Abstract
Background
Health care workers (HCWs) are essential for the delivery of health care services in conflict areas and in rebuilding health systems post-conflict.
Objective
The aim of this study was to systematically identify and map the published evidence on HCWs in conflict and post-conflict settings. Our ultimate aim is to inform researchers and funders on research gap on this subject and support relevant stakeholders by providing them with a comprehensive resource of evidence about HCWs in conflict and post-conflict settings on a global scale.
Methods
We conducted a systematic mapping of the literature. We included a wide range of study designs, addressing any type of personnel providing health services in either conflict or post-conflict settings. We conducted a descriptive analysis of the general characteristics of the included papers and built two interactive systematic maps organized by country, study design and theme.
Results
Out of 13,863 identified citations, we included a total of 474 studies: 304 on conflict settings, 149 on post-conflict settings, and 21 on both conflict and post-conflict settings. For conflict settings, the most studied counties were Iraq (15%), Syria (15%), Israel (10%), and the State of Palestine (9%). The most common types of publication were opinion pieces in conflict settings (39%), and primary studies (33%) in post-conflict settings. In addition, most of the first and corresponding authors were affiliated with countries different from the country focus of the paper. Violence against health workers was the most tackled theme of papers reporting on conflict settings, while workforce performance was the most addressed theme by papers reporting on post-conflict settings. The majority of papers in both conflict and post-conflict settings did not report funding sources (81% and 53%) or conflicts of interest of authors (73% and 62%), and around half of primary studies did not report on ethical approvals (45% and 41%).
Conclusions
This systematic mapping provides a comprehensive database of evidence about HCWs in conflict and post-conflict settings on a global scale that is often needed to inform policies and strategies on effective workforce planning and management and in reducing emigration. It can also be used to identify evidence for policy-relevant questions, knowledge gaps to direct future primary research, and knowledge clusters.
Introduction
Health care workers (HCWs) are essential for the delivery of health care services in conflict areas and in rebuilding health systems post-conflict. However, HCWs in conflict areas around the world are being threatened, detained, and killed. For instance, in Syria, Physicians for Humans Rights has reported that, since the start of the conflict till December 2017, 847 medical personnel have been killed [1]. In Afghanistan, around 92 attacks against health facilities and health workers killed 14 health workers and four caretakers in the period extending from March 1, 2015 till February 10, 2016 [2].
Direct attacks and insecurity have led to the exodus of HCWs from conflict areas. In Syria, 50% of the health workers and 95% of physicians living in Aleppo have left the country since 2011. In Iraq, almost half of the health professionals have emigrated since 2014 [2]. In Nigeria, almost all health workers have escaped areas controlled by Boko Haram since 2012, leading to the closure of 450 health facilities [2].
The resulting shortage of HCWs has devastating effects on the delivery of, and access to health care not only during conflicts but also in the aftermath of war. The post-conflict settings are characterized by poor health outcomes due to limited availability of HCWs and disruption of health systems [3, 4]. Rebuilding the health workforce is critical to address health needs and strengthen health systems. Furthermore, post-conflict settings present a window of opportunity to develop responsive and evidence-informed strategies and policies to address defects in the supply, distribution and performance of the health workforce [4, 5].
In 2012, the World Health Organization (WHO) passed a resolution that calls on the WHO Director General for leadership in documenting evidence of attacks against health workers, facilities, and patients in situations of armed conflict [6]. A scoping review on HCWs in Syria and other “Arab Spring” countries showed scarcity of research evidence on HCWs in the setting of the “Arab Spring” [7]. While that review revealed a number of themes of interest (e.g., violence against health care workers, education, practicing in conflict setting, migration), it focused on only one region and did not address post-conflict settings. Therefore, the objective of this study was to systematically identify and map the published evidence on HCWs in both conflict and post-conflict settings. Our ultimate aim is to inform researchers and funders on research gap on this subject and support relevant stakeholders by providing them with a comprehensive resource of evidence about HCWs in conflict and post-conflict settings on a global scale.
Methods
Study design
This systematic mapping was based on a protocol registered with Open Science Framework [8]. We followed standard methodology for screening, data extraction and coding, data analysis, and visualizing the findings in systematic mapping. Contrary to systematic reviews, systematic mapping does not aim to answer a specific question but instead “collates, describes and catalogues available evidence (e.g. primary, secondary, quantitative or qualitative) relating to a topic of interest” [9]. In accordance with the definition of systematic maps, this study is a “systematic visual presentation of the availability of relevant evidence,” but not the content of the evidence [10] for the topic of health care workers in conflict and post-conflict settings. The studies included in a systematic map can be used to identify evidence for policy-relevant questions, knowledge gaps to direct future primary research, and knowledge clusters. Knowledge clusters are sub-sets of evidence that may be suitable for secondary research, for example systematic review.
Eligibility criteria
Population of interest
Our population of interest consisted of any personnel providing health services such as: midwives, nurses, paramedics, pharmacists, physicians, laboratory technicians, community health workers as well as medical students and trainees. We excluded military HCWs, because we aimed to focus on the delivery of health care primarily to civilians.
Setting of interest
We included both conflict and post-conflict settings. We considered both conflicts between and within states [11]. We focused on contemporary conflicts that started after or were ongoing in the 1990s. We defined conflicts as international armed conflicts between two or more states or non-international armed conflicts between non-governmental armed groups or with governmental forces [11]. Post-conflict settings are considered as a stage of recovery of the state from a conflict or crisis and a stage of rebuilding and reconstruction starting from emergency and stabilization followed by transition and recovery, and peace and development [5, 12, 13]. We referred to the description used by the authors when specifying whether the setting of the study was conflict or post-conflict.
Study design
We included all types of study designs, including news, editorials, commentaries, opinion pieces, technical reports, primary studies, narrative reviews, and systematic reviews. We excluded conference abstracts. We restricted our eligibility criteria to papers published after the year 2000 to better reflect the current challenges facing health systems and the new aspects of contemporary conflicts.
Literature search
We searched the following electronic databases: Medline (Ovid), PubMed, EMBASE (Ovid), the Cochrane Central Register of Controlled Trials (CENTRAL), Cumulative Index of Nursing and Allied Health Literature CINAHL (EBSCOT) on July 2017. We also searched the ReBUILD Consortium Resources webpage and the Human Resources for Health (HRH) Global Resource Center.
We used both index terms and free text words for the two following concepts: (1) health care workers and (2) conflict and post-conflict settings. The search terms and Medical Subject Headings (MeSH) terms for each database were developed with the guidance of an information specialist. We did not limit the search to specific languages. S1 File provides the search strategies for the different databases.
Selection process
Title and abstract screening
Teams of two reviewers used the above eligibility criteria to screen titles and abstracts of identified citations in duplicate and independently for potential eligibility. We retrieved the full texts for citations judged as potentially eligible by at least one of the two reviewers.
Full-text screening
Teams of two reviewers used the above eligibility criteria to screen the full texts in duplicate and independently for eligibility. The teams of two reviewers resolved disagreement by discussion or with the help of a third reviewer. We used standardized and pilot-tested screening forms. We conducted calibration exercises to ensure the validity of the selection process.
Data extraction and coding
Two reviewers extracted data using standardized and pilot tested forms. The reviewers resolved any disagreement by discussion and when needed with the help of a third reviewer. We conducted calibration exercises to ensure the validity of the data abstraction process.
We extracted from each paper the following information:
Citation;
Year of publication;
Countr(ies) subject of the paper;
Type of publication (e.g., news, editorial, correspondence, opinion pieces, primary study, narrative review, systematic review, case study, technical report)
Language of publication;
- Authors’ information:
- ○ Total number of authors;
- ○ Number of authors from the countr(ies) subject of the paper;
- ○ Country of affiliation of the first author;
- ○ Country of affiliation of the contact author;
Characteristics of the journal of publication (name and impact factor);
Setting (conflict or post-conflict);
Theme(s) of the study for conflict settings: we adopted the themes from a previous scoping review on health care workers in the setting of Arab Spring [7]: violence against health care workers, education, practicing in conflict setting, migration, and other (S2 File);
Theme(s) of the study for post-conflict settings: we adopted the theme(s) from a previous review on human resource management in post-conflict health systems [5]: workforce supply, workforce distribution, workforce performance, and other (S2 File);
Reporting of funding of the study;
Reporting of conflict of interest of authors;
Ethical approval of the study.
For the themes, data was coded as ‘other’ if it did not address any of the existing themes, or if it covered an emerging theme and an existing one. Using an iterative process of review and refinement, data coded as ‘other’ was revisited, collated and new themes were generated.
Critical appraisal
We did not appraise the quality of included studies since our review is consistent with standard systematic mapping methodology [9].
