Supplemental Digital Content is available in the text.
Abstract
During the coronavirus disease 2019 (COVID-19) pandemic, infectious disease control is of utmost importance in acute stroke treatment. This is a new situation for most stroke teams that often leads to uncertainty among physicians, nurses, and technicians who are in immediate contact with patients. The situation is made even more complicated by numerous new regulations and protocols that are released in rapid succession. Herein, we are describing our experience with simulation training for COVID-19 stroke treatment protocols. One week of simulation training allowed us to identify numerous latent safety threats and to adjust our institution-specific protocols to mitigate them. It also helped our physicians and nurses to practice relevant tasks and behavioral patterns (eg, proper donning and doffing PPE, where to dispose potentially contaminated equipment) to minimize their infectious exposure and to adapt to the new situation. We therefore strongly encourage other hospitals to adopt simulation training to prepare their medical teams for code strokes during the COVID-19 pandemic.
In acute stroke treatment, every minute counts. Most hospitals have well-functioning protocols to optimize door to needle times for intravenous thrombolysis and door to groin puncture times for endovascular treatment. Until now, when treating patients with acute stroke, there was no need to put special emphasis on infectious disease control, personal protection, and patients’ respiratory symptoms. During the coronavirus disease 2019 (COVID-19) pandemic, however, infectious disease control is of utmost importance. This often leads to uncertainty on the part of the physicians who manage the patient and among the nurses and technicians with immediate patient contact. The medical team might also be much larger with additional anesthesia and critical care staff with varying levels of information, experience with personal protection equipment, and with different levels of anxiety. The latter one is partly driven by the fact that healthcare workers themselves are at high risk of obtaining and transmitting the virus, and in many parts of the world, this has already led to staff shortages. Thus, the remaining healthcare workers are often required to take on new responsibilities and tasks with which they are mostly unfamiliar and often uncomfortable.
How Can Simulation Training Help to Improve This Situation?
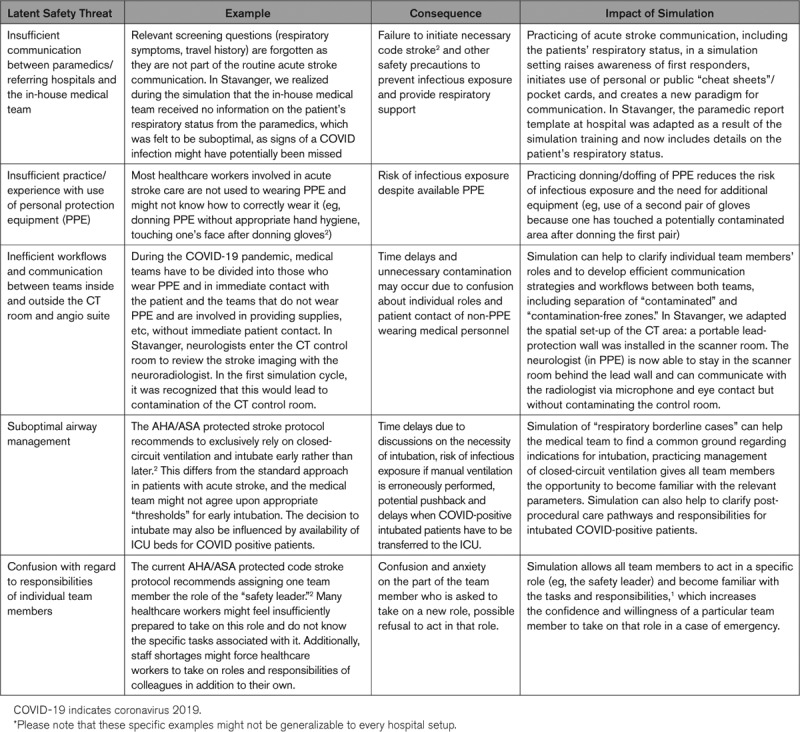
Simulation can help to (1) identify latent safety threats and (2) practice newly established protocols, thereby (3) reducing the mental strain of healthcare workers.1 This has the potential to improve the safety for patients and healthcare workers themselves. The current American Heart Association protected code stroke protocol acknowledges this and states that “simulation training, especially in-situ, can alleviate the anxiety of the situation and reduce safety threats”.2 The Table provides specific examples of situations in which simulation training can help to identify safety threats and initiate necessary workflow modifications to mitigate those.
Table.
Examples for the Impact of Simulation Training in Overcoming Latent Safety Threats During the COVID-19 Pandemic*
Code-Stroke Simulation in a Patient With COVID-19 Exposure: the Stavanger Experience
In Stavanger, we have conducted regular simulation-based team-training for intravenous thrombolysis and endovascular stroke treatment for >3 years.3 In reaction to the COVID-19 pandemic, we created a simulation scenario that involved a patient with COVID-19 positive code stroke with left-sided paresis and dysarthria and an underlying large vessel occlusion (for a detailed scenario description, see the Data Supplement). All participating healthcare workers received a brief explanation on the use of personal protective equipment, the current local COVID-19 code stroke protocol, and specific information about implemented infection control safeguards. We repeated this simulation scenario on a daily basis for 1 week. During the simulation cycles, we detected numerous latent safety threats, for example, potential contamination of the CT control room, risk of infectious exposure during intravenous alteplase administration, and lack of detail in assessing the patient’s respiratory status (Table). The workflow protocol was then adjusted. Protocol adjustments ranged from small changes (eg, defining where PPE donning should be done, and change of communication details), to more comprehensive changes such as planning and effectuating a lead wall in the CT scan room. The new and adapted protocol was then used for the following simulation sessions. We continuously communicated protocol changes to all relevant personnel. The focus of the simulation training was to get all relevant personnel through at least one simulation training before standing at the front line with a real patient. There was no final “examination,” but a debrief after the simulation run addressed points of improvement. Our presimulation assessment showed that initially, only 15% of the simulation participants were completely comfortable with their role in the local COVID-19 stroke treatment workflow. After one simulation cycle, this number increased to 80%. Additionally, over 60% of the participants stated that they identified at least one latent safety threat that would have led to infectious exposure of themselves or a team member. Although we are still training and adapting the protocols, after 1 week of simulation training, we were much better organized when our first patient with COVID-19 positive stroke arrived. We therefore strongly recommend every stroke center to go through this exercise. It does not take much of equipment: a simulation mannequin or a team member acting as the patient and a video camera or an attentive observer is all that is needed.
We do realize that there are several limitations of this experience, and each institution will have its own bottlenecks, protocols, and practical limitations. However, although it is hard to address all these unique circumstances in a “universal” protocol, simulation can help hospitals identify latent safety threats that are specific to their institution and to develop and optimize individually tailored, institution-specific protocols. But not only can simulation training improve performance of healthcare workers on the frontlines, it also helps them to get familiar with their new tasks, thereby alleviating the tremendous mental strain that each and every one of us has to face during these challenging times.
Acknowledgments
We are most grateful to all physicians who participated in the simulation training. All authors participated in the conceptualization, drafting, and critical revision of the manuscript.
Disclosures
Dr Ospel is supported by the University of Basel Research Foundation, Julia Bangerter Rhyner Foundation, and Freiwillige Akademische Gesellschaft Basel. Dr Goyal is a consultant for Medtronic, Stryker, Microvention, GE Healthcare, Mentice. Dr Kurz reports a research grant from The Laerdal Foundation. The other author reports no conflicts.
Supplementary Material
Footnotes
For Sources of Funding and Disclosures, see page xxx.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.120.030091.
References
- 1.Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf. 2013;22:468–477. doi: 10.1136/bmjqs-2012-000942. doi: 10.1136/bmjqs-2012-000942. [DOI] [PubMed] [Google Scholar]
- 2.Khosravani H RP, Notario L, Chapman M, Menon BK. Hyperacute stroke management during the coronavirus disease 2019 (covid-19) pandemic [published online April 1, 2020]. Stroke. 2020 doi: 10.1161/STROKEAHA.120.029838. doi: STROKEAHA120029838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ajmi SC, Advani R, Fjetland L, Kurz KD, Lindner T, Qvindesland SA, et al. Reducing door-to-needle times in stroke thrombolysis to 13 min through protocol revision and simulation training: a quality improvement project in a Norwegian stroke centre. BMJ Qual Saf. 2019;28:939–948. doi: 10.1136/bmjqs-2018-009117. doi: 10.1136/bmjqs-2018-009117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


