Abstract
We investigated the association of some environmental and economic factors and the global distribution indicators of the COVID-19 pandemic. Since the number of cases and deaths is higher in high-income countries located in higher latitudes and colder climates, further studies are required to shed light on this matter.
Keywords: COVID-19, Latitude, Temperature, Gross domestic product
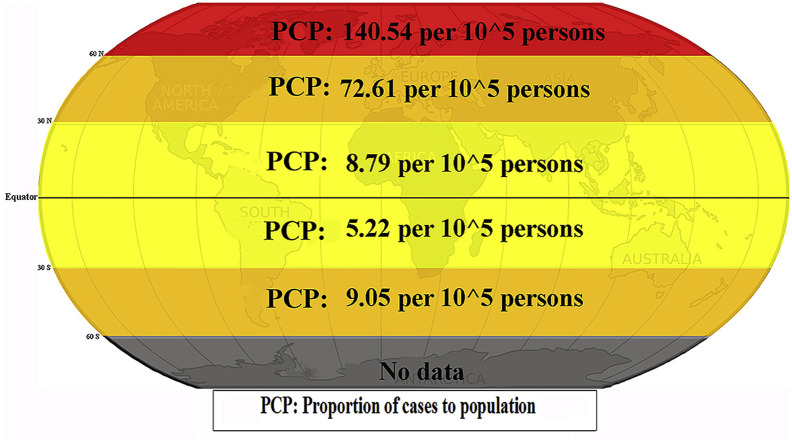
Graphical abstract
1. Introduction
Following the epidemic outbreak of COVID-19 in Wuhan, China, in December 2019 (Chen et al., 2020), most countries are currently in a pandemic situation. The behavior of this disease is extremely sophisticated and is the main topic of discussion in academic circles. The maps describing COVID-19 are being updated every day; however, almost all these maps have focused on the number of disease cases and the death number. At present, drawing maps and performing analyses based on other parameters such as latitude and socioeconomic factors could be useful for researchers and health policy-makers.
2. Methods
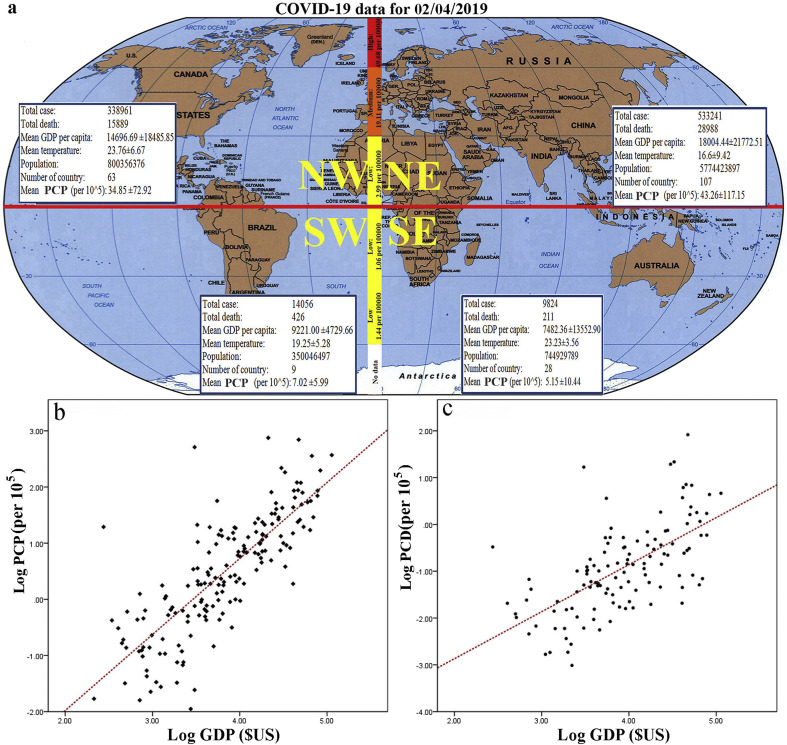
We employed the WHO report (Organization, 2020) as the main source of COVID-19 data based on the last update on April 2, 2020. Initially, the equator and the prime meridian were used for dividing the world into four parts: northeastern, northwestern, southeastern, and southwestern (Fig. 1 , a). Based on primary COVID-19 data, two main variables of this study included the proportion of cases to population per 105 (PCP) and the proportion of death to population per 105 (PDP). Other parameters were the average temperature (oC) and GDP ($US) of countries, which were extracted from different websites (World Economic Outlook Database, 2019; WORLD BANK GROUP, 2020). A descriptive analysis was performed on all the data. Bivariate correlation and regression test were used to analyze the associations between socioeconomic and meteorological factors (temperature, GDP, latitude, and longitude) and the variables of COVID-19. Also, the scatter plot of log case and death rate with log GDP was drawn using SPSS. All the statistical analyses were performed at a 5% significance level .(see: Fig 1).