Data analysis
We conducted a descriptive analysis of the general characteristics of the included papers using frequencies. We also used the results of this review to build two interactive and visual systematic evidence maps on (1) HCWs in conflict settings and (2) HCWs in post-conflict settings. We represented the evidence maps by country, type of publication and themes. We have also provided direct links to the included studies in the maps.
Results
Study selection
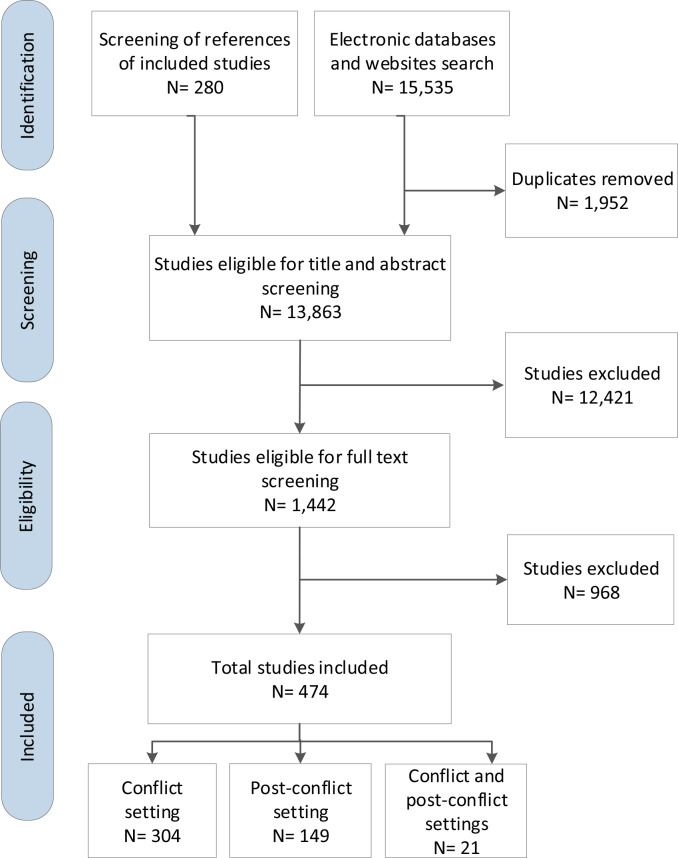
Fig 1 summarizes the study selection process. Out of 13,863 identified unique citations, we included a total of 474 studies [4, 14–470]: 304 on conflict settings, 149 on post-conflict settings, and 21 on both conflict and post-conflict settings. We excluded 968 papers for the following reasons: not study design of interest (n = 63); not setting of interest (n = 324); not population of interest (n = 538); and not timeframe of interest (e.g. ceasefire was called on before 1990) (n = 43). We present below our findings on the characteristics of the included papers, journals, authors, funding, conflicts of interest, and ethics reporting. We also report on the two generated systematic maps.
Fig 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) study flow diagram for selection.
Characteristics of the included papers
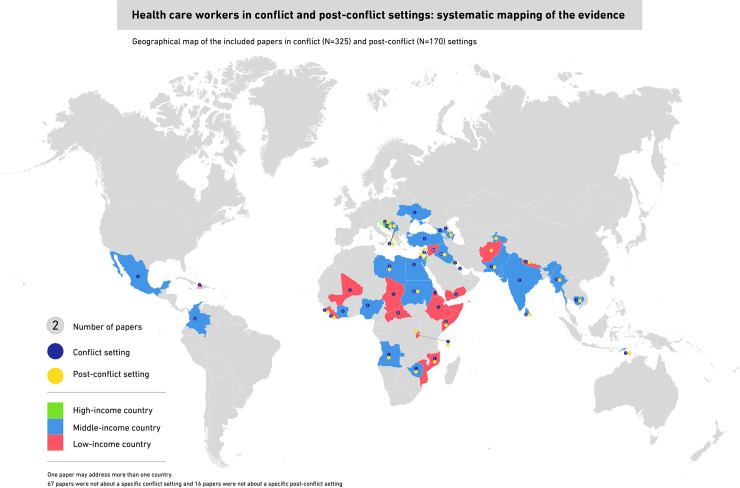
Fig 2 presents a geographical map of the countries focus of the included papers (S3 File). A description of the included studies is also presented in S4 File. The majority of the articles included in this systematic mapping were about low-income countries. For conflict settings (N = 325), 79% of the included papers addressed specific conflicts related to 47 countries. The most studied counties were Iraq (15%), Syria (15%), Israel (10%), and the State of Palestine (9%). For post-conflict settings (N = 170), 91% of the included papers addressed specific settings related to 32 countries. Sierra Leone (14%) was the most studied country followed by Uganda (11%) and Afghanistan (9%). The majority of papers on conflict and post-conflict were published in English language (98% and 100% respectively).
Fig 2. Geographical map of the included papers in conflict (N = 325) and post-conflict (N = 170) settings.
Table 1 represents the themes focus of the papers on health care workers in conflict (N = 325) and post-conflict (N = 170) settings. More than one theme was reported in 33% of the papers on HCWs in conflict settings and in 52% of the papers on HCWs in post-conflict settings. In addition to the themes about HCWs in conflict settings reported in Bou-Karroum et al. (2018) [7], three additional themes emerged in this review, and those were the role of HCWs in peace promotion or protecting health care, mental health of HCWs, and medical ethics. Most of the included papers on conflict settings addressed the theme of violence against health workers (41%), followed by health or medical practice (34%) and education (21%). For post-conflict settings, besides the themes adopted from Roome et al. (2014) [5], an emerging theme was the mental health of HCWs. The majority of the included papers on post-conflict settings addressed the workforce performance theme (77%) followed by workforce supply (58%).
Table 1. Topics focus of the papers on health care workers in conflict (N = 325) and post-conflict (N = 170) settings.
| Topics of the papers* | n (%) |
|---|---|
| Conflict setting (N = 325) | |
| • Violence against health care workers | 133 (41) |
| • Health or medical practice | 109 (34) |
| • Education | 67 (21) |
| • Role in peace promotion or protecting health care | 48 (15) |
| • Mental health | 42 (13) |
| • Migration | 37 (11) |
| • Medical ethics | 16 (5) |
| Post-conflict setting (N = 170) | |
| • Workforce performance | 131 (77) |
| • Workforce supply | 98 (58) |
| • Workforce distribution | 40 (24) |
| • Retention | 22 (13) |
| • Mental health | 8 (5) |
*One paper may address more than one topic.
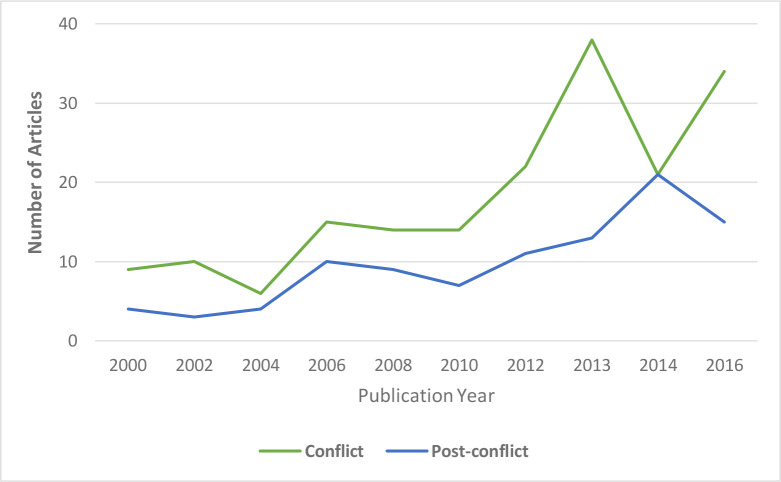
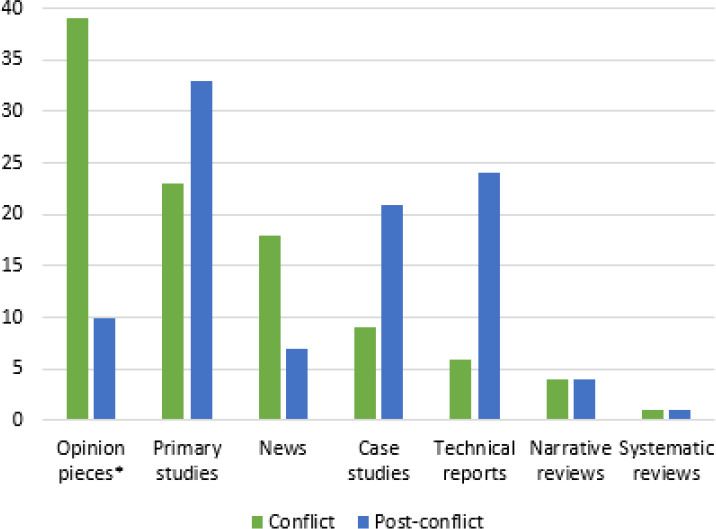
Fig 3 shows the annual production rate of the included papers. The year for the peak number of publications was 2013 for conflict settings and 2014 for post-conflict settings. Fig 4 shows the types of publication of the included papers. Opinion pieces represented the most common type of publication (39%) in conflict settings, followed by primary studies (23%) and news (18%). Primary studies were the most common type of publication (33%) in post-conflict settings followed by technical reports (24%) and case studies (21%).
