.2020 | 6761 | 874 | 47 | 0.054 | 0.129 |
| Trento | 22.03.2020 | 3050 | 954 | 35 | 0.037 | 0.313 |
| Bolzano | 22.03.2020 | 5718 | 678 | 23 | 0.034 | 0.119 |
| Puglia | 22.03.2020 | 6160 | 786 | 31 | 0.039 | 0.128 |
| Abruzzo | 22.03.2020 | 3375 | 587 | 33 | 0.056 | 0.174 |
| Umbria | 22.03.2020 | 3135 | 521 | 16 | 0.031 | 0.166 |
| 21 Countries (with > 10 deaths)b | ||||||
| Italy | 3.04.2020 | 619,849 | 115,242 | 13,917 | 0.121 | 0.186 |
| Indonesia | 4.04.2020 | 7986 | 1986 | 181 | 0.091 | 0.249 |
| UK | 3.04.2020 | 173,784 | 33,722 | 2961 | 0.088 | 0.194 |
| Netherlands | 2.04.2020 | 75,415 | 13,614 | 1173 | 0.086 | 0.181 |
| France | 31.03.2020 | 224,254 | 58,327 | 4490 | 0.077 | 0.260 |
| Belgium | 3.04.2020 | 67,945 | 15,348 | 1011 | 0.066 | 0.226 |
| Ecuador | 2.04.2020 | 9604 | 2372 | 146 | 0.062 | 0.247 |
| Denmark | 3.04.2020 | 39,928 | 3386 | 123 | 0.036 | 0.085 |
| Japan | 3.04.2020 | 39,446 | 2617 | 65 | 0.025 | 0.066 |
| India | 27.03.2020 | 26,798 | 724 | 17 | 0.023 | 0.027 |
| USA | 3.04.2020 | 1,267,658 | 213,600 | 4793 | 0.022 | 0.168 |
| Turkey | 3.04.2020 | 141,716 | 18,135 | 356 | 0.020 | 0.128 |
| Ireland | 31.03.2020 | 30,213 | 2910 | 54 | 0.019 | 0.096 |
| South Korea | 3.04.2020 | 443,273 | 10,062 | 174 | 0.017 | 0.023 |
| Malaysia | 3.04.2020 | 47,723 | 3116 | 50 | 0.016 | 0.065 |
| Pakistan | 3.04.2020 | 30,308 | 2450 | 35 | 0.014 | 0.081 |
| Austria | 4.04.2020 | 104,134 | 11,129 | 158 | 0.014 | 0.107 |
| Canada | 1.04.2020 | 256,933 | 11,372 | 152 | 0.013 | 0.044 |
| Estonia | 3.04.2020 | 19,091 | 858 | 11 | 0.013 | 0.045 |
| Germany | 29.03.2020 | 918,460 | 52,547 | 389 | 0.007 | 0.057 |
| Australia | 3.04.2020 | 277,278 | 5224 | 23 | 0.004 | 0.019 |
aData source: www.protezionecivile.gov.it/
bData sources: for total tests performed—https://ourworldindata.org/ and for positive tests and deaths—www.who.int/
Fig. 1.
The relationship between COVID-19 testing success (a ratio of positive tests and total tested) and case fatality rate (CRF) (a ratio of deaths and positive tests) in 14 Italian regions with at least 10 cases of deaths due to COVID-19 as of 22 March 2020 (Spearman rank correlation coefficient ρ = 0.657; p < 0.01).
Data source: www.protezionecivile.gov.it/
The observations from Vò Euganeo are in agreement with COVID-19 data observed on a large scale and potentially explain the marked discrepancies in outbreak severity across countries. For instance, South Korea is similar to Italy in both the population (55 million and 60 million, respectively) and the average life expectancy (82 and 83.4 years, respectively), yet the impact of COVID-19 is different. The number of infected people in South Korea totalled 9000 with about 110 deaths equivalent to a lethality rate of 1.2%. As of March, more than 300,000 people had been tested in South Korea. The results showed that 55% of asymptomatic infected people were responsible for the 80% of symptomatic patients. Among infected, 33% were in the age range of 20 through 29 years (Data mentioned in the text were taken, at the time of the article submission, from the official site of South Korea government, http://ncov.mohw.go.kr/en).
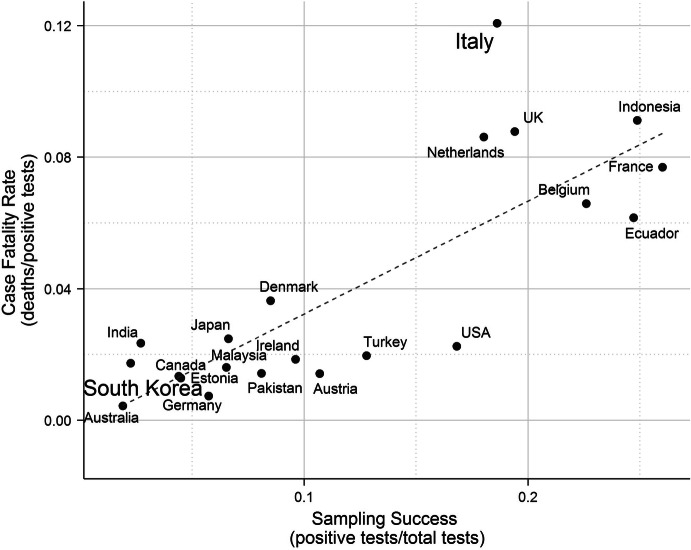
We then compiled data on the number of performed tests, positive tests, deaths, testing success and CRF in 21 countries with more than 10 deaths due to COVID-19 reported by the end of March to the beginning of April 2020 (Table 1). The relationship between the COVID-19 positive testing and case fatality rates across 21 countries is strong (Spearman rank correlation coefficient ρ = 0.739; p ≪ 0.01). The difference between two countries Italy and South Korea in terms of a testing success, defined as a ratio of positive tests and total tested and CFR is quite apparent (Fig. 2). These findings conform to data from a study conducted in Wuhan just before the lockdown of the Hubei area in China. That study shows 55% of undocumented cases of COVID-19 were responsible for 79% of documented cases [8].
Fig. 2.
The relationship between COVID-19 testing success (a ratio of positive tests and total tested) and case fatality rate (CRF) (a ratio of deaths and positive tests) in 21 countries with more than 10 deaths as of 3 March 2020 (Spearman rank correlation coefficient ρ = 0.739; p < < 0.01). Data sources: for total tests performed—https://ourworldindata.org/ and for positive tests and deaths—www.who.int/
Concluding remarks
We want to stress that testing strategy appears to enormously affect the virus spread. A lack of definitive procedures and protocols, including guidance on clean and dirty routes for patient hospitalization, further increased virus transmission and its consequences. The high risk of exposure combined with the prolonged work shift hours, yet a low number of tests administered to doctors and healthcare workers, contributed to a high toll of severe disease and deaths among doctors and healthcare professionals.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sergio Romagnani and Raffaele De Palma are the first authors.
Contributor Information
Sergio Romagnani, Email: sergio.romagnani@unifi.it.
Raffaele De Palma, Email: raffaele.depalma@unige.it.
References
- 1.Berger K. The man who saw the pandemic coming. Nautilus Retrieved, March 10, 2020
- 2.Coronavirus disease 2019 (COVID-19) symptoms. CDC USA, January 30, 2020
- 3.Chen N, Zhan M, Dang X, et al. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hui DS, Hazar E, Madam DA, et al. 2019-nCoV epidemic threat of novel coronavirus to global health—the latest 2019 novel coronavirus outbreak in Wuhan. China J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coronavirus Disease 2019 (COVID-19) transmission. CDC, March 17, 2020
- 6.CDC tests for 2019-nCoV. CDC, February 12, 2020
- 7.Laboratory tests for 2019 novel coronavirus (2019-nCoV in suspected human cases. WHO, March 13, 2020)
- 8.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]