Abstract
Disease advocacy organizations (DAOs) have traditionally focused on raising awareness of rare diseases, providing educational resources to patients, and supporting patients and families. Previous research has described how scientists collaborate with DAOs, but little empirical data are available regarding the extent to which physicians interact with DAOs and how those interactions impact patient care. We conducted a national survey of 230 board-certified pediatric neurologists to assess their engagement with DAOs and their beliefs about the impact of DAOs on patient care. In that context, we evaluated a set of 24 items describing interactions between physicians and DAOs. Exploratory factor analysis produced a 19-item model capturing four types of physician-DAO engagement: 1) accessing or distributing DAO-produced materials (6 items, alpha=0.80); 2) consulting on DAO activities (5 items, alpha=0.81); 3) collaborating with DAOs on research activities (6 items, alpha=0.80); and 4) co-producing scholarly materials with DAOs (2 items, alpha=0.80). Our data indicate that physicians engage with DAOs in more frequent and diverse ways than has been previously reported. Almost all physicians in our sample had interacted directly with a DAO in some way, from low-effort activities such as visiting a DAO’s website to deeper forms of engagement including co-authoring journal articles. These findings may provide a framework for bioethicists to characterize the nature and extent of physician interactions with advocacy organizations, which is critical for evaluating the ethical implications of physician-DAO relationships.
INTRODUCTION
Disease advocacy organizations (DAOs), also referred to as patient advocacy groups (PAGs), health social movements, and voluntary health agencies, have played an important role in patient empowerment. The first DAOs emerged in the 1950s in response to patient desires to play a more active role in their care (Koay and Sharp 2013; Aymé, Kole, and Groft 2008). In contrast to other medical organizations, DAOs have traditionally focused on raising public awareness of diseases, providing educational resources to newly diagnosed patients, and offering support to patients and families (Rose 2013; Hall 2013).
In recent years, DAOs have expanded their traditional role by supporting clinical research for specific diseases (Rose et al. 2017; Hall 2013). Previous studies have described how scientists collaborate with DAOs on research activities. In addition to providing financial support for clinical research (Sharp and Landy 2010), DAOs engage in study design, participant recruitment, data collection and interpretation, and dissemination of research results (Landy et al. 2012; Smith et al. 2015). In many cases DAOs have been credited with accelerating the research & development process for tests and treatments (Terry et al. 2007; Boon and Broekgaarden 2010; Institute of Medicine 2010) and for ensuring that research aligns more closely with patient values and priorities (Polich 2012).
DAOs appear to be expanding the scope of their influence to include patient-care settings as well. With increasing recognition of the expertise that patients bring to their care, and growing commitments to shared decision making in medicine, many DAOs view part of their role as preparing patients to take a more assertive role in clinical encounters (Keller and Packel 2014). Many of the education materials produced by DAOs include clinical recommendations, for example, and may be co-authored with clinicians, researchers, and pharmaceutical companies (Aymé, Kole, and Groft 2008). DAOs report that their constituents value information about treatment options, disease management, and healthcare providers (Keller and Packel 2014). In providing recommendations related to medical care, DAOs may complicate the physician-patient relationship, as clinicians may have mixed reactions to empowered patients whose knowledge is derived from the review of DAO websites (Hagan et al. 2017). In addition, commentators have raised concerns about the transparency of DAO ties to pharmaceutical companies, which may influence the advice they provide (Rose et al. 2017; McCoy et al. 2017).
Although the peer-reviewed literature has described DAOs indirectly influencing the clinical environment through interactions with patients and health policymakers, there is some evidence that DAOs are seeking to influence clinicians more directly. For example, a recent study reported that many DAOs view organizing professional conferences and changing professional attitudes as major organizational priorities (Keller and Packel 2014). In addition, to the extent that DAOs may work directly with physicians, it is unclear in what ways physicians may be interacting with DAOs. There is little evidence of physicians participating frequently in health advocacy and community engagement (Earnest, Wong, and Federico 2010). A 2004 survey of 1662 US physicians showed that 91.6% supported the idea of advocacy, but only 25.6% had actually engaged in some form of advocacy in the past 3 years (Gruen, Campbell, and Blumenthal 2006).
While scholars have examined some of the ethical implications of DAO expansion, most research has been related to the extent and implications of conflicts of interest (Koay and Sharp 2013). Several studies have investigated the relationship between DAOs and pharmaceutical companies or clinical researchers, but to our knowledge none have examined non-financial relationships among physicians and DAOs. As a result, it is unclear to what extent DAOs may be engaging clinicians or otherwise influencing patient-care activities. Understanding the scope of physician-DAO interactions is a crucial step in evaluating their ethical impact on patient care.