Fig 3. Publication year of articles of the papers included in the systematic maps in conflict (N = 325) and post-conflict settings*.
Fig 4. Types of publication* of the included papers on health care workers in conflict (N = 325) and post-conflict (N = 170) settings.
Characteristics of the journals
For conflict settings (N = 325), the included papers were published across 134 journals. The journals that published the highest proportions of included studies were the Lancet (15%), BMJ (7%), and CMAJ (5%). Out of the 134 journals, 90 journals (67%) had 2017 impact factors. 230 of the 325 papers were published in these 90 journals and had a median impact factor of 4.74 (IQR = 1.74–27.94).
For post-conflict settings (N = 170), the included papers were published across 79 journals. The journals that published the highest number of included studies were the Lancet (6%), Conflict and Health (5%), and Health Policy and Planning (5%). Out of the 79 journals, 51 journals (65%) had 2017 impact factors. 92 of the 170 papers were published in these 51 journals and had a median impact factor of 2.42 (IQR = 1.61–3.31).
Characteristics of the authors
Table 2 summarizes the characteristics of the authors of the included papers. For conflict settings, 69% of the included papers reported affiliations of authors and addressed specific conflict(s). Out of these, 40% had at least 1 author affiliated with the country focus of the paper. The median percentage of authors affiliated with the country focus of the paper was null (0%) (IQR = 0–75). In addition, most of the first and corresponding authors were affiliated with countries different from the country focus of the paper (68% and 70% respectively), mainly the United States of America (42% and 39% respectively) followed by the United Kingdom (21% and 24% respectively).
Table 2. Characteristics of authors of the included papers in conflict (N = 325) and post-conflict (N = 170) settings.
| Any/all authors | Conflict (N = 325) | Post-conflict (N = 170) |
|---|---|---|
| n (%) | ||
| Papers with named authors | 302 (93) | 161 (95) |
| Papers reporting affiliations of authors | 279 (86) | 141 (83) |
| N = 224* (69) | N = 128* (75) | |
| Papers with at least 1 author affiliated with country focus of paper | 90 (40) | 68 (53) |
| % authors affiliated with country focus of paper (median [IQR]) | 0 (0–75) | 20 (0–67) |
| First author | N = 224 | N = 128 |
| Country focus of paper | 68 (30) | 42 (33) |
| Different country | 151 (68) | 84 (66) |
| - United States of America | 63 (42) | 2 (32) |
| - United Kingdom | 31 (21) | 31 (37) |
| - European countries other than UK | 20 (13) | 7 (8) |
| - Canada | 15 (10) | 7 (8) |
| - Other | 22 (14) | 12 (15) |
| Independent | 5 (2) | 2 (1) |
| Corresponding author | N = 213§ | N = 125§§ |
| Country focus of paper | 60 (28) | 29 (23) |
| Different country | 148 (70) | 94 (75) |
| - United States of America | 58 (39) | 29 (31) |
| - United Kingdom | 35 (24) | 38 (40) |
| - European countries other than UK | 20 (14) | 8 (9) |
| - Canada | 14 (9) | 7 (7) |
| - Other | 21 (14) | 12 (13) |
| Independent | 5 (2) | 2 (2) |
Abbreviation: IQR, interquartile range
* This is the number of papers reporting affiliations of authors and addressing a specific setting.
§ The corresponding author was unclear in 11 papers.
§§ The corresponding author was unclear in 3 papers.
For post-conflict settings, 75% of the included papers reported affiliations of authors and addressed specific conflict(s). Out of these, about half (53%) had at least 1 author affiliated with the country focus of the paper. The median percentage of authors affiliated with the country focus of the paper was 20% (IQR = 0–67). Similar to conflict settings, most of the first and corresponding authors were affiliated with countries different from the country focus of the paper (66% and 75% respectively), mainly the United Kingdom (37% and 40% respectively) followed by the United States of America (32 and 31% respectively).
Funding, conflicts of interest and ethics reporting characteristics
Table 3 shows the funding, conflicts of interest, and ethics reporting characteristics of the included papers. For conflict settings, most of the included papers did not report funding sources (81%) or statements of conflicts of interest of authors (73%). Out of the included primary studies, about half (55%) reported ethical approval to conduct the studies. For post-conflict settings, about half of the included papers did not report funding sources (53%) and 62% did not report on the conflicts of interest of authors. Out of the included primary studies, 59% reported ethical approval.
Table 3. Funding, conflicts of interest and ethics reporting characteristics of the included papers in conflict (N = 325) and post-conflict (N = 170) settings.
| Conflict (N = 325) | Post-conflict (N = 170) | |
| Funding sources | n (%) | |
| Not reported | 263 (81) | 90 (53) |
| Reported as funded | 50 (15) | 75 (44) |
| Reported as not funded | 12 (4) | 5 (3) |
| Conflicts of interest | ||
| Not reported | 238 (73) | 106 (62) |
| Reported | 87 (27) | 64 (38) |
| Ethical approval of primary studies | Conflict (N = 76) | Post-conflict (N = 56) |
| Not reported | 33 (44) | 21 (38) |
| Reported as approved | 42 (55) | 33 (59) |
| Reported as not required | 1 (1) | 2 (3) |
Systematic maps
The two systematic maps, which represent a visual and interactive overview of the evidence on health care workers in conflict and post-conflict settings, can be freely accessed and downloaded using the following links for conflict settings (http://evidencemaphcw.com/gapmap/conflict) and for post-conflict settings (http://evidencemaphcw.com/gapmap/post-conflict). The maps allow data to be filtered and sorted by type of primary studies (experimental, survey, qualitative, mixed-methods, and document analysis). The maps contain links that redirect the user to PubMed or other databases, to access the title and abstract of included papers, when available.
The systematic map for conflict settings shows that papers on violence and attacks against HCWs were mainly not country specific, about Syria, or about Iraq. The theme of health or medical practice of HCWs was mainly addressed in Iraq and Syria. Education and training of health care workers was the theme mainly addressed in Iraq and Myanmar. Primary studies on HCWs in conflict setting were mainly about Israel and the State of Palestine with a focus on mental health in both countries.
The systematic map for post-conflict settings shows that the theme of workforce performance was mainly about Sierra Leone and Uganda. The papers on workforce supply were mainly not country specific, about Afghanistan, or about Sierra Leone. Primary studies on HCWs in post-conflict setting were mainly about Sierra Leone and Afghanistan with a focus on workforce performance in both countries.
Discussion
This review presents a systematic mapping of the evidence on health care workers in conflict and post-conflict settings. It has uncovered interesting findings relating to the characteristics of the included papers, journals, and authors respectively; as well as the reporting of funding, conflicts of interest, and ethics.
The systematic map for conflict settings shows the scarcity of primary studies conducted in conflict settings with the predominance of news, opinion pieces and commentaries. This is in line with a previous scoping review on health care workers in the setting of Arab Spring that showed the scarcity of research evidence [7]. Similarly, Patel et al. (2017) reported on the lack of baseline and routine data mainly on violence against health workers [304]. In contrast to conflict settings, primary studies represented the most frequent type of publications on health care workers in post-conflict settings. These findings might relate to the specific settings in which the conflict and post-conflict studies were conducted. However, they might also reflect the challenges in conducting primary research in conflict settings, including security concerns, difficulties in obtaining representative samples and with data collection, political bias, lack of tools and methods specific to conflict settings, and insufficient research funding and capacity [1, 304, 471].
The majority of authors (including first and corresponding) of the included papers were affiliated with high income counties, as opposed to being affiliated with the country focus of the paper. This finding may reflect global imbalances in research capacity between high- and low- and middle-income countries [472–474]. Reasons for this imbalance include limited funding, instability, poor research training, collaboration challenges, and shortage of skilled human resources in low and middle income countries [1, 473–477].
As most of the articles addressing health care workers in conflict and post-conflict are about low-income countries, we can infer that conflicts are still taking place in these countries that already suffer from weak health systems [478]. Our findings are consistent with the previously published scoping review focusing on health care workers in the setting of Arab Spring which found that violence was the most tackled theme [7]. Findings for post-conflict settings concur with a previous review by Roome et al. (2014) on human resources management in post-conflict health systems [5]. This shows the need for more studies on the topic of workforce distribution, which is important to ensure equity in health service provision.
Another interesting finding is the low rates of reporting of funding sources and disclosures of conflict of interest by authors of the included studies. This is particularly for papers about HCWs in conflict settings. Indeed, funders may have specific agendas while researchers may have political biases and tendency to take sides [471]. These may lead to distorted research and biased data that could be used to mislead local and international communities and negatively affect policy making. Reporting of funding sources and conflict of interest becomes important to better assess the confidence in the publication, particularly when it reports primary studies or makes policy recommendations.
We also found a relatively low reporting of ethical approvals for primary studies, in both conflict and post-conflict settings. This might be attributed to a weak local research capacity including the absence of or complicated ethical review boards [1]. Reporting and seeking ethical approvals in these settings is important given the vulnerability of individuals living in conflict-affected states [479]. This calls journals publishing research conducted in conflict settings to have stringent policies for reporting funding, conflict of interest and ethical approval.
To our knowledge, this is the first systematic mapping of evidence on health care workers in conflict and post-conflict settings. One strength of this study is that we have followed a standardized methodology for conducting and reporting systematic mapping [9]. Further, we have used published frameworks to classify studies on HCWs in conflict and post-conflict settings [5, 7]. One limitation of this study is restricting inclusion to studies published after the year 2000. However, studies published before 2000 might not reflect the current challenges facing health systems and the new aspects of contemporary conflicts. Another limitation of our systematic map is that we relied on the authors’ characterization of the conflict (e.g., conflict or post-conflict), and subsequently we did not differentiate between countries in conflict such as Somalia, Iraq and Syria, and those affected by conflict such as Lebanon.
The findings of this review and the resulting systematic maps can support policy makers working on rebuilding health systems post-conflict. These systematic maps provide a comprehensive resource of evidence about HCWs in conflict and post-conflict settings on a global scale. As such, policymakers as well as researchers can use them to find relevant studies by theme. In addition, the mapped evidence can inform policies and practices to protect, support and address the needs of the health care workers in conflict settings. The evidence identified can also inform efforts and strategies for reconstruction and rebuilding of post-conflict health systems, in particular human resource for health.
The findings also highlight the need to strengthen the capacity of local researchers working in conflict-affected states. Also, they can inform agendas of funders and researchers working in the field of health care workers in conflict and post-conflict settings of potential knowledge gaps. This systematic map will inform areas for potential systematic reviews in the field, and may provide a jumpstart for those reviews, given that the relevant studies have already been identified and organized by theme.
Supporting information
(DOCX)
(DOCX)
(PDF)
(XLSX)
Acknowledgments
We would like to thank Mr. Mahmoud Chmeiss for designing the geographical map of the included papers, Ms. Nour Hemadi for helping in the screening process and Ms. Karen Bou-Karroum, Ms. Rand Al Ghoussaini and Mr. Mark Jreij for helping in the data abstraction process.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
EAA and FEJ received funding from the Lebanese National Council for Scientific Research (CNRS)-American University of Beirut (AUB) and the Alliance for Health Policy and Systems Research of the World Health Organization (WHO). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Woodward A, Sheahan K, Martineau T, Sondorp E. Health systems research in fragile and conflict affected states: a qualitative study of associated challenges. Health Research Policy and Systems. 2017;15(1):44 10.1186/s12961-017-0204-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conflict SHi. No Protection No Respect. 2016.
- 3.Rubenstein RJHLS. Health in Postconflict and Fragile States. United States Institute of Peace. 2012;Special Report 301.
- 4.Martineau T, McPake B, Theobald S, Raven J, Ensor T, Fustukian S, et al. Leaving no one behind: lessons on rebuilding health systems in conflict- and crisis-affected states. BMJ Global Health. 2017;2(2):e000327 10.1136/bmjgh-2017-000327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roome E, Raven J, Martineau T. Human resource management in post-conflict health systems: review of research and knowledge gaps. Conflict and health. 2014;8:18 Epub 2014/10/09. 10.1186/1752-1505-8-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHA WHA. WHO’s response, and role as the health cluster lead, in meeting the growing demands of health in humanitarian emergencies. 2012.
- 7.Bou-Karroum L, Daou KN, Nomier M, El Arnaout N, Fouad FM, El-Jardali F, et al. Health Care Workers in the setting of the "Arab Spring": a scoping review for the Lancet-AUB Commission on Syria. J Glob Health. 2019;9(1):010402–. 10.7189/jogh.09.010402 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khamis AM, Hakoum MB, Bou-Karroum L, Habib JR, Ali A, Guyatt G, et al. Requirements of health policy and services journals for authors to disclose financial and non-financial conflicts of interest: a cross-sectional study. Health Research Policy and Systems. 2017;15(1):80 10.1186/s12961-017-0244-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environmental Evidence. 2016;5(1):7 10.1186/s13750-016-0059-6 [DOI] [Google Scholar]
- 10.Saran A, White H. Evidence and gap maps: a comparison of different approaches. Campbell Systematic Reviews. 2018;14(1):1–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ICRC ICotRC. How is the term "Armed Conflict" defined in international humanitarian law? 2008.
- 12.McPake B. Health systems in conflict affected states—are they different from in other low and middle income countries? Early ideas from the work of the ReBUILD programme. ReBuild Consortium; 2017. [Google Scholar]
- 13.Ahonsi BA. Towards more informed responses to gender violence and HIV/AIDS in post-conflict West African settings: Nordiska Afrikainstitutet; 2010. [Google Scholar]
- 14.The L. A tribute to aid workers. Lancet. 2006;368(9536):620 . [DOI] [PubMed] [Google Scholar]
- 15.Abbara A, Orcutt M, Gabbar O. Syria's lost generation of doctors. BMJ. 2015;350:h3479 10.1136/bmj.h3479 . [DOI] [PubMed] [Google Scholar]
- 16.Abdou R, Romm I, Schiff D, Austad K, Dubal S, Kimmel S, et al. In solidarity with Gaza. Lancet. 2009;373(9660):295 10.1016/S0140-6736(09)60042-8 . [DOI] [PubMed] [Google Scholar]
- 17.Abramovitch H. Making war a part of medical education. Israel Medical Association Journal: Imaj. 2013;15(3):174–5. . [PubMed] [Google Scholar]
- 18.Abrams E. Saving my heart. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2009;181(6–7):E115 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abramsky O. Letter to the Royal College of Physicians (London): Take anti-Israeli politics out of medicine. Israel Medical Association Journal. 2009;11(6):334 . [PubMed] [Google Scholar]
- 20.Abu-El-Noor NI, Aljeesh YI, Radwan AS, Abu-El-Noor MK, Qddura IA, Khadoura KJ, et al. Post-Traumatic Stress Disorder Among Health Care Providers Following the Israeli Attacks Against Gaza Strip in 2014: A Call for Immediate Policy Actions. Archives of Psychiatric Nursing. 2016;30(2):185–91. 10.1016/j.apnu.2015.08.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Acerra JR, Iskyan K, Qureshi ZA, Sharma RK. Rebuilding the health care system in Afghanistan: An overview of primary care and emergency services. International Journal of Emergency Medicine. 2009;2(2):77–82. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams E. Human rights and health in conflict zones. World of Irish Nursing & Midwifery. 2016;24(8):22–3. . Language: English. Entry Date: 20170113. Revision Date: 20170113. Publication Type: Article. Journal Subset: Europe. [Google Scholar]
- 23.Adil M, Johnstone P, Furber A, Siddiqi K, Khan D. Violence against public health workers during armed conflicts. Lancet. 2013. January 5;381(9860):1 Lancet. 2013;381 North American Edition(9863):293-. 10.1016/S0140-6736(13)60127-0 . Language: English. Entry Date: 20130222. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 24.Afkhami AA. Psychiatry and efforts to build community in Iraq. American Journal of Psychiatry. 2014;171(9):913–5. . [DOI] [PubMed] [Google Scholar]
- 25.Ahmadzai TK, Maburutse Z, Miller L, Ratnayake R. Protecting public health in Yemen. The Lancet. 2016;388(10061):2739 . [DOI] [PubMed] [Google Scholar]
- 26.Ahmed F. The sideline or frontline: where should the UK medical profession stand in times of armed conflict overseas? BMJ: British Medical Journal. 2014;348(7940):26–. . Language: English. Entry Date: 20140115. Revision Date: 20150710. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 27.Aiga H, Pariyo GW. Violence against health workers during armed conflict. Lancet. 2013. January 26;381(9863):293 Lancet. 2013;381 North American Edition(9874):1276-. 10.1016/S0140-6736(13)60839-9 . Language: English. Entry Date: 20130517. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 28.Al Mosawi AJ. Medical education and the physician workforce of Iraq. Journal of Continuing Education in the Health Professions. 2008;28(2):103–5. . Language: English. Entry Date: 20080905. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 29.Alasaad S. War diseases revealed by the social media: Massive leishmaniasis outbreak in the Syrian Spring. Parasites and Vectors. 2013;6 (1) (no pagination)(94). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alkan ML, Shwartz S. Medical services for rural Ethiopean Jews in Addis Ababa, 1990–1991. Rural and remote health. 2007;7(4):829 . [PubMed] [Google Scholar]
- 31.Al-Kindi S. Violence against doctors in Iraq. The Lancet. 2014;384(9947):954–5. . [DOI] [PubMed] [Google Scholar]
- 32.Allan R. Where are you from? Clinical Medicine. 2007;7(2):101–2. 10.7861/clinmedicine.7-2-101a . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ameh CA, Bishop S, Kongnyuy E, Grady K, Van den Broek N. Challenges to the provision of emergency obstetric care in iraq. Maternal & Child Health Journal. 2011;15(1):4–11. 10.1007/s10995-009-0545-3 . Language: English. Entry Date: 20110131. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 34.Amin NM, Khoshnaw MQ. Medical education and training in Iraq. Lancet. 2003;362(9392):1326 10.1016/s0140-6736(03)14580-1 . [DOI] [PubMed] [Google Scholar]
- 35.Anonymous. Defining the limits of public health. Lancet. 2000;355(9204):587 10.1159/000491433 . [DOI] [PubMed] [Google Scholar]
- 36.Nurse pledges to stay in war zone. Nursing Standard. 2001;16(5): 4–. . Language: English. Entry Date: 20020118. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 37.Plea for safety in war zones. Nursing Standard. 2002;16(31):6–. . Language: English. Entry Date: 20020614. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 38.Health professions speak out against armed conflict. Canadian Nurse. 2003;99(5):32–. . Language: English. Entry Date: 20030711. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 39.Anonymous. Help needed for East Timor nurses. Australian nursing journal (July 1993). 2006;14(1):15 . [PubMed] [Google Scholar]
- 40.Nurses gear up to help treat injured children in war zone. Paediatric Nursing. 2010;22(3):5–. . Language: English. Entry Date: 20100604. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 41.Charities send aid and staff to Libya. Nursing Standard. 2011;26(1):6–. . Language: English. Entry Date: 20110930. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 42.Anonymous. A medical crisis in Syria. Lancet. 2012;380(9841):537 10.1016/S0140-6736(12)61309-9 . [DOI] [PubMed] [Google Scholar]
- 43.Anonymous. Health Care in Danger: Deliberate Attacks on Health Care during Armed Conflict. PLoS Medicine. 2014;11(6):1–2. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anonymous. The war on Syrian civilians. The Lancet. 2014;383(9915):383 . [DOI] [PubMed] [Google Scholar]
- 45.Anonymous. Care for the carers. Nature. 2015;527(7576):7–8. . [DOI] [PubMed] [Google Scholar]
- 46.Anonymous. Syria: a health crisis too great to ignore. Lancet. 2016;388(10039):2 10.1016/S0140-6736(16)30936-9 . [DOI] [PubMed] [Google Scholar]
- 47.Nurses' flight worsens Middle Eastern health crisis. Lamp. 2017;74(1):22–3. . Language: English. Entry Date: 20170208. Revision Date: 20170210. Publication Type: Article. Journal Subset: Australia & New Zealand. [Google Scholar]
- 48.The L. Syria suffers as the world watches. The Lancet. 2017;389(10074):1075 . [DOI] [PubMed] [Google Scholar]
- 49.Arias-López BE. Care and social suffering: nursing within contexts of political violence. Investigacion & Educacion en Enfermeria. 2013;31(1):125–32. . Language: English. Entry Date: 20130606. Revision Date: 20150820. Publication Type: Journal Article. Journal Subset: Mexico & Central/South America. [Google Scholar]
- 50.Arie S. Gaddafi's forces attacked hospitals, patients, and health professionals, report confirms. BMJ (Clinical research ed). 2011;343:d5533 . [DOI] [PubMed] [Google Scholar]
- 51.Arie S. Charity donations in name of UK doctor killed in Syria rise beyond expectations. BMJ (Clinical research ed). 2013;346 (no pagination)(f3592). . [DOI] [PubMed] [Google Scholar]
- 52.Arie S. Family of missing UK doctor says he entered Syria with 20,000 in medical supplies to provide aid. BMJ (Clinical research ed). 2013;346 (no pagination)(f681). . [DOI] [PubMed] [Google Scholar]
- 53.Arie S. Investigate death of British doctor in Syria, say campaigners. BMJ (Clinical research ed). 2013;347 (no pagination)(f7647). . [DOI] [PubMed] [Google Scholar]
- 54.Arie S. Islamic State executes 10 doctors for refusing to treat its wounded fighters. BMJ (Clinical research ed). 2015;350:h1963 . [DOI] [PubMed] [Google Scholar]
- 55.Asia MR, Georges JM, Hunter AJ. Research in conflict zones: implications for nurse researchers. Advances in Nursing Science. 2010;33(2):94–100. 10.1097/ANS.0b013e3181d52dd4 . Language: English. Entry Date: 20100709. Revision Date: 20150818. Publication Type: Journal Article. Journal Subset: Core Nursing. [DOI] [PubMed] [Google Scholar]
- 56.Austin H. 'The situation is worse than before the war'. Nursing Standard. 2003;17(46):8–. . Language: English. Entry Date: 20040116. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 57.Bagaric I. Medical services of Croat people in Bosnia and Herzegovina during 1992–1995 war: Losses, adaptation, organization, and transformation. Croatian Medical Journal. 2000;41(2):124–40. 10.1111/idj.12450 . [DOI] [PubMed] [Google Scholar]
- 58.Band-Winterstein T, Koren C. "We take care of the older person, who takes care of us?" Professionals working with older persons in a shared war reality. Journal of Applied Gerontology. 2010;29(6):772–92. . [Google Scholar]
- 59.Bar-El Y, Reisner S, Beyar R. Moral dilemmas faced by hospitals in time of war: the Rambam Medical Center during the second Lebanon war. Medicine, health care, and philosophy. 2014;17(1):155–60. . [DOI] [PubMed] [Google Scholar]
- 60.Barmania S. Undercover medicine: Treating Syria's wounded. The Lancet. 2012;379(9830):1936–7. . [DOI] [PubMed] [Google Scholar]
- 61.Baroness Cox C. The Baroness Cox of Queensbury. Nursing ethics. 2003;10(4):441–5. . [DOI] [PubMed] [Google Scholar]
- 62.Batley NJ, Makhoul J, Latif SA. War as a positive medical educational experience. Medical Education. 2008;42(12):1166–71. . Language: English. Entry Date: 20090522. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 63.Ben-Ezra M, Bibi H. The Association Between Psychological Distress and Decision Regret During Armed Conflict Among Hospital Personnel. Psychiatric Quarterly. 2016;87(3):515–9. . [DOI] [PubMed] [Google Scholar]
- 64.Ben-Ezra M, Palgi Y, Essar N. Impact of war stress on posttraumatic stress symptoms in hospital personnel. General Hospital Psychiatry. 2007;29(3):264–6. . Language: English. Entry Date: 20071130. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 65.Ben-Ezra M, Palgi Y, Essar N. The impact of exposure to war stress on hospital staff: A preliminary report. Journal of Psychiatric Research. 2008;42(5):422–3. . [DOI] [PubMed] [Google Scholar]
- 66.Ben-Ezra M, Palgi Y, Shrira A, Hamama-Raz Y. Somatization and Psychiatric Symptoms among Hospital Nurses Exposed to War Stressors. Israel Journal of Psychiatry & Related Sciences. 2013;50(3):182–6. . Language: English. Entry Date: 20150904. Revision Date: 20150923. Publication Type: Journal Article. [PubMed] [Google Scholar]
- 67.Ben-Ezra M, Palgi Y, Wolf JJ, Shrira A. Psychiatric symptoms and psychosocial functioning among hospital personnel during the Gaza War: a repeated cross-sectional study. Psychiatry research [Internet]. 2011; 189(3):[392–5 pp.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/483/CN-00801483/frame.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ben-Ezra M, Palgi Y, Wolf JJ, Shrira A. Psychosomatic symptoms among hospital physicians during the Gaza War: a repeated cross-sectional study. Israel journal of psychiatry and related sciences [Internet]. 2011; 48(3):[170–4 pp.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/330/CN-00804330/frame.html. [PubMed] [Google Scholar]
- 69.Bergovec M, Kuzman T, Rojnic M, Makovic A. Zagreb University School of Medicine: Students' grades during war. Croatian Medical Journal. 2002;43(1):67–70. . [PubMed] [Google Scholar]
- 70.Betsi NA, Koudou BG, Cisse G, Tschannen AB, Pignol AM, Ouattara Y, et al. Effect of an armed conflict on human resources and health systems in Cote d'Ivoire: Prevention of and care for people with HIV/AIDS. AIDS Care—Psychological and Socio-Medical Aspects of AIDS/HIV. 2006;18(4):356–65. . [DOI] [PubMed] [Google Scholar]
- 71.Birch M. A risk worth taking. Nursing standard (Royal College of Nursing (Great Britain): 1987). 2001;16(12):60–1. . [DOI] [PubMed] [Google Scholar]
- 72.Birch M, Ratneswaren S. From Solferino to Sri Lanka: health workers, health information, and international law. Medicine, conflict, and survival. 2009;25(3):191–2. . [DOI] [PubMed] [Google Scholar]
- 73.Bloem C, Morris RE, Chisolm-Straker M. Human Trafficking in Areas of Conflict: Health Care Professionals' Duty to Act. AMA journal of ethics. 2017;19(1):72–9. . [DOI] [PubMed] [Google Scholar]
- 74.Bloom JD, Sondorp E. Relations between ethnic Croats and ethnic Serbs at Vukovar General Hospital in wartime and peacetime. Medicine, conflict, and survival. 2006;22(2):110–31. . [DOI] [PubMed] [Google Scholar]
- 75.Boehm A. The functions of social service workers at a time of war against a civilian population. Disasters. 2010;34(1):261–86. . [DOI] [PubMed] [Google Scholar]
- 76.Bolza R. Delivering hope—and babies—in a war-torn land. Interview by Laura Putre. Hospitals & Health Networks. 2010;84(11):17 . [PubMed] [Google Scholar]
- 77.Boren D. Physician obligations to help document the atrocities of war. The Virtual Mentor. 2007;9(10):692–4. 10.1001/virtualmentor.2007.9.10.jdsc1-0710 . [DOI] [PubMed] [Google Scholar]
- 78.Bradbeer M. Safeguard nurses at war…Cover story about workplace violence, ANJ July 2011. Australian Nursing Journal. 2011;19(4):3–. Language: English. Entry Date: 10.1038/oby.2010.5 Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 79.Brook OR. Recollections of a radiology resident at war. Radiology. 2007;244(2):329–30. . [DOI] [PubMed] [Google Scholar]
- 80.Brundtland GH, Glinka E, Hausen HZ, D'Avila RL. Open letter: Let us treat patients in Syria. The Lancet. 2013;382(9897):1019–20. . [DOI] [PubMed] [Google Scholar]
- 81.Brunham L, Lee P, Pinto A. Medical students not mum on Iraq. CMAJ Canadian Medical Association Journal. 2003;169(6):541 . [PMC free article] [PubMed] [Google Scholar]
- 82.Burkle FM Jr, Erickson TB, Von Schreeb J, Redmond AD, Kayden S, Van Rooyen M, et al. A declaration to the UN on wars in the Middle East. Philadelphia, Pennsylvania: Lancet; 2017. p. 699–700. [DOI] [PubMed] [Google Scholar]
- 83.Burkle FM Jr., Erickson T, von Schreeb J, Kayden S, Redmond A, Chan EY, et al. The Solidarity and Health Neutrality of Physicians in War & Peace. PLoS currents. 2017;9:20 10.1371/currents.dis.1a1e352febd595087cbeb83753d93a4c . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Burnham G, Malik S, Dhari Al-Shibli AS, Mahjoub AR, Baqer AQ, Baqer ZQ, et al. Understanding the impact of conflict on health services in Iraq: Information from 401 Iraqi refugee doctors in Jordan. International Journal of Health Planning and Management. 2012;27(1):e51–e64. . [DOI] [PubMed] [Google Scholar]
- 85.Byamungu DC, Ogbeiwi OI. Integrating leprosy control into general health service in a war situation: The level after 5 years in Eastern Congo. Leprosy Review. 2003;74(1):68–78. . [PubMed] [Google Scholar]
- 86.Carlisle D. In the line of fire. Nursing Standard. 2012;26(39):18–9. . Language: English. Entry Date: 20120622. Revision Date: 20150819. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 87.Carmichael JL, Karamouzian M. Deadly professions: violent attacks against aid-workers and the health implications for local populations. International Journal of Health Policy & Management. 2014;2(2):65–7. 10.15171/ijhpm.2014.16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Casey SE, Mitchell KT, Amisi IM, Haliza MM, Aveledi B, Kalenga P, et al. Use of facility assessment data to improve reproductive health service delivery in the Democratic Republic of the Congo. Conflict & Health [Electronic Resource]. 2009;3:12 10.1186/1752-1505-3-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Catton H. It takes a brave heart to be a nurse in a war-torn country. RCNi; 2016. p. 28–. [DOI] [PubMed] [Google Scholar]
- 90.Challoner KR, Forget N. Effect of civil war on medical education in Liberia. International Journal of Emergency Medicine. 2011;4(1). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chi PC, Bulage P, Urdal H, Sundby J. Perceptions of the effects of armed conflict on maternal and reproductive health services and outcomes in Burundi and Northern Uganda: A qualitative study. BMC International Health and Human Rights. 2015;15 (1) (no pagination)(7). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Clarfield AM. Close calls. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2009;180(12):E98 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Clark JR. Civilians in a War Zone. Air Medical Journal. 2016;35(5). . [DOI] [PubMed] [Google Scholar]
- 94.Cohn JR, Romirowsky A, Marcus JM. Abuse of health-care workers' neutral status [1]. Lancet. 2004;363(9419):1473 . [DOI] [PubMed] [Google Scholar]
- 95.Corcione A, Petrini F, Gristina G, De Robertis E. A statement on the war in Syria from SIAARTI and partners. The Lancet. 2017;389(10064):31 . [DOI] [PubMed] [Google Scholar]
- 96.Coupland R, Cordner S. People missing as a result of armed conflict: standards and guidelines are needed for all, including health professionals. BMJ: British Medical Journal (International Edition). 2003;326(7396):943–4. . Language: English. Entry Date: 20030718. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cousins S. Syrian crisis: Health experts say more can be done. The Lancet. 2015;385(9972):931–4. . [DOI] [PubMed] [Google Scholar]
- 98.Davenport A. Healthcare in Kosovo. Midwifery today with international midwife. 2000;(53):50–2. . [PubMed] [Google Scholar]
- 99.Davis M, Goldstein K, Nasser T, Assaf C. Peace through Health: The Role of Health Workers in Preventing Emergency Care Needs. Academic Emergency Medicine. 2006;13(12):1324–7. . [DOI] [PubMed] [Google Scholar]
- 100.de Val D'Espaux S, Madi B, Nasif J, Arabasi M, Raddad S, Madi A, et al. Strengthening mental health care in the health system in the occupied Palestinian territory. Intervention (15718883). 2011;9(3):279–90. 10.1097/WTF.0b013e32834dea41 . Language: English. Entry Date: 20120217. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [Google Scholar]
- 101.Dean E. Nursing in the world's most challenging places. Nursing Standard. 2016;30(48):38–9. . Language: English. Entry Date: 20160801. Revision Date: 20160801. Publication Type: Article. Journal Subset: Double Blind Peer Reviewed. [DOI] [PubMed] [Google Scholar]
- 102.Decker JT, Constantine Brown JL, Tapia J. Learning to Work with Trauma Survivors: Lessons from Tbilisi, Georgia. Social Work in Public Health. 2017;32(1):53–64. 10.1080/19371918.2016.1188744 . [DOI] [PubMed] [Google Scholar]
- 103.D'Errico NC, Wake CM, Wake RM. Healing Africa? Reflections on the peace-building role of a health-based non governmental organization operating in eastern Democratic Republic of Congo. Medicine, conflict, and survival. 2010;26(2):145–59. . [DOI] [PubMed] [Google Scholar]
- 104.Devi S. Syria's refugees face a bleak winter. The Lancet. 2012;380(9851):1373–4. . [DOI] [PubMed] [Google Scholar]
- 105.Devi S. Syria's health crisis: 5 years on. The Lancet. 2016;387(10023):1042–3. . [DOI] [PubMed] [Google Scholar]
- 106.Devkota B, van Teijlingen ER. Politicians in apron: case study of rebel health services in Nepal. Asia-Pacific Journal of Public Health. 2009;21(4):377–84. 10.1177/1010539509342434 . Language: English. Entry Date: 20091204. Revision Date: 20150819. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 107.Dewachi O, Skelton M, Nguyen VK, Fouad FM, Sitta GA, Maasri Z, et al. Changing therapeutic geographies of the Iraqi and Syrian wars.[Erratum appears in Lancet. 2014 Feb 1;383(9915):412]. Lancet. 2014;383(9915):449–57. 10.1016/S0140-6736(13)62299-0 . [DOI] [PubMed] [Google Scholar]
- 108.Donaldson RI, Mulligan DA, Nugent K, Cabral M, Saleeby ER, Ansari W, et al. Using tele-education to train civilian physicians in an area of active conflict: certifying iraqi physicians in pediatric advanced life support from the United States. Journal of Pediatrics. 2011;159(3):507–9.e1. . Language: English. Entry Date: 20111118. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 109.Donaldson RI, Shanovich P, Shetty P, Clark E, Aziz S, Morton M, et al. A survey of national physicians working in an active conflict zone: the challenges of emergency medical care in iraq. Prehospital & Disaster Medicine. 2012;27(2):153–61. . Language: English. Entry Date: 20120914. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 110.Doocy S, Malik S, Burnham G. Experiences of Iraqi doctors in Jordan during conflict and factors associated with migration. American journal of disaster medicine. 2010;5(1):41–7. . [DOI] [PubMed] [Google Scholar]
- 111.Duffin C. Aid work 'in jeopardy' as combatants in war zones target charity services. Emergency nurse: the journal of the RCN Accident and Emergency Nursing Association. 2010;18(2):7 . [PubMed] [Google Scholar]
- 112.Dumont F. On the ground in the Gaza Strip. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2009;180(6):610 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Durham J, Pavignani E, Beesley M, Hill PS. Human resources for health in six healthcare arenas under stress: a qualitative study. Human resources for health. 2015;13:14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Dyer E. Nursing in Goma, Congo. The American journal of nursing. 2002;102(5):87, 9, 91. . [DOI] [PubMed] [Google Scholar]
- 115.Eaton L. Doctors must speak out over war and humanitarian crises. BMJ (Clinical research ed). 2001;323(7316):771 . [PMC free article] [PubMed] [Google Scholar]
- 116.Eisenkraft A, Gilburd D, Kassirer M, Kreiss Y. What can we learn on medical preparedness from the use of chemical agents against civilians in Syria? American Journal of Emergency Medicine. 2014;32(2):186 . [DOI] [PubMed] [Google Scholar]
- 117.El Jamil F, Hamadeh GN, Osman H. Experiences of a support group for interns in the setting of war and political turmoil. Family Medicine. 2007;39(9):656–8. . [PubMed] [Google Scholar]
- 118.Elamein M, Bower H, Valderrama C, Zedan D, Rihawi H, Almilaji K, et al. Attacks against health care in Syria, 2015–16: Results from a real-time reporting tool. The Lancet. 2017. . [DOI] [PubMed] [Google Scholar]
- 119.El-Fiki M, Rosseau G. The 2011 Egyptian revolution: A neurosurgical perspective. World Neurosurgery. 2011;76(1–2):28–32. . [DOI] [PubMed] [Google Scholar]
- 120.Essar N, Ben-Ezra M, Langer S, Palgi Y. Gender differences in response to war stress in hospital personnel: Does profession matter? A preliminary study. European Journal of Psychiatry. 2008;22(2):77–83. . [Google Scholar]
- 121.Zarocostas J. Libya's health system struggles after exodus of foreign medical staff. BMJ (Clinical research ed). 2011;342:d1879 . [DOI] [PubMed] [Google Scholar]
- 122.Wisborg T, Murad MK, Edvardsen O, Husum H. Prehospital trauma system in a low-income country: system maturation and adaptation during 8 years. Journal of Trauma. 2008;64(5):1342–8. . Language: English. Entry Date: 20080620. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 123.Wilson JF. Physicians contribute professional expertise worldwide. Annals of internal medicine. 2003;138(12):1013–6. . [DOI] [PubMed] [Google Scholar]
- 124.Webster PC. Iraq's growing health crisis. Lancet. 2014;384(9938):119–20. 10.1016/s0140-6736(14)61148-x . [DOI] [PubMed] [Google Scholar]
- 125.Webster PC. The deadly effects of violence against medical workers in war zones. CMAJ: Canadian Medical Association Journal. 2011;183(13):E981–2. 10.1503/cmaj.109-3964 . Language: English. Entry Date: 20111118. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Webster P. Facility attacks in Syria contravene Geneva Convention. CMAJ: Canadian Medical Association Journal. 2016;188(7):491–. 10.1503/cmaj.109-5249 . Language: English. Entry Date: 20160903. Revision Date: 20170421. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Webster P. Medical faculties decimated by violence in Iraq. CMAJ Canadian Medical Association Journal. 2009;181(9):576–8. 10.1503/cmaj.109-3035 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Weaver K. Caring for the living and the dead. Nursing Standard. 2004;18(18):18–9. . Language: English. Entry Date: 20050712. Revision Date: 20150711. Publication Type: Journal Article. [PubMed] [Google Scholar]
- 129.Washington CH, Tyler FJ, Davis J, Shapiro DR, Richards A, Richard M, et al. Trauma training course: innovative teaching models and methods for training health workers in active conflict zones of Eastern Myanmar. International Journal of Emergency Medicine. 2014;7(1). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Anderson K. Working in a war zone. Interview by Lynne Wallis. Nursing standard (Royal College of Nursing (Great Britain): 1987). 2001;15(24):19–20. . [PubMed] [Google Scholar]
- 131.Wakabi W. South Sudan faces grim health and humanitarian situation. The Lancet. 2011;377(9784):2167–8. . [DOI] [PubMed] [Google Scholar]
- 132.Wakabi W. WHO trains surgeons in troubled Somalia. Lancet. 2010;375(9723):1336 . [DOI] [PubMed] [Google Scholar]
- 133.Fernandez G, Boulle P. Where conflict's medical consequences remain unchanged. The Lancet. 2013;381(9870):901 . [DOI] [PubMed] [Google Scholar]
- 134.Fisher RC. Musculoskeletal trauma services in Mozambique and Sri Lanka. Clinical Orthopaedics and Related Research. 2008;466(10):2399–402. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Foghammar L, Jang S, Kyzy GA, Weiss N, Sullivan KA, Gibson-Fall F, et al. Challenges in researching violence affecting health service delivery in complex security environments. Social Science & Medicine. 2016;162:219–26. 10.1016/j.socscimed.2016.03.039 . Language: English. Entry Date: 20160724. Revision Date: 20160908. Publication Type: Article. Journal Subset: Allied Health. [DOI] [PubMed] [Google Scholar]
- 136.Footer KH, Meyer S, Sherman SG, Rubenstein L. On the frontline of eastern Burma's chronic conflict—listening to the voices of local health workers. Social Science & Medicine. 2014;120:378–86. 10.1016/j.socscimed.2014.02.019 . [DOI] [PubMed] [Google Scholar]
- 137.Fouad FM, Alameddine M, Coutts A. Human resources in protracted crises: Syrian medical workers. Philadelphia, Pennsylvania: Lancet; 2016. p. 1613–. [DOI] [PubMed] [Google Scholar]
- 138.Fouad FM, Sparrow A, Tarakji A, Alameddine M, El-Jardali F, Coutts AP, et al. Health workers and the weaponisation of health care in Syria: A preliminary inquiry for The Lancet-American University of Beirut Commission on Syria. The Lancet. 2017. . [DOI] [PubMed] [Google Scholar]
- 139.Friedrich MJ. Human rights report details violence against health care workers in Bahrain. JAMA. 2011;306(5):475–6. 10.1001/jama.2011.1091 . [DOI] [PubMed] [Google Scholar]
- 140.Garfield R. Health professionals in Syria. Lancet. 2013;382(9888):205–6. 10.1016/S0140-6736(13)61507-X . [DOI] [PubMed] [Google Scholar]
- 141.Garfield R, Dresden E, Boyle JS. Health care in Iraq. Nursing Outlook. 2003;51(4):171–7. . Language: English. Entry Date: 20031121. Revision Date: 20150818. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 142.Gately R. Humanitarian aid to Iraqi Civilians during the war: A US nurse's role. Journal of Emergency Nursing. 2004;30(3):230–6. . [DOI] [PubMed] [Google Scholar]
- 143.Gearey J. A call to unite: physicians must help children in areas of conflict. CMAJ: Canadian Medical Association Journal. 2007;176(10):1407–. . Language: English. Entry Date: 20070713. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Vostanis P. Healthcare professionals in war zones are vulnerable too. Journal of Psychiatric & Mental Health Nursing. 2015;22(10):747–8. 10.1111/jpm.12272 . Language: English. Entry Date: 20151218. Revision Date: 20161130. Publication Type: Editorial. Journal Subset: Core Nursing. [DOI] [PubMed] [Google Scholar]
- 145.Vogel L. UN inaction emboldens attacks on health care. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2016;188(17–18):E415–E6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Voelker R. Iraqi health minister works to reform, restore neglected system. JAMA—Journal of the American Medical Association. 2008;300(6):639 . [DOI] [PubMed] [Google Scholar]
- 147.Viola JM. On the letters on the war. The American journal of nursing. 2003;103(5):16; discussion . [DOI] [PubMed] [Google Scholar]
- 148.Veronese G, Pepe A, Massaiu I, De Mol AS, Robbins I. Posttraumatic growth is related to subjective well-being of aid workers exposed to cumulative trauma in Palestine. Transcultural Psychiatry. 2017;54(3):332–56. . [DOI] [PubMed] [Google Scholar]
- 149.Veronese G, Pepe A, Afana A. Conceptualizing the well-being of helpers living and working in war-like conditions: A mixed-method approach. International Social Work. 2016;59(6):938–52. 10.1177/0020872814537855 . Language: English. Entry Date: 20161111. Revision Date: 20170203. Publication Type: Article. Journal Subset: Allied Health. [DOI] [Google Scholar]
- 150.Veronese G, Pepe A. Sense of Coherence as a Determinant of Psychological Well-Being Across Professional Groups of Aid Workers Exposed to War Trauma. Journal of Interpersonal Violence. 2015;18:18 10.1177/0886260515590125 . [DOI] [PubMed] [Google Scholar]
- 151.Veronese G. Self-perceptions of well-being in professional helpers and volunteers operating in war contexts. Journal of health psychology. 2013;18(7):911–25. . [DOI] [PubMed] [Google Scholar]
- 152.Abandonments Varley E., Solidarities and Logics of Care: Hospitals as Sites of Sectarian Conflict in Gilgit-Baltistan. Culture, Medicine & Psychiatry. 2016;40(2):159–80. 10.1007/s11013-015-9456-5 . [DOI] [PubMed] [Google Scholar]
- 153.Varley E. Targeted doctors, missing patients: Obstetric health services and sectarian conflict in Northern Pakistan. Social Science and Medicine. 2010;70(1):61–70. . [DOI] [PubMed] [Google Scholar]
- 154.VanRooyen M, Venugopal R, Greenough PG. International humanitarian assistance: where do emergency physicians belong? Emergency Medicine Clinics of North America. 2005;23(1):115–31. . Language: English. Entry Date: 20051028. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 155.VanRooyen MJ, Eliades MJ, Grabowski JG, Stress ME, Juric J, Burkle FM Jr. Medical relief personnel in complex emergencies: perceptions of effectiveness in the former Yugoslavia. Prehospital & Disaster Medicine. 2001;16(3):145–9. . Language: English. Entry Date: 20030711. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 156.Urlic I. Recognizing inner and outer realities as a process: On some countertransferential issues of the group conductor. Group Analysis. 2005;38(2):249–63. . [Google Scholar]
- 157.Turk T, Aboshady OA, Albittar A. Studying medicine in crisis: Students' perspectives from Syria. Philadelphia, Pennsylvania: Taylor & Francis Ltd; 2016. p. 861–2. [DOI] [PubMed] [Google Scholar]
- 158.Tschudin V, Schmitz C. The impact of conflict and war on international nursing and ethics. Nursing Ethics. 2003;10(4):354–67. 10.1191/0969733003ne618oa . Language: English. Entry Date: 20050425. Revision Date: 20150818. Publication Type: Journal Article. Journal Subset: Double Blind Peer Reviewed. [DOI] [PubMed] [Google Scholar]
- 159.Tiembre I, Benie J, Coulibaly A, Dagnan S, Ekra D, Coulibaly S, et al. Impact of armed conflict on the health care system of a sanitary district in Cote d'Ivoire. [French] Impact du conflit arme sur le systeme de sante d'un district sanitaire en Cote d'Ivoire. Medecine Tropicale. 2011;71(3):249–52. . [PubMed] [Google Scholar]
- 160.Teela KC, Mullany LC, Lee CI, Poh E, Paw P, Masenior N, et al. Community-based delivery of maternal care in conflict-affected areas of eastern Burma: perspectives from lay maternal health workers. Social Science & Medicine. 2009;68(7):1332–40. 10.1016/j.socscimed.2009.01.033 . Language: English. Entry Date: 20090710. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 161.Tanabe M, Robinson K, Lee CI, Leigh JA, Htoo EM, Integer N, et al. Piloting community-based medical care for survivors of sexual assault in conflict-affected Karen State of eastern Burma. Conflict & Health [Electronic Resource]. 2013;7(1):12 10.1186/1752-1505-7-12 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Taira BR, Cherian MN, Yakandawala H, Kesavan R, Samarage SM, DeSilva M. Survey of Emergency and Surgical Capacity in the Conflict-Affected Regions of Sri Lanka. World Journal of Surgery. 2009:1–5. . [DOI] [PubMed] [Google Scholar]
- 163.Taha AA, Westlake C. Palestinian nurses' lived experiences working in the occupied West Bank. International Nursing Review. 2017;64(1):83–90. 10.1111/inr.12332 . Language: English. Entry Date: 20170216. Revision Date: 20170216. Publication Type: Article. Journal Subset: Continental Europe. [DOI] [PubMed] [Google Scholar]
- 164.Stone-Brown K. Syria: a healthcare system on the brink of collapse. BMJ. 2013;347:f7375 10.1136/bmj.f7375 . [DOI] [PubMed] [Google Scholar]
- 165.Squires A, Sindi A, Fennie K. Health system reconstruction: perspectives of Iraqi physicians. Global Public Health. 2010;5(6):561–77. 10.1080/17441690903473246 . Language: English. Entry Date: 20110107. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Squires A, Sindi A, Fennie K. Reconstructing a health system and a profession: priorities of Iraqi nurses in the Kurdish region. Advances in Nursing Science. 2006;29(1):55–68. . Language: English. Entry Date: 20060804. Revision Date: 20150818. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 167.Southall D. Armed conflict women and girls who are pregnant, infants and children; a neglected public health challenge. What can health professionals do? Early Human Development. 2011;87(11):735–42. . Language: English. Entry Date: 20130830. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 168.Sousa C, Hagopianb A. Conflict, health care and professional perseverance: A qualitative study in the West Bank. Global Public Health. 2011;6(5):520–33. . [DOI] [PubMed] [Google Scholar]
- 169.Solberg K. Gaza's health and humanitarian crisis. The Lancet. 2014;384(9941):389–90. . [DOI] [PubMed] [Google Scholar]
- 170.Slagstad K. Even wars have rules. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2016;136(10):891 . [DOI] [PubMed] [Google Scholar]
- 171.Skirtz A. Whither the social workers? why the silence? Social Work. 2008;53(3):286–8. . [DOI] [PubMed] [Google Scholar]
- 172.Siriwardhana C, Adikari A, Bortel T, McCrone P, Sumathipala A. An intervention to improve mental health care for conflict-affected forced migrants in low-resource primary care settings: a WHO MhGAP-based pilot study in Sri Lanka (COM-GAP study). Trials [Internet]. 2013; 14:[423 p.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/844/CN-01119844/frame.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sinha S, David S, Gerdin M, Roy N. Vulnerabilities of Local Healthcare Providers in Complex Emergencies: Findings from the Manipur Micro-level Insurgency Database 2008–2009. PLoS Currents. 2013;(APR 2013) (no pagination)(ecurrents.dis.397bcdc6602b84f9677fe49ee283def7). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Singh JA, DePellegrin TL. Images of war and medical ethics: physicians should not permit filming of their patients without consent. BMJ: British Medical Journal (International Edition). 2003;326(7393):774–5. . Language: English. Entry Date: 20030613. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Simunovic VJ. Health care in Bosnia and Herzegovina before, during, and after 1992–1995 war: a personal testimony. Conflict & Health [Electronic Resource]. 2007;1:7 10.1186/1752-1505-1-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ghaleb S, Mukwege DM, Roberts R, Sulkowicz KJ, Vlassov VV. Protect Syria's doctors: an open letter to world leaders. Philadelphia, Pennsylvania: Lancet; 2016. p. 1056–. [DOI] [PubMed] [Google Scholar]
- 177.Gilbert M. Protect health personnel in war zones!. [Norwegian] Beskytt helsepersonell i krigssoner! Tidsskrift for den Norske Laegeforening. 2002;122(9):892 . [PubMed] [Google Scholar]
- 178.Gluncic V, Pulanic D, Prka M, Marusic A, Marusic M. Curricular and extracurricular activities of medical students during war, Zagreb University School of Medicine, 1991–1995. Academic Medicine. 2001;76(1):82–7. 10.1097/00001888-200101000-00022 . [DOI] [PubMed] [Google Scholar]
- 179.Gold S. Caring for Gaza's victims of war. Nursing Standard. 2009;23(26):64–. . Language: English. Entry Date: 20090417. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 180.Goldberger JJ, Popp RL, Zipes DP. Israel-Gaza conflict. The Lancet. 2014;384(9943):577–8. . [DOI] [PubMed] [Google Scholar]
- 181.Goniewicz K, Goniewicz M, Pawlowski W. [Protection of medical personnel in contemporary armed conflicts]. Wiadomosci Lekarskie. 2016;69(2 Pt 2):280–4. . [PubMed] [Google Scholar]
- 182.Gordon JS. Healing the wounds of war: Gaza Diary. Alternative Therapies in Health and Medicine. 2006;12(1):18–21. . [PubMed] [Google Scholar]
- 183.Gulland A. Attacks on health workers in conflict areas should be documented for advocacