Abstract
We assessed the appropriateness of initiating antibiotics in 49 nursing home (NH) residents receiving antibiotics for urinary tract infection (UTI) using 3 published algorithms. Overall, 16 residents (32%) received prophylaxis, and among the 33 receiving treatment, the percentage of appropriate use ranged from 15% to 45%. Opportunities exist for improving UTI antibiotic prescribing in NH.
Antibiotics are among the most commonly prescribed drugs in nursing homes (NHs), and between 25% and 75% of antibiotic prescriptions in this setting may be inappropriate.1 A frequent driver of antibiotic use is urinary tract infection (UTI), which accounts for 20%–60% of systemic antibiotic courses administered in NHs.2 Examples of inappropriate UTI prescribing include administration for UTI prophylaxis3 and antibiotic treatment without documented signs or symptoms.4 Using data collected during a 1-day point prevalence survey of antimicrobial use in 9 community-based NHs, we applied 3 published algorithms to assess appropriateness of antibiotic initiation among residents treated for UTI indications.
METHODS
From an antimicrobial use point-prevalence survey involving 1,272 nursing home residents in 4 states,5 we identified those who received antibiotics for a UTI indication. We evaluated data collected on resident demographics, antibiotics used, rationale for use (either treatment or prophylaxis), clinical presentations, and diagnostic testing. We applied 3 published algorithms identified through literature review to determine the proportion of treatment initiation that was appropriate. They include (1) the revised McGeer criteria, intended for retrospective infection surveillance in long-term care settings, which require a combination of clinical signs and symptoms with a positive urine culture6; (2) the Loeb minimum criteria, which outline the minimum clinical signs and symptoms present before initiating antibiotics in NH residents7; and (3) an algorithm proposed by Crnich and Drinka8 (Crnich algorithm) for diagnosing UTI and initiating antibiotic therapy in NH residents, which is based on Infectious Diseases Society of America (IDSA) UTI treatment recommendations9 and includes a combination of clinical signs and symptoms along with results from urinalysis and urine cultures. Analyses and descriptive statistics were calculated using SAS version 9.3 software (SAS Institute, Cary, NC).
RESULTS
Of 1,272 NH residents, 141 (11.1%) received antibiotics on the day of the survey. Of these 141 NH residents, 50 (35%) received antimicrobials for a UTI indication. Of these 50 residents, 82% were female, 18% were short stay residents, 12% had an indwelling urinary catheter, and the median age was 82 years (range, 56–99). In total, 52 antibiotics were prescribed for UTI; the most common were trimethoprim/sulfamethoxazole (n = 17; 33%), ciprofloxacin (n = 10; 19%), and nitrofurantoin (n = 9; 17%). Rationale for antibiotic use for residents were documented as treatment for 33 (66%) and as prophylaxis for 16 (32%); the rationale for 1 resident was missing.
Of the 33 residents receiving antibiotics for UTI treatment, 28 (85%) had a urine culture performed (26 positive, 1 negative, and 1 result unknown); 23 (67%) had a urinalysis performed (22 were positive, 1 negative); and 5 (15%) had no urine testing documented. Moreover, 14 residents (42%) had ≥1 localizing UTI sign or symptom (Table 1). Overall, 6 residents (18%) had fever (a systemic infection sign included in all 3 algorithms) and positive urine culture; 5 of these 6 residents had no localizing UTI signs and symptoms. Of the 10 residents (30%) that had an acute mental status change documented, 58% had confusion but only 1 met the criteria for delirium; 4 (12%) had documented acute functional decline in activities of daily living.
TABLE 1.
Clinical Characteristics of Residents Given an Antibiotic for Therapeutic Treatment of Urinary Tract Infection (n = 33)
| Variable | No. | % |
|---|---|---|
| Localizing signs or symptomsa | 14 | 42 |
| Dysuria | 8 | 57 |
| Suprapubic pain or tenderness | 4 | 29 |
| Increased frequency | 3 | 21 |
| Acute costovertebral angle pain or tenderness | 2 | 14 |
| Incontinence | 1 | 7 |
| Gross hematuria | 1 | 7 |
| Increased urgency | 1 | 7 |
| Fever | 6 | 18 |
| Acute mental status changea | 10 | 30 |
| Confusion | 7 | 58 |
| Altered level of consciousness | 3 | 25 |
| Disorganized thinking | 2 | 17 |
| Deliriumb | 1 | 8 |
| Acute functional decline | 4 | 12 |
Not mutually exclusive.
Delirium is defined as an acute mental status change plus altered level of consciousness and disorganized thinking.
Other findings documented in the medical record included nonspecific behavioral changes (eg, agitation, violent behavior, anxiety) in 6 residents (18%), and 9 residents (30%) had urine described as cloudy or foul smelling.
The appropriateness of antibiotic initiation according to each algorithm was calculated among the 33 residents treated for UTI (Figure 1). Antibiotic initiation for UTI was deemed appropriate in 5 residents (15%) based on the revised McGeer Criteria, 10 residents (30%) based on the Loeb minimum criteria, and 15 residents (45%) based on the Crnich algorithm.
FIGURE 1.
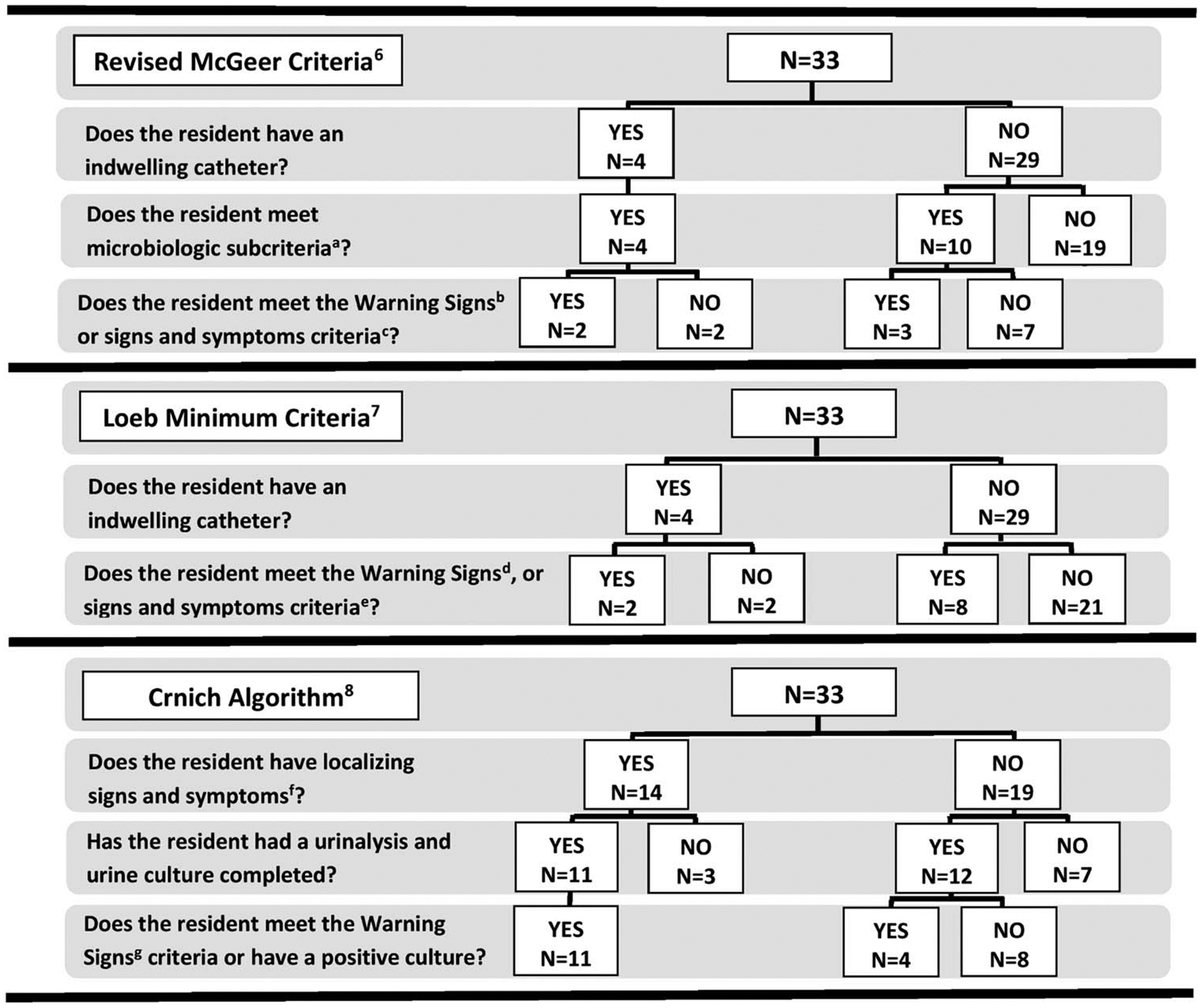
Appropriateness of antibiotic initiation in nursing-home residents for therapeutic treatment of urinary tract infection (n = 33).(a) Microbiologic subcriteria includes at least 105 cfu/mL of no more than 2 species of microorganisms in a voided urine sample or 105 cfu/mL of any organism from a urinary catheter specimen. (b) McGeer warning signs of an infection for all residents include fever (single oral temperature of >100°F [37.8°C] or repeated oral temperatures >99°F [> 37.5°C] or rectal temperatures >99.5°F [> 37.5°C] or single temperature >2°C [1.1°C] over baseline from any site), leukocytosis, rigors, new onset of hypotension, and only for residents with an indwelling urinary catheter, delirium, purulent discharge, or suprapubic pain or tenderness. (c) McGeer localizing signs and symptoms for all residents include acute dysuria or acute pain, swelling, or tenderness of the testes, epididymis, or prostate, increased urgency, increased frequency, gross hematuria, acute costovertebral angle pain or tenderness, or increased incontinence, and only for residents without an indwelling urinary catheter, suprapubic pain. (d) Loeb warning signs of infection for all residents include fever (>100°F [37.9°C] or an increase of 2.4°F [1.5°C] above baseline temperature), and only for residents with an indwelling urinary catheter rigors, delirium, or costovertebral tenderness. (e) Loeb localizing signs and symptoms for all residents include new or worsening urgency, frequency, suprapubic pain, gross hematuria, or dysuria, and only for residents without an indwelling urinary catheter, costovertebral angle tenderness. (f) Crnich localizing signs and symptoms for all residents include acute dysuria, new urgency, frequency, or incontinence, acute gross hematuria, costovertebral tenderness, suprapubic pain, new scrotal/prostate tenderness, or purulent urethral discharge. (g) Crnich warning signs of an infection for all residents include fever (as defined by McGeer Criteria), rigors, delirium, unstable vital signs, which were defined as decreased oxygenation, respiratory rate ≥25 breaths per minute, or new onset of hypotension. (h) Delirium is defined as an acute mental status change plus altered level of consciousness and disorganized thinking.
DISCUSSION
Our analysis of data collected during a 1-day point-prevalence survey among NH residents found that antibiotic initiation for UTI treatment was appropriate in only 15% to 45% of residents, depending upon the algorithm used. Studies evaluating use of antibiotics for NH residents have estimated the overall appropriateness to range from 25% to 75%.2 However, interpreting these findings is challenging due to the use of different definitions for appropriateness. To better understand the impact of these differences, we sought to describe the range of proportions of UTI antibiotic appropriateness by applying 3 published algorithms to the same data set. Regardless of the algorithm used, the percentage of appropriate antibiotic administration for UTI was <50%. Thus, improving antibiotic prescribing for UTI in NHs, a common antibiotic indication in this population, could have a significant impact on overall antibiotic use in NHs.
The lowest proportion of appropriate use (15%) was calculated using the revised McGeer criteria.6 While previously used to measure antibiotic appropriateness, the McGeer criteria are intended for infection surveillance purposes and are not suitable to guide decisions on antibiotic use.8 In contrast, the Loeb minimum criteria published in 2001 were developed specifically to guide the initiation of antibiotics. Using this algorithm, the percent appropriate increased to 30%. The Crnich algorithm published in 2014 was developed to specifically guide treatment for the initiation of antibiotics for UTI; this yielded a 45% level of appropriateness. This algorithm combines elements from Loeb with updated ISDA clinical practice guidelines to encourage use of UTI diagnostic testing only when evidence-based localizing urinary or systemic signs or symptoms are present. While the Crnich algorithm contains more elements than Loeb, we did not find it complicated to apply.
Only 42% of NH residents who received antibiotics for UTI treatment had 1 or more localizing UTI signs or symptoms documented. According to IDSA guidelines, antimicrobials should not be used to treat bacteriuria in older adults unless specific urinary tract symptoms are present.9 In addition, one-third of antibiotics were documented for UTI prophylaxis. We did not collect sufficient information to determine whether this prophylactic use was appropriate; however, very few situations warrant the use of antibiotics for UTI prophylaxis.3 Therefore, we surmise that much of the antibiotic use for UTI prophylaxis among NH residents is not appropriate.
We acknowledge the following limitations to our evaluation. Our results may underestimate appropriateness due to the retrospective nature of medical record review and the possibility of incomplete documentation. Additionally, this analysis does not reflect overall appropriateness. Our measures only assessed the initiation of antibiotics for UTI, without considering other aspects of appropriate prescribing (eg, drug selection, dosing, or duration). Notably, we did not determine whether NHs used antibiotic prescribing protocols or treatment guidelines, which prevented us from evaluating compliance with facility-specific protocols or other clinical practice guidelines.
Our findings demonstrate that opportunities exist for nursing homes to improve their use of antibiotics for UTI. They include (1) education on the use of UTI diagnostic testing only in the presence of relevant signs or symptoms, (2) implementing an algorithm-based UTI management protocol, which have been demonstrated to reduce antibiotics without increases in hospitalizations or deaths among nursing homes residents,10 and (3) evaluation of and feedback on prescriber performance against the protocol, as recommended by the CDC.11 Because antibiotic use for UTI in nursing homes is common, these antibiotic stewardship efforts would likely significantly reduce inappropriate prescribing practices.
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support: No financial support was provided relevant to this article.
Footnotes
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.
PREVIOUS PRESENTATION: An abstract of this work, “Measuring Antibiotic Appropriateness for Urinary Tract Infection in Nursing Home Residents,” was presented in Atlanta, Georgia, on May 20, 2016, at the Society for Healthcare Epidemiologists of America Spring Conference.
REFERENCES
- 1.Nicolle LE, Bentley DW, Garibaldi R, Neuhaus EG, Smith PW. Antimicrobial use in long-term-care facilities. SHEA Long-Term-Care Committee. Infect Control Hosp Epidemiol 2000;21:537–545. [DOI] [PubMed] [Google Scholar]
- 2.Rotjanapan P, Dosa D, Thomas KS. Potentially inappropriate treatment of urinary tract infections in two Rhode Island nursing homes. Arch Intern Med 2011;171:438–443. [DOI] [PubMed] [Google Scholar]
- 3.Giannella M, Tedeschi S, Bartoletti M, Viale P. Prevention of infections in nursing homes: antibiotic prophylaxis versus infection control and antimicrobial stewardship measures. Expert Rev Anti Infect Ther 2016;14:219–230. [DOI] [PubMed] [Google Scholar]
- 4.Phillips CD, Adepoju O, Stone N, et al. Asymptomatic bacteriuria, antibiotic use, and suspected urinary tract infections in four nursing homes. BMC Geriatr 2012;12:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson N, LaPlace L, Epstein L, et al. Prevalence of antimicrobial use and opportunities to improve prescribing practices in US nursing homes. J Am Med Dir Assoc Issue 2016. October 14 pii S1525–8610:30365–30366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stone ND, Ashraf MS, Calder J, et al. Surveillance definitions of infections in long-term care facilities: revisiting the McGeer criteria. Infect Control Hosp Epidemiol 2012;33:965–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loeb M, Bentley DW, Bradley S, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol 2001;22:120–124. [DOI] [PubMed] [Google Scholar]
- 8.Crnich CJ, Drinka PJ. Improving the management of urinary tract infections in nursing homes: it’s time to stop the tail from wagging the dog. Ann Long Term Care 2014:43–47. [Google Scholar]
- 9.Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 2005;40:643–554. [DOI] [PubMed] [Google Scholar]
- 10.Loeb M, Brazil K, Lohfeld L, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomized controlled trial. BMJ 2005. September 24;331(7518):669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The core elements of antibiotic stewardship for nursing homes. Centers for Disease Control and Prevention website. http://www.cdc.gov/longtermcare/index.html. Published 2015. Accessed April 20, 2017. [Google Scholar]