We examined physician interactions with DAOs via a national survey of physicians. Our aims were to describe the frequency and nature of physician-DAO interactions and to explore the types of physicians who engaged in those interactions. To encourage additional studies, we also identified four categories of activities that may be used as a framework to characterize physician-DAO interactions.
METHODS
Study population
The field of pediatric neurology was selected for this study since pediatric disorders are likely to inspire multiple forms of patient advocacy, particularly since affected patients are often unable to speak for themselves (Oberg 2003). Pediatric neurology also encompasses many rare diseases in which small numbers of patients may form very active support networks, often providing key sources of information on the disorder (Pauer et al. 2017). In addition, recent controversy regarding the information provided by autism-related advocates may have raised awareness of DAOs’ activities among specialists in pediatric neurology (The Autistic Self Advocacy Network et al. 2014).
Through the American Board of Psychiatry and Neurology (ABPN) “verifyCERT” system, 2268 board certified neurologists with special qualification in Child Neurology were identified (as of December 2013). The list of eligible pediatric neurologists was further refined by including only those for whom the research team was able to identify an active medical license number using publicly available state medical board websites and locate and confirm the provider’s current mailing address on a valid healthcare provider website. From the refined list of 1000 eligible physicians, 500 were randomly selected to be mailed a survey.
Survey
We developed a survey through collaboration and iterative revisions with researchers and CSR staff. The survey consisted of 78 distinct items grouped into 46 questions. These items assessed pediatric neurologists’ engagement with DAOs and their beliefs about the impact of DAOs on patient care. A definition of DAO was included at the beginning of the survey:
This survey is about non-profit, patient- or disease-oriented groups organized around specific diseases or conditions, for example the Muscular Dystrophy Association and the National Fragile X Foundation. These groups are also sometimes called “advocacy groups,” “patient advocacy groups,” or “Disease Advocacy Organizations.” For the purpose of this survey, we will use the acronym “DAO” throughout to refer to all advocacy groups in general.
Demographic questions were included in the survey to describe the characteristics of individual respondents and their medical practices. Physicians were asked to provide the city and state of their main practice location. Additionally, we included screening questions to confirm eligibility, which asked whether respondents were board certified in pediatric neurology and saw patients in a clinical setting at least 4 hours per week.
Data Collection
Surveys were sent in a Priority Mail envelope with a cover letter and postage-paid return envelope, along with a $20 prepaid cash incentive. Surveys were fielded from February to July 2015 by the Center for Survey Research at the University of Massachusetts Boston (CSR). A thank you/reminder postcard was sent to the entire sample after 3 weeks, and a second copy of the survey along with pre-paid return envelope was sent to non-responders after 6 weeks. Survey data were entered, verified, and cleaned by CSR staff. Data were also rechecked by two Mayo Clinic research assistants (CH, CN). The study was approved by the Mayo Clinic Institutional Review Board.
Data Analysis
Descriptive statistics were calculated using SAS. We analyzed frequencies, percentages, means, and standard deviations for all demographic and outcome variables. To evaluate physicians’ main practice locations, we determined the US Census region of the country, the city population as of 2013 (using a Google search), and whether there was an academic medical center in that city (based on a Google search for “academic medical center” and the city name). City populations were grouped according to the U.S. Office of Management and Budget 2010 standards for delineation.
Factor analysis of interaction items
Twenty-four dichotomous “yes” or “no” items described specific types of physician interactions with DAOs, ranging from visiting a DAO’s website to serving on a DAO’s advisory board. To determine whether these interactions grouped into any natural structure, we conducted an exploratory factor analysis using oblique rotation. Three-, four-, and five-factor models were evaluated.
Five of the 24 items were eliminated from our analysis due to a combination of concerns about conceptual clarity and their failure to load onto a single discrete factor. “Founded or co-founded a DAO” was eliminated because too few physicians had engaged in the activity to fit into a reliable factor structure. “Connected with a DAO using social media” and “Participated in a DAO-sponsored webinar” were eliminated due to concerns about introducing a potential age bias associated with the online nature of these activities. “Received CME or CEU credits through a DAO-sponsored activity” was eliminated since participants may not have been aware of DAO involvement or in-kind contributions to these educational activities. “Written for a DAO newsletter or website” was eliminated because the context of the writing (e.g. whether the content described a research study or provided clinical advice) was felt to be ambiguous. None of these five items which were eliminated loaded clearly onto one distinct factor.
Regression of interaction constructs
Multivariate regression was used to explore associations between demographic variables and each of the interaction constructs identified through exploratory factor analysis. Prior to the regression analysis, independent variables were selected based on hypothesized associations with the constructs. Gender, age, years as a pediatric neurologist, number of pediatric patients per week, percent time for clinical responsibilities, percent time for research responsibilities, academic appointment at a medical school, region of country, academic medical center in city, and population of city were all selected for analysis. Number of activities in which physicians participated was treated as a continuous variable (linear regression), or was dichotomized (logistic regression), and models were fit using maximum likelihood parameter estimates. We considered p < 0.05 to be the threshold for significance and tests were two-sided. All analyses were conducted in SAS v9.4.
RESULTS
We received 251 out of 500 surveys, resulting in a response rate of 50.2%. Twenty-one surveys were excluded from analysis because participants responded that they did not see patients for at least four hours per week or were not board certified. We conducted analysis on 230 completed surveys.
Characteristics of respondents and their medical practices are described in Table 1. Our sample included a diverse group of physicians from all over the country. Participants had an average of over 20 years of experience in pediatric neurology and spent the majority of their time on clinical responsibilities.
Table 1. Individual and practice characteristics of 230 pediatric neurologists.
| Individual Characteristics | N (%) |
|---|---|
| Female | 94 (40.9) |
| Hispanic or Latino descent (n=227) | 12 (5.3) |
| Race (n=224) | |
| White | 163 (73.4) |
| Asian | 51 (23.0) |
| Black or African American | 2 (0.9) |
| American Indian or Alaska Native | 1 (0.5) |
| Native Hawaiian or Pacific Islander | 0 (0.0) |
| Other | 7 (3.2) |
| Age (n=224) – Mean (SD), Range | 53.2 (11.1), 34–84 |
| Medical degree | |
| MD | 226 (98.3) |
| DO | 4 (1.7) |
| Academic or other professional degree | |
| PhD | 24 (10.4) |
| MPH | 7 (3.0) |
| Other | 13 (5.7) |
| Hold academic appointment at medical school | 183 (79.6) |
| Practice Characteristics | Mean (SD), Range |
| Years of pediatric neurology practice (n=229) | 22.2 (11.7), 3–57 |
| Average number of patients seen /week (n=228) | 37.5 (25.0), 2–160 |
| Average number of pediatric patients /week (n=229) | 33.5 (22.5), 2–150 |
| Percent time clinical responsibilities | 75.4 (26.2), 10–100 |
| Percent time research responsibilities | 14.5 (22.1), 0–90 |
| Region of country in which practice located (n=226) – N (%) | |
| South | 75 (33.2) |
| Northeast | 56 (24.8) |
| Midwest | 50 (22.1) |
| West | 45 (19.9) |
| Academic medical center in city of practice (n=220) – N (%) | 193 (87.7) |
| Population of city of practice (n=222) – N (%) | |
| <2,500 | 1 (0.5) |
| 2,500 – 9,999 | 6 (2.7) |
| 10,000 – 49,999 | 21 (9.5) |
| 50,000 – 249,999 | 58 (26.1) |
| 250,000 – 2,499,999 | 123 (55.4) |
| ≥ 2,500,000 | 13 (5.9) |
Almost all physicians in this population reported that they had interacted with DAOs in some way, with 219 (95.2%) reporting that they had participated in at least 1 of the 24 activities examined. The 24 items describing types of physician interactions with DAOs are shown in Table 2. Frequency of participation in individual activities ranged from less than 2% to over 90% of respondents.
Table 2. Frequencies and percentages of pediatric neurologists reporting interactions with DAOs (n = 230).
| N (%) | |
|---|---|
| In the last 5 years, have you suggested that patients or their parents look into a DAO? | 202 (90.6) |
| In the last 5 years, have you discussed a DAO with any of your patients or their parents? | 199 (89.6) |
| In the last 5 years, have you given any patients or their parents educational material from a DAO? | 183 (82.8) |
| In the last 12 months, have you received a DAO’s newsletter in the mail or by email? | 177 (77.6) |
| In the last 12 months, have you visited a DAO’s website? | 170 (74.6) |
| In the last 5 years, have you had information from a DAO available in your office for patients or their parents? | 155 (69.8) |
| In the last 5 years, have you attended a DAO-sponsored meeting or conference? | 108 (48.4) |
| Have you ever served on a DAO medical or scientific advisory board? | 77 (33.5) |
| In the last 5 years, have you attended a DAO support group? | 75 (33.6) |
| In the last 5 years, have you delivered a talk at a DAO event? | 73 (32.7) |
| In the last 5 years, have you received CME or CEU credits through a DAO-sponsored activity?* | 66 (29.9) |
| In the last 5 years, have you consulted for a DAO? | 65 (28.9) |
| In the last 5 years, have you collaborated with a DAO to recruit research participants? | 42 (18.8) |
| In the last 5 years, have you participated in a DAO-sponsored online webinar?* | 36 (16.2) |
| In the last 5 years, have you provided scientific or clinical expertise to a DAO for a research study? | 34 (15.2) |
| In the last 5 years, have you received research funding from a DAO? | 33 (14.9) |
| In the last 12 months, have you connected with a DAO using social media (such as Facebook, Twitter, or blogs)* | 32 (14.2) |
| In the last 5 years, have you written for a DAO newsletter or website?* | 31 (13.9) |
| In the last 5 years, have you collaborated with a DAO on the design of a research study? | 22 (9.9) |
| In the last 5 years, have you reviewed a research grant for a DAO? | 22 (9.9) |
| In the last 5 years, have you co-authored a journal article with someone from a DAO? | 20 (9.0) |
| In the last 5 years, have you co-presented a paper or poster with someone from a DAO? | 15 (6.7) |
| In the last 5 years, have you received a training grant or fellowship support from a DAO? | 9 (4.1) |
| Have you founded or co-founded a DAO?* | 4 (1.7) |
deleted from subsequent factor analysis
Factor analysis of these items produced a four-factor solution (Table 3). All items have adequate internal loadings (>0.30) and the individual factors have high internal consistency (alphas ~0.80). The four factors are largely discrete, with very little cross-loading of items. Just two items (“Received DAO newsletter” and “Collaborated to recruit research participants”) have moderate cross-loadings on two or more factors. These items were assigned to group with their current factors due to slightly higher loading on that factor and a better conceptual fit with other items comprising the factor.
Table 3. Factor analysis of pediatric neurologist interactions with DAOs.
These items segregated into four factors each corresponding to a distinct type of physician-DAO interaction. The exact text of each item is reported in Table 2.
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
|---|---|---|---|---|
| Discussed a DAO with patients/parents | 0.909 | −0.119 | 0.208 | −0.157 |
| Suggested that patients/parents look into a DAO | 0.862 | −0.099 | 0.167 | −0.080 |
| Given patients/parents educational material from a DAO | 0.797 | 0.129 | −0.208 | 0.151 |
| Had information from a DAO available in office | 0.496 | 0.194 | −0.262 | 0.176 |
| Received a DAO’s newsletter | 0.364 | 0.289 | −0.071 | 0.053 |
| Visited a DAO’s website | 0.361 | 0.210 | 0.004 | 0.063 |
| Attended a DAO support group | 0.096 | 0.708 | −0.025 | −0.062 |
| Delivered a talk at a DAO event | 0.063 | 0.663 | 0.170 | −0.104 |
| Served on a DAO advisory board | −0.010 | 0.640 | 0.052 | −0.031 |
| Attended a DAO-sponsored meeting or conference | 0.165 | 0.604 | −0.016 | −0.021 |
| Consulted for a DAO | −0.047 | 0.563 | 0.214 | −0.021 |
| Provided expertise to a DAO for a research study | −0.069 | 0.318 | 0.644 | −0.011 |
| Received research funding from a DAO | 0.003 | −0.027 | 0.598 | 0.074 |
| Collaborated with a DAO on research study design | 0.002 | 0.086 | 0.576 | 0.157 |
| Received a training grant/fellowship support from a DAO | 0.024 | −0.054 | 0.456 | 0.032 |
| Reviewed a research grant for a DAO | −0.082 | 0.210 | 0.438 | 0.055 |
| Collaborated with a DAO to recruit research participants | 0.051 | 0.327 | 0.351 | 0.151 |
| Co-presented a paper/poster with a DAO | 0.038 | −0.091 | 0.184 | 0.768 |
| Co-authored a journal article with a DAO | 0.032 | −0.058 | 0.166 | 0.718 |
| Cronbach’s alpha for each factor | 0.797 | 0.809 | 0.800 | 0.795 |
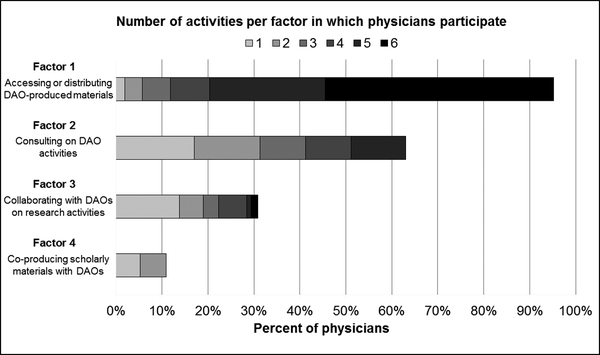
The four factors identified reflect distinct types of physician interactions with DAOs: accessing or distributing DAO-produced materials (Factor 1), consulting on DAO activities (Factor 2), collaborating with DAOs on research activities (Factor 3), and co-producing scholarly materials with DAOs (Factor 4). As illustrated in Figure 1, accessing or sharing information from DAOs (Factor 1) was frequent among physicians. Almost all physicians (95.4%) reported that they had interacted with DAOs in this way, with almost half (49.3%) having participated in all six activities. More active forms of collaboration among physicians and DAOs (Factors 2–4) were much less common. While over half of physicians surveyed (63.1%) participated in consultative activities, only 31.3% conducted research with DAOs and just 10.6% had co-authored papers and presentations with DAOs.
Figure 1. Percent of pediatric neurologists interacting with DAOs by factor.
Bars reflect the percent of physicians in our sample (n=230) who reported interactions within each factor. The specific activities comprising each factor are reported in Table 3.
Multivariate regression showed very few associations of note. Participation in Factor 1 activities was associated with being slightly younger. Physicians use or share DAO information through one fewer activity for each 20 years of age (coefficient β=−0.05, p=0.047). Participation in Factor 3 activities was associated with spending more time on research responsibilities. Physicians engage in one more research activity with DAOs for each 33.33% of time dedicated to research (coefficient β=0.03, p<0.0001). No other statistically significant associations were identified.
DISCUSSION
To assess the full array of ethical and professional implications of physician interactions with DAOs, we first must understand the forms and extent of those interactions. We believe our study is among the first to seek to characterize the full array of direct and indirect interactions that physicians have with DAOs.
Our data suggest that interactions between physicians and DAOs are quite common. We found that nearly all physicians in our sample had interacted directly with DAOs, and that most had engaged with DAOs in several ways. Interactions with DAOs were frequent and diverse, ranging from low-effort activities like visiting a DAO website to more extended forms of engagement like co-authoring journal articles. Among pediatric neurologists who responded, participation in low-effort activities was nearly universal. Engaging with DAOs in more time-consuming ways was less common, however, perhaps because such activities imply greater levels of personal alignment with DAO goals and mission.
The breadth of physician-DAO interactions we identified suggests that DAOs are expanding into clinical settings in many ways, raising potential ethical and professional issues. The influence of DAOs may challenge the typical doctor-patient relationship by encouraging patients to play a more active role in their care. While DAOs may help patients to learn more about their conditions and feel more confident in medical discussions, physicians may be cautious of relying on clinical information provided by DAOs since it could be of varying quality, as has been found in other industry-funded medical websites (Read and Cain 2013). However, many physicians may embrace relationships with DAOs, resulting in partnerships to educate patients in the clinic and online. These collaborations may reframe the doctor-patient relationship as more of a partnership, much like similar alliances between scientists and DAOs have redefined the researcher-subject relationship (Koay and Sharp 2013, Wood et al. 2013).
Furthermore, physician collaborations with DAOs may increase patients’ influence on their care, which may lead to better patient experience. Some scholars have suggested that forging close relationships with researchers can give DAOs increased influence over the research process and goals (Panofsky 2011). While many physicians and researchers recognize benefits of patient input on research and care (Deal et al. 2017; Smith et al. 2015), some may be wary of DAOs as the intermediary for patients’ goals. Many concerns have been expressed in the ethics literature and the popular media regarding potential conflicts of interest associated with DAOs receiving industry funding (Huehnergarth 2016; Klein 2017; Abola and Prasad 2016; McCoy et al. 2017; Rose et al. 2017). These conflicts of interest cast doubt on whether the actions of some DAOs are solely reflective of their patients’ interests, so close collaborations between physicians and DAOs may not be successful in increasing patient input. These considerations highlight the importance of examining the multiple ways in which physicians interact with DAOs.
Many in the medical field have called for more physician involvement in health advocacy and have encouraged doctors to engage patient communities beyond individual patient care (Gruen, Pearson, and Brennan 2004). Our survey, while small, suggests that pediatric neurologists may be engaging patient communities through DAOs and supporting health advocacy activities through the dissemination of DAO content.
We found very few demographic associations with DAO engagement, which suggests that DAOs may not be targeting specific types of physicians based on demographic factors or characteristics of their clinical practices. The association between research responsibilities and DAO research collaborations that we observed is intuitive since clinicians who spend more time on research are generally more likely to form research collaborations. Increased utilization and sharing of DAO materials among younger physicians could be attributed to a greater familiarity with, and reliance on, information found on the Internet (Martin 2004). While DAOs may be more prevalent in certain areas of the country or collaborate frequently with academic medical centers (Gallin et al. 2013), physician engagement with DAOs does not seem to be associated with these factors. On the contrary, interacting with DAOs may be nearly universal among physicians in this specialty. It should be noted, however, that our sample may have been too small to detect demographic associations, and some differences between physician subgroups may truly exist.
This study is the first to describe the diverse types of physician interactions with DAOs. We identified four distinct types of interactions, which may provide a framework for characterizing modes of engagement as DAOs seek to influence the delivery of medical care. These types of interactions are not specific to any particular clinical specialty, and therefore could be adaptable to other contexts. Additionally, the items are neutral with respect to the value and directionality of these interactions. The activities are not framed as positive or negative, and most items do not clarify whether it was the physician or the DAO who initiated the interaction. By allowing for either party to serve as the initiator, we intended to capture as many interactions as possible. The diversity of activity types assessed, combined with the distribution of participation levels seen across individual activities, suggests that this list of physician interactions with DAOs could be a good candidate for a global measure of physicians’ engagement with DAOs.
These items, however, would likely need more modification and testing in order to be used as a consistent scale across disciplines. Further development would benefit from a theoretical model or evaluations of content validity. As noted in the Methods, some of the items describing physician-DAO interactions may be interpreted in multiple ways. We sought to use terms that were sufficiently open-ended to capture as many interactions as possible, but ambiguity could be problematic for responders and analysis. Cognitive interviews with physicians would help clarify and refine the item set.
Another limitation of the items is their different time frames (within the last 12 months, 5 years, or ever). While these time frames were chosen intentionally to capture the prevalence of each activity type, it does make it difficult to directly compare across items. Additionally, the factors themselves vary in number of items, so direct comparisons across factors should not be over-interpreted. In addition, these items do not capture the frequency of physicians’ interactions with DAOs. A physician who consults for a DAO on a regular basis and is deeply committed to the group’s mission cannot be distinguished from a physician who consulted for a DAO on a single occasion and decided never to do it again. The items are only used to measure the frequency of specific interactions with DAOs, and do not assess a physician’s dedication to or endorsement of a DAO.
Finally, these items were only administered in a small survey, with a response rate slightly greater than 50%. This response rate is not atypical for physicians (Cho, Johnson, and Vangeest 2013), but does introduce potential response bias. We did not collect data on non-responders to evaluate potential bias. The small respondent pool and lack of cognitive testing should also add caution to our results. Additionally, the survey only targeted members of one physician specialty. We intentionally surveyed pediatric neurologists, who are likely to interact with DAOs frequently. Frequency and types of interactions may vary by physician subspecialty and the types of DAOs associated with the field. Since comparable levels of interactions with DAOs cannot be expected in all physician subspecialties, testing these items in a larger national sample of healthcare providers would be beneficial.
This multifactor item set provides one way to describe physician interactions with DAOs, but it should not be used in isolation. Other tools will be necessary to examine the intensity and directionality of these interactions. Future research should aim to develop such tools and more thoroughly assess the nature, benefits, and potential harms of physician-DAO interactions.
CONCLUSION
Our data indicate that physicians are interacting with DAOs in more frequent and diverse ways than has been reported. As the scope of DAOs expands to include activities that may more directly impact patient care, it is critical to evaluate the ethical implications of physician-DAO relationships. We identified four distinct types of physician-DAO interactions, which may provide a useful framework for bioethicists to characterize the nature and extent of physician interactions with advocacy organizations.
ACKNOWLEDGMENTS:
The authors thank Amy Jo Marcano, David Landy, and Mary Ellen Colten for their advice on the construction of our sample and for their input on early versions of the survey. The authors also thank Christina Nyquist for her assistance with data cleaning.
FUNDING: This project was supported by the National Human Genome Research Institute under grant number P50 HG003390 (Center for Genetic Research Ethics and Law) and the Center for Individualized Medicine at Mayo Clinic.
Footnotes
CONFLICTS OF INTEREST: None disclosed.
ETHICAL APPROVAL: This study was approved by the institutional review boards at Mayo Clinic.
Contributor Information
Carol Cosenza, Center for Survey Research, University of Massachusetts Boston, 100 Morrissey Blvd, Boston, MA 02125.
Richard R. Sharp, Biomedical Ethics Research Program, Center for Individualized Medicine, Mayo Clinic, 200 First St SW, Rochester, MN 55905.
REFERENCES
- Abola Matthew V., and Prasad Vinay. 2016. “Industry Funding of Cancer Patient Advocacy Organizations.” Mayo Clinic Proceedings 91 (11):1668–1670. doi: 10.1016/j.mayocp.2016.08.015. [DOI] [PubMed] [Google Scholar]
- Aymé Ségolène, Kole Anna, and Groft Stephen. 2008. “Empowerment of patients: lessons from the rare diseases community.” The Lancet 371 (9629):2048–2051. doi: 10.1016/S0140-6736(08)60875-2. [DOI] [PubMed] [Google Scholar]
- Boon Wouter, and Broekgaarden Ria. 2010. “The role of patient advocacy organisations in neuromuscular disease R&D – The case of the Dutch neuromuscular disease association VSN.” Neuromuscular Disorders 20 (2):148–151. doi: 10.1016/j.nmd.2009.10.012. [DOI] [PubMed] [Google Scholar]
- Cho YI, Johnson TP, and Vangeest JB. 2013. “Enhancing surveys of health care professionals: a meta-analysis of techniques to improve response.” Eval Health Prof 36 (3):382–407. doi: 10.1177/0163278713496425. [DOI] [PubMed] [Google Scholar]
- Deal Linda S, Goldsmith Jonathan C, Martin Susan, Barbier Ann J, Roberds Steven L, and Schubert David H. 2017. “Patient Voice in Rare Disease Drug Development and Endpoints.” Therapeutic Innovation & Regulatory Science 51 (2):257–263. [DOI] [PubMed] [Google Scholar]
- Earnest Mark A., Wong Shale L., and Federico Steven G.. 2010. “Perspective: Physician Advocacy: What Is It and How Do We Do It?” Academic Medicine 85 (1):63–67. doi: 10.1097/ACM.0b013e3181c40d40. [DOI] [PubMed] [Google Scholar]
- Gallin EK, Bond E, Califf RM, Crowley WF, Davis P, and Galbraith R. 2013. “Forging stronger partnerships between academic health centers and patient-driven organizations.” Acad Med 88. doi: 10.1097/ACM.0b013e31829ed2a7. [DOI] [PubMed] [Google Scholar]
- Gruen RL, Campbell EG, and Blumenthal D. 2006. “Public roles of us physicians: Community participation, political involvement, and collective advocacy.” JAMA 296 (20):2467–2475. doi: 10.1001/jama.296.20.2467. [DOI] [PubMed] [Google Scholar]
- Gruen RL, Pearson SD, and Brennan TA. 2004. “Physician-citizens—public roles and professional obligations.” JAMA 291 (1):94–98. doi: 10.1001/jama.291.1.94. [DOI] [PubMed] [Google Scholar]
- Hagan TH, Rosenzweig M, Zorn K, van Londen J, and Donovan H. 2017. “Perspectives on Self-Advocacy: Comparing Perceived Uses, Benefits, and Drawbacks Among Survivors and Providers.” Oncol Nurs Forum 44 (1):52–59. doi: 10.1188/17.ONF.52-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JG. 2013. “The role of patient advocacy/parent support groups.” SAMJ: South African Medical Journal 103:1020–1022. [DOI] [PubMed] [Google Scholar]
- Huehnergarth Nancy Fink. 2016. Has EpiPen Price Gouger Mylan Silenced Allergy Advocates? Forbes. [Google Scholar]
- Institute of Medicine. 2010. “Advocacy Group Approaches to Accelerating Research and Product Development: Illustrative Examples” In Rare Diseases and Orphan Products: Accelerating Research and Development, edited by Field Marilyn J. and Boat Thomas F., 371–386. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Keller Ann C., and Packel Laura. 2014. “Going for the Cure: Patient Interest Groups and Health Advocacy in the United States.” Journal of Health Politics, Policy & Law 39 (2):331–367. doi: 10.1215/03616878-2416238. [DOI] [PubMed] [Google Scholar]
- Klein Marnie. 2017. Masked Marketing: Pharmaceutical Company Funding of ADHD Patient Advocacy Groups. Bioethics Forum. [Google Scholar]
- Koay Pei P., and Sharp Richard R.. 2013. “The Role of Patient Advocacy Organizations in Shaping Genomic Science.” Annual Review of Genomics and Human Genetics 14 (1):579–595. doi: 10.1146/annurev-genom-091212-153525. [DOI] [PubMed] [Google Scholar]
- Landy David C., Brinich Margaret A., Mary Ellen Colten Elizabeth J. Horn, Terry Sharon F., and Sharp Richard R.. 2012. “How disease advocacy organizations participate in clinical research: a survey of genetic organizations.” Genet Med 14 (2):223–228. [DOI] [PubMed] [Google Scholar]
- Martin Shelley. 2004. “Younger physicians, specialists use Internet more.” CMAJ : Canadian Medical Association Journal 170 (12):1780–1780. doi: 10.1503/cmaj.1040621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy Matthew S., Carniol Michael, Chockley Katherine, Urwin John W., Emanuel Ezekiel J., and Schmidt Harald. 2017. “Conflicts of Interest for Patient-Advocacy Organizations.” New England Journal of Medicine 376 (9):880–885. doi: 10.1056/NEJMsr1610625. [DOI] [PubMed] [Google Scholar]
- Oberg Charles N. 2003. “Pediatric Advocacy: Yesterday, Today, and Tomorrow.” Pediatrics 112 (2):406–409. [DOI] [PubMed] [Google Scholar]
- Panofsky A 2011. “Generating sociability to drive science: patient advocacy organizations and genetics research.” Soc Stud Sci 41 (1):31–57. doi: 10.1177/0306312710385852. [DOI] [PubMed] [Google Scholar]
- Pauer Frédéric, Litzkendorf Svenja, Jens Göbel Holger Storf, Zeidler Jan, and Johann-Matthias Graf von der Schulenburg. 2017. “Rare Diseases on the Internet: An Assessment of the Quality of Online Information.” Journal of Medical Internet Research 19 (1):e23. doi: 10.2196/jmir.7056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plumridge G, Metcalfe A, Coad J, and Gill P. 2011. “The role of support groups in facilitating families in coping with a genetic condition and in discussion of genetic risk information.” Health Expect 15 (3):255–66. doi: 10.1111/j.1369-7625.2011.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polich Ginger R. 2012. “Rare disease patient groups as clinical researchers.” Drug Discovery Today 17 (3):167–172. doi: 10.1016/j.drudis.2011.09.020. [DOI] [PubMed] [Google Scholar]
- Read J, and Cain A. 2013. “A literature review and meta-analysis of drug company–funded mental health websites.” Acta Psychiatrica Scandinavica 128 (6):422–433. doi: 10.1111/acps.12146. [DOI] [PubMed] [Google Scholar]
- Rose Susannah L, Highland Janelle, Karafa Matthew T, and Steven Joffe. 2017. “Patient advocacy organizations, industry funding, and conflicts of interest.” JAMA internal medicine 177 (3):344–350. [DOI] [PubMed] [Google Scholar]
- Rose Susannah L. 2013. “Patient Advocacy Organizations: Institutional Conflicts of Interest, Trust, and Trustworthiness.” The Journal of Law, Medicine & Ethics 41 (3):680–687. doi: 10.1111/jlme.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp RR, and Landy DC. 2010. “The financing of clinical genetics research by disease advocacy organizations: A review of funding disclosures in biomedical journals.” Am J Med Genet A 152A (12):3051–6. doi: 10.1002/ajmg.a.33767. [DOI] [PubMed] [Google Scholar]
- Smith Sophia K., Selig Wendy, Harker Matthew, Roberts Jamie N., Hesterlee Sharon, Leventhal David, Klein Richard, Patrick-Lake Bray, and Abernethy Amy P.. 2015. “Patient Engagement Practices in Clinical Research among Patient Groups, Industry, and Academia in the United States: A Survey.” PLoS ONE 10 (10):e0140232. doi: 10.1371/journal.pone.0140232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry Sharon F., Terry Patrick F., Rauen Katherine A., Uitto Jouni, and Bercovitch Lionel G.. 2007. “Advocacy groups as research organizations: the PXE International example.” Nat Rev Genet 8 (2):157–164. [DOI] [PubMed] [Google Scholar]
- The Autistic Self Advocacy Network, The Association for Autistic Community, Autism Women’s Network, Association of Programs for Rural Independent Living, Autism National Committee, Asperger’s Association of New England, National Council on Independent Living, National Coalition on Mental Health Recovery, Little People of America, Self-Advocates Becoming Empowered (SABE), Not Dead Yet, Ollibean, TASH, The Thinking Person’s Guide to Autism, Queerability, Michigan Disability Rights Coalition, PACLA, Down Syndrome Uprising, YOUTH POWER!, Education DREAM: Disability Rights, Activism, and Mentoring,, Taishoff Center for Inclusive Higher Education, I Am Norm, We Are Like Your Child, The Unpuzzled Project, Autism Rights Group Highland, and Autism Acceptance Day. 2014. “2014 Joint Letter to the Sponsors of Autism Speaks.” Autistic Self Advocacy Network; https://autisticadvocacy.org/2014/01/2013-joint-letter-to-the-sponsors-of-autism-speaks/. [Google Scholar]
- Wood Jill, Sames Lori, Moore Allison, and Ekins Sean. 2013. “Multifaceted roles of ultra-rare and rare disease patients/parents in drug discovery.” Drug Discovery Today 18 (21):1043–1051. doi: 10.1016/j.drudis.2013.08.006. [DOI] [PubMed] [Google Scholar]