Fig. 1.
Charactersistic and distribution map of COVID-19 in the world; a) category of earth and COVID-19 details in every part and proportion of cases to population per 105 (PCP) (highlight line) in each latitude category (0-30°, 30-60° and 60-90°), b) The correlation between Log PCP of COVID-19 with GDP per capita ($) (R = 0.799, Unstandardized Coefficients = 1.354, SE = 0.078, F = 300.587, P < 0.001), c) The correlation between Log PDP of COVID-19 with GDP per capita ($) (R = 0.630, Unstandardized Coefficients = 1.005, SE = 0.115, F = 76.518, P < 0.001).
3. Results and discussion
The results showed that the majority of cases (533241) were observed in northeastern areas, the more COVID-19 PCP (43.26 per 105 people), were also appeared northeast. The pattern of PDP was similar to the case rate, and the highest death rate was found in the northeast (1.63 per 105). Categorizing the COVID-19 case rate based on latitude revealed that this variable is associated with the COVID-19 latitude (r = 0.54; p < 001). As it appears in Fig. 1a (the highlighted line passing through the prime meridian), in the latitude beyond 60°, a higher PCP of COVID-19, 104.54 per 105, is observed. Countries with a higher GDP had more COVID-19 PCP and PDP (Table 1 and Fig. 1b and c). Furthermore, temperature had a reverse association with both COVID-19 PCP (r = −0.50; p < 001) and PDP (r = −0.50; p < 001).
Table 1.
The correlation (r) between case and death of COVID-19 (per105 people) and independent variables up to April 2, 2020.
| Earth category | variable | GDP per capita ($) | Temperature (oC) | Latitude (degree) | Longitude (degree) |
|---|---|---|---|---|---|
| Globally | PCPa | 0.827** | −0.50** | 0.54** | −0.16* |
| PDPa | 0.50** | −0.50** | 0.38** | −0.18* | |
| North | PCPa | 0.82** | −0.51** | 0.53** | −0.22* |
| PDPa | 0.50** | −0.46** | 0.41** | −0.19** | |
| South | PCPa | 0.83** | −0.45* | 0.39** | 0.47** |
| PDPa | 0.57** | −0.25 | 0.054 | 0.12 |
**P < 0.01, *P < 0.05; PCP = proportion of cases to population per 105, PDP: proportion of deaths to population per 105.
While discussions about the results of COVID-19 distribution throughout the globe are inconclusive, we suggest some possible reasons for these findings. Interestingly, higher COVID-19 PCP and PDP were observed in northern areas, including some parts of North America and approximately the entire Asia and Europe which are located in higher latitudes and have a colder climate and better socioeconomic condition. To interpret these results, the authors suggest some major reasons for these data. First, the distribution patterns and the mentioned associations could be related to the availability of diagnostics kits and health care facilities (Bi et al., 2020; Coronavirus Testing, 2020). In addition, both colder climate and more densely populated areas could contribute to the spread of the disease in European and Asian megacities (Xie and Zhu, 2020; Sajadi et al., 2020).
Several studies have suggested that a higher temperature could be effective against different types of coronavirus such as SARS (Van Doremalen et al., 2013; Chan et al., 2011; Bi et al., 2007). In the study by Ma et al. (2020), it has been reported that there is a negative relationship between COVID-19 mortality and temperature (Ma et al., 2020) because at lower temperatures, the performance of the immune system, as well as the liver, is decreased; as a result, the situation will be conducive to the activity of infectious agents and virus transmission (Shephard and Shek, 1998; Donaldson et al., 1999; Steel et al., 2011; Li et al., 2019; Davis et al., 2016). Furthermore, the mortality rate and incidence of COVID-19 could be associated with air pollution and the average age of the population. It seems that older populations in the northern hemisphere, especially in Europe and North America with a higher income, have a higher death rate from respiratory infections (Michel, 2010; Cristea et al., 2020; Knickman and Snell, 2002; Eurostat, 2019). Additionally, it seems that air pollution plays a determinative role in COVID-19 outbreak and mortality. For instance, day-by-day changes of pollutant concentration were positively linked with the number of infected individuals in Italy; likewise, the number of confirmed cases was extremely higher in cities with more than 100 days of air pollution than cities with cleaner air (Coccia, 2020). A substantial relationship has also been found between urban air pollution and the transmission dynamics of COVID-19. In addition, it has been established that air pollutants emitted from vehicles and industries, such as nitrogen oxide and particle matter, may affect viral infection emission and increase the number of hospital admissions due to respiratory virus bronchiolitis and asthma (Carugno et al., 2018; Glencross et al., 2020; Groulx et al., 2018; Nenna et al., 2017).
While it is still not well established in the case of the coronavirus disease, vitamin D deficiency in people living in high-latitude areas and colder climates may somehow trigger the disease in those regions (Grant et al., 2020; Zhou et al., 2005; Barger-Lux and Heaney, 2002). Vitamin D supplementation is highly recommended for preventing acute respiratory diseases, but the effectiveness of vitamin D for coronavirus infection is in urgent need of further investigations. The authors of this short communication acknowledge possible limitations, including the fast-changing pattern of the disease and the deficiencies linked with the source of data. Environmentally speaking, there are many factors that may affect COVID-19 distribution and mortality, including humidity, wind speed, and air pressure. Besides, government-based interactions such as compulsory quarantine, social distancing, and advertising precaution measures could bring substantial benefits to cope with COVID-19 in different areas. We should also address intrinsic limitations and the fallacy of ecological research to some extent. We believe that this study can provide researchers with a deeper understanding of the coronavirus distribution pattern and the associated contributing factors. It is also suggested that, in the future, studies address the effect of public awareness, social distancing, quarantine effectiveness, and people's participation in isolation plans.
Funding
This study was funded by Neyshabur university of medical sciences by grant number 99-01-163..
Declarations
The authors have disclosed that they do not have any conflicts of interest.
Availability of data and materials
All data and materials used in this study were publicly available and mention in the text.
Consent for publication
Not applicable.
Credit author statement
Mohammad Sarmadi: Writing - original draft, Methodology, Software,Writing- Reviewing and Editing Nilufar Marufi.: Investigation, Writing- Original draft preparation, Software Vahid Kazemi Moghadam: Conceptualization, Supervision, Writing- Reviewing and Editing
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors would like to thank Neyshabur University of Medical Sciences for their financial support for performing this research (grant number: 99-01-163).
References
- Barger-Lux M.J., Heaney R.P. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J. Clin. Endocrinol. Metab. 2002;87(11):4952–4956. doi: 10.1210/jc.2002-020636. [DOI] [PubMed] [Google Scholar]
- Bi P., Wang J., Hiller J.E. Weather: driving force behind the transmission of severe acute respiratory syndrome in China? Intern. Med. J. 2007;37(8):550–554. doi: 10.1111/j.1445-5994.2007.01358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30287-5. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carugno M., Dentali F., Mathieu G., Fontanella A., Mariani J., Bordini L. PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy. Italy. Environ. Res. 2018;166:452–457. doi: 10.1016/j.envres.2018.06.016. [DOI] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.S.M., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011:734690. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020:138474. doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worldometer Coronavirus Testing . 2020. Criteria and Numbers by Country.https://www.worldometers.info/coronavirus/covid-19-testing Available from: [Google Scholar]
- Cristea M., Noja G.G., Stefea P., Sala A.L. The impact of population aging and public health support on EU labor markets. Int. J. Environ. Res. Publ. Health. 2020;17(4):1439. doi: 10.3390/ijerph17041439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis R.E., Dougherty E., McArthur C., Huang Q.S., Baker M.G. Cold, dry air is associated with influenza and pneumonia mortality in Auckland, New Zealand. Influenza Other Respir Viruses. 2016;10(4):310–313. doi: 10.1111/irv.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson G.C., Seemungal T., Jeffries D.J., Wedzicha J.A. Effect of temperature on lung function and symptoms in chronic obstructive pulmonary disease. Eur. Respir. J. 1999;13(4):844–849. doi: 10.1034/j.1399-3003.1999.13d25.x. [DOI] [PubMed] [Google Scholar]
- Eurostat . Imprimerie Bietlot in Belgium; Luxembourg: 2019. Ageing Europe LOOKING at the LIVES of OLDER PEOPLE IN the EU [Collection: Statistical Books]https://ec.europa.eu/eurostat/documents/3217494/10166544/KS-02-19%E2%80%91681-EN-N.pdf/c701972f-6b4e-b432-57d2-91898ca94893 [cited 2020 May 5]. 2019:[Available from: [Google Scholar]
- Glencross D.A., Ho T.-R., Camiña N., Hawrylowicz C.M., Pfeffer P.E. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 2020 doi: 10.1016/j.freeradbiomed.2020.01.179. [DOI] [PubMed] [Google Scholar]
- Grant W.B., Lahore H., McDonnell S.L., Baggerly C.A., French C.B., Aliano J.L. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):19. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groulx N., Urch B., Duchaine C., Mubareka S., Scott J.A. The Pollution Particulate Concentrator (PoPCon): a platform to investigate the effects of particulate air pollutants on viral infectivity. Sci. Total Environ. 2018;628–629:1101–1107. doi: 10.1016/j.scitotenv.2018.02.118. [DOI] [PubMed] [Google Scholar]
- Knickman J.R., Snell E.K. The 2030 problem: caring for aging baby boomers. Health Serv. Res. 2002;37(4):849–884. doi: 10.1034/j.1600-0560.2002.56.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M., Zhou M., Yang J., Yin P., Wang B., Liu Q. Temperature, temperature extremes, and cause-specific respiratory mortality in China: a multi-city time series analysis. Air Quality, Atmosphere & Health. 2019;12(5):539–548. [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel J.P. Updated vaccine guidelines for aging and aged citizens of Europe. Expert Rev. Vaccines. 2010;9(3 Suppl. l):7–10. doi: 10.1586/erv.10.27. [DOI] [PubMed] [Google Scholar]
- Nenna R., Evangelisti M., Frassanito A., Scagnolari C., Pierangeli A., Antonelli G. Respiratory syncytial virus bronchiolitis, weather conditions and air pollution in an Italian urban area: an observational study. Environ. Res. 2017;158:188–193. doi: 10.1016/j.envres.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization W.H. vol. 67. 2020. (Coronavirus Disease 2019 (COVID-19): Situation Report). [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. 2020. Temperature and Latitude Analysis to Predict Potential Spread and Seasonality for COVID-19. Available at: SSRN 3550308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shephard R.J., Shek P.N. Cold exposure and immune function. Can. J. Physiol. Pharmacol. 1998;76(9):828–836. doi: 10.1139/cjpp-76-9-828. [DOI] [PubMed] [Google Scholar]
- Steel J., Palese P., Lowen A.C. Transmission of a 2009 pandemic influenza virus shows a sensitivity to temperature and humidity similar to that of an H3N2 seasonal strain. J. Virol. 2011;85(3):1400–1402. doi: 10.1128/JVI.02186-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N., Bushmaker T., Munster V. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18(38):4. doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- World Bank Group Climate change knowledge portal. https://climateknowledgeportal.worldbank.org/. 2020. 2020 [Available from:
- World Economic Outlook Database . 2019. IMF.org. International Monetary Fund.https://www.worldometers.info/coronavirus/covid-19-testing/ 15 October 2019. Retrieved 22 Murch 2020. [Available from: [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W., Suk R., Liu G., Park S., Neuberg D.S., Wain J.C. Vitamin D is associated with improved survival in early-stage non-small cell lung cancer patients. Cancer Epidemiol. Biomark. Prev. 2005;14(10):2303–2309. doi: 10.1158/1055-9965.EPI-05-0335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials used in this study were publicly available and mention in the text.