Abstract
Aim
In response to the COVID-19 pandemic, there is a need for substantial changes in the procedures for accessing healthcare services. Even in the current pandemic, we should not reduce our attention towards the diagnosis and treatment of GDM. The purpose of this document is to provide a temporary guide for GDM screening, replacing the current guidelines when it is not possible to implement standard GDM screening because of an unfavorable risk/benefit ratio for pregnant women or when usual laboratory facilities are not available.
Data synthesis
At the first visit during pregnancy, we must exclude the presence of “Overt diabetes” in all women. The criteria for the diagnosis of overt diabetes are either fasting plasma glucose ≥126 mg/dL, or random plasma glucose ≥200 mg/dL, or glycated hemoglobin ≥6.5%. When the screening procedure (OGTT) cannot be safely performed, the diagnosis of GDM is acceptable if fasting plasma glucose is ≥ 92 mg/dL. In order to consider the impaired fasting glucose as an acceptable surrogate for the diagnosis of GDM, the fasting glucose measurement should be performed within the recommended time windows for the risk level (high or medium risk).
Conclusions
The changes to the screening procedure for GDM reported below are specifically produced in response to the health emergency of the COVID-19 pandemic. Therefore, these recommended changes should cease to be in effect and should be replaced by current national guidelines when the healthcare authorities declare the end of this emergency.
Introduction
In response to the COVID-19 pandemic, there is need for substantial changes in the procedures for accessing healthcare services for all subspecialties. The care for expecting mothers is special, because pregnancy requires control visits at specific times to assess that the unborn child is developing normally, and, essential for this to happen, that the mother is in good health.
The Prime Ministry Decree dated March 11, 2020, details measures for the containment of Coronavirus infection, including travel limitations of individuals throughout the country, closure of non-essential businesses and public places, etc. Listed among the exceptions is the possibility for patients to travel for “outpatient visits during pregnancy”. The decree confirms the current organization of the network for maternal-neonatal care in an outpatient setting, such as outpatient family services (Consultori), as well as in the hospital setting. Diagnostic imaging, laboratory testing, and other procedures specific for a certain gestational age are also guaranteed if all recommended safety measures are in place.
Gestational diabetes (GDM) is a condition that, if not promptly recognized and treated, translates into an increased risk of maternal and fetal complications, both in the short and long term. There is currently no evidence of a relationship between COVID-19 and GDM, but it is known that hyperglycemia worsens the immune response to infections and that the associated inflammatory state, in turn, worsens insulin resistance. Therefore, even in the current pandemic, we should not reduce our attention towards the diagnosis and treatment of GDM.
In Italy, the screening and diagnosis of GDM follows the guidelines published in 2011 by the Istituto Superiore di Sanità (ISS). According to the risk of GDM, an Oral Glucose Tolerance Test (OGGT) at 16–18 gestational weeks is prescribed in high risk cases and at 24–28 gestational weeks in medium risk cases. Screening is not recommended for women at a low risk of GDM. High risk women with a normal OGTT at 16–18 gestational weeks repeat the OGTT at 24–28 gestational weeks.
The purpose of this document is to provide a TEMPORARY guide for GDM screening, replacing the current guidelines when it is not possible to implement standard GDM screening because of an unfavorable risk/benefit ratio for pregnant women or when usual laboratory facilities are not available:
-
1.
The changes to the screening procedure for GDM reported below are specifically produced in response to the health emergency of the COVID-19 pandemic.
-
2.
Therefore, these recommended changes should cease being in effect and be replaced by current guidelines [LG ISS Physiological Pregnancy and SID/AMD 2018 Standard of Care [1,2] and subsequent updates] when the healthcare authorities declare the end of this national health emergency.
-
3.When drafting these recommendations, we took into account the following considerations:
-
a.Currently available scientific evidence does not recognize any alternative to the 75-g oral glucose tolerance test with sampling for blood glucose measurements at 0 ′, 60′, and 120′ post-load. Therefore, the OGTT remains the gold standard for the diagnosis of GDM;
-
b.The health emergency we are facing is unprecedented, and Coronavirus transmission has specific, although not completely known, characteristics;
-
c.The risk/benefit ratio contingent on this situation.
-
a.
On these bases, we recommend the implementation of the following changes to the algorithm for the screening of GDM and to the usual schedule of outpatient visits, when an unfavorable risk/benefit ratio is identified by the team making the exposure of the pregnant woman to the risk of Coronavirus transmission, or if the healthcare system can only provide limited services.
-
1.
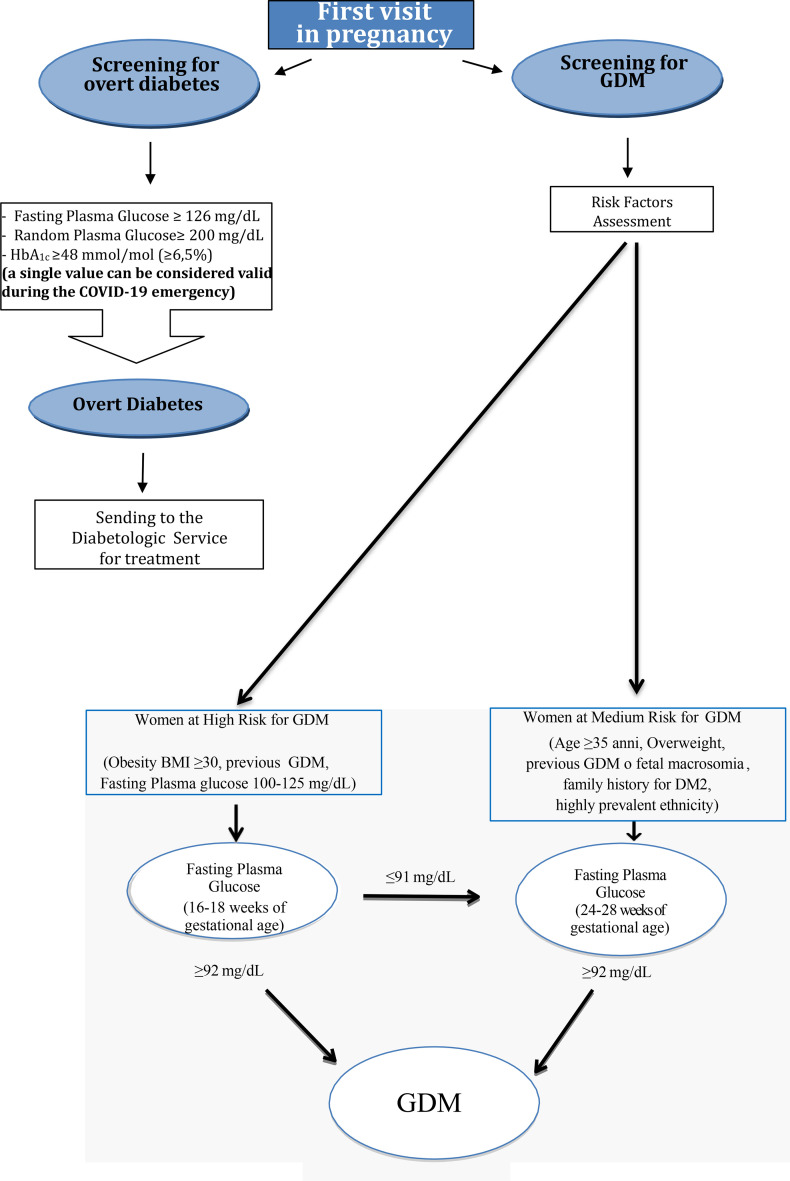
At the first visit during pregnancy, we must exclude the presence of an “Overt diabetes” in all women, as it may have been undiagnosed before pregnancy. The criteria for the diagnosis of overt diabetes are either fasting plasma glucose ≥126 mg/dL, or random plasma glucose ≥200 mg/dL, or glycated hemoglobin ≥6.5% (Fig. 1 ).
Figure 1.
Screening Procedure for GDM during COVID-19 emergency.
Rationale. Many studies have shown that pre-existing diabetes, if not recognized and promptly treated, is associated with adverse maternal and fetal outcomes. In particular, a recent Canadian study [3] analyzed the maternal and fetal outcomes of 995,990 women, documenting that 2.6% of them had pre-existing diabetes in pregnancy. Among those women, the risk of preterm birth, perinatal mortality, congenital malformations, and neonatal hypoglycemia was significantly higher than among women with GDM.
-
2. a
When the screening procedure (OGTT) cannot be safely performed, the diagnosis of GDM is acceptable even without performing the entire curve if fasting plasma glucose is ≥ 92 mg/dL. In order to consider the impaired fasting glucose, an acceptable surrogate for the diagnosis of GDM—the fasting glucose measurement—should be performed within the recommended time windows for the risk level (high or medium risk) defined by the aforementioned guide lines (LG ISS) [1] (Fig. 1).
-
b
In the event that screening for GDM is possible, the procedure should be carried out in compliance with the provisions of social distancing in place in all medical facilities. Both the expectant mother and the healthcare personnel should wear the recommended personal protective equipment (surgical mask and gloves).
Rationale. One single point of the OGTT above the recommended threshold is sufficient to diagnose GDM. Data in the literature suggest that fasting plasma glucose alone can be used to diagnose gestational diabetes, as sensitivity and specificity of fasting plasma glucose in a sample of 500 pregnant women were 88.8% and 95.2%, respectively [4]. Nonetheless, it is important to underline that this procedure, limited to the measurement of basal glucose alone, underestimates the cases of GDM; indeed, a certain percentage of GDM patients have basal glucose values < 92 mg/, while the post-load values at 1 and 2 h are abnormal. In addition, we should note that completing the sampling of the OGTT, even when a fasting diagnostic value is detected, allows for the detection of metabolic disorders that have a different clinical impact, and therefore helps to define the most appropriate therapeutic strategy by stratifying patients according to their metabolic and cardiovascular risk in the short and long term. Therefore, the OGTT as screening method for GDM has significant benefits for the woman and the fetus. During the COVID-19 pandemic, it is likely that the risk associated with performing the full OGTT may outweigh the benefit for the mother and the fetus when fasting blood glucose value is ≥ 92 mg/dL threshold. We state once more that a fasting glucose value can be considered diagnostic for GDM only when it is obtained at the gestational age when the OGTT should have been carried out, i.e., between 16–18 weeks in high-risk pregnant women or between 24 and 28 weeks in medium-risk women.
-
3.
After the diagnosis of GDM and the first visit to the diabetes center, periodic contact with patients will be maintained through telemedicine consultations.
Rationale. To reduce access to healthcare facilities, we need to define and implement shared standard management processes that include communication, recording, and monitoring tools. In Italy, diabetes clinics mostly share the same management software, and we are activating the option of downloading from remote capillary glucose data or from continuous glucose monitoring devices through several APPs or other sharing tools. It will be useful to define specific PDTAs that will provide management support for clinicians and will aim to harmonize the behavior of clinicians with innovative tools, such as telemedicine.
-
4.
To limit the need for patients to leave their homes to access a healthcare facility, it is important to coordinate the prescription and performance of laboratory tests and diagnostic imaging/procedures recommended by the various specialists involved in the management of pregnancy.
Rationale. Pregnancy complicated by GDM carries an increased risk of medium- and long-term complications for the mother and the fetus. In this sense, the management of hyperglycemia in pregnancy is particularly rigorous and it may require more frequent laboratory testing and diagnostic imaging/procedures to support treatment decisions (e.g., monitoring fetal growth parameters) and/or to detect complications early on. Clinicians need to assess the risk/benefit ratio for each individual patient, considering on one hand the increased risk of Coronavirus transmission with the access to a healthcare facility, and, on the other hand, the reduced risk of maternal and/or fetal complications because of early detection. This risk assessment also needs to be shared with the other specialists involved in the care of these women.
-
5.
Defer the postpartum OGTT to the end of the Coronavirus health emergency, except in cases where there is persistence of hyperglycemia after delivery (e.g., high capillary blood glucose values in the immediate postpartum period or high insulin requirement during pregnancy). In all cases, clinicians need to inform their patient about the importance of post-partum screening of glucose tolerance and attending follow-up visits, which, for the time being, can be carried out as telemedicine consultations, including the monitoring of nutrition during breastfeeding.
Rationale. A pregnancy complicated by GDM increases the risk of type 2 diabetes and cardiovascular diseases in the short and long-term after delivery. In Italy, the scientific societies SID and AMD recommend testing glucose tolerance with a 75-g OGTT, performed between 6 weeks and 6 months after delivery, to identify early impairment of glucose tolerance. Furthermore, they recommended assessing other metabolic parameters when necessary according to the patient's history. The primary concern during the current Coronavirus pandemic is to limit all unnecessary exposure of individuals to Coronavirus transmission. Therefore, although we recognize the importance of the post-partum assessment of glucose tolerance in women with GDM, this assessment should be postponed to the end of the current pandemic emergency. An exception to this policy is cases in which persistent hyperglycemia is documented. In these cases, through telemedicine consultation, the specialist may suggest the opportunity for further assessments.
-
6.
In pregnant women with GDM and a documented Coronavirus infection, it is recommended to intensify glucose control and management.
Rationale. In the literature, there are currently no reports of pregnancies complicated by GDM and COVID-19. In general, diabetes, while not increasing the risk of Coronavirus infection, does worsen the prognosis of COVID-19 [5]. In pregnant women with GDM and Coronavirus infection, insulin is the only recommended treatment of hyperglycemia, as the condition does not respond to nutritional management.
-
7.
Given the importance of fasting plasma glucose measurement in this recommendation, it is mandatory to respect standardized conditions of the pre-analytical phase, especially with regard to the choice of the appropriate anticoagulant, in order to avoid the occurrence of false negatives due to a reduction in blood glucose in vitro and to avoid excessive latency between samples collection and analysis [6].
C.F. The author's membership in AIFA does not involve the Institution in any way, as the work is the result of studies conducted on an individual basis.
Acknowledgments
The authors wish to acknowledge SIE (Società Italiana di Endocrinologia), SIBioC (Società Italiana di Biochimica Clinica e Biologia Molecolare Clinica), SIPMEL (Società Italiana di Patologia Clinica e Medicina di Laboratorio), SIGO (Società Italiana di Ostetricia e Ginecologia), AOGOI (Associazione degli Ostetrici e Ginecologi Ospedalieri Italiani), AGUI (Associazione Ginecologi Universitari Italiani).
AGEO (Associazione Ginecologi Extraospedalieri), and SIMP (Società Italiana di Medicina Perinatale) for their collaboration.
Handling Editor: G. Targher
References
- 1.Linee Guida Gravidanza Fisiologica ISS- CEVEAS http://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?id=1436
- 2.Standard di cura AMD-SID 2018. https://aemmedi.it/standard-di-cura/
- 3.Lee D., Booth G.L., Ray J.G., Ling V., Feig D.S. Undiagnosed type 2 diabetes during pregnancy is associated with increased perinatal mortality: a large population-based cohort study in Ontario, Canada. Diabet Med. 2020 Jan 28 doi: 10.1111/dme.14250. [Epub ahead of print] PubMed PMID: 31994233. [DOI] [PubMed] [Google Scholar]
- 4.Poomalar G.K., Rangaswamy V. A comparison of fasting plasma glucose and glucose challenge test for screening of gestational diabetes mellitus. J Obstet Gynaecol. 2013 Jul;33(5):447–450. doi: 10.3109/01443615.2013.771156. PubMed PMID: 23815193. [DOI] [PubMed] [Google Scholar]
- 5.Fadini G.P., Morieri M.L., Longato E., Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020 Mar 28 doi: 10.1007/s40618-020-01236-2. [Epub ahead of print] PubMed PMID: 32222956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonetti G., Carta M., Lapolla A., Miccoli R., Testa R., Mosca A. A in qualità di delegati SIBioC, Società Italiana di Patologia Clinica e Medicina di Laboratorio (SIPMeL) e Società Italiana di Diabetologia (SID) e per il Gruppo di Studio SIBioC-SIPMeL Diabete Mellito. Raccomandazioni per l’ottimizzazione della fase pre-analitica per una corretta determinazione della glicemia in ambito diabetologico. Biochim Clin. 2018;42:263–265. [Google Scholar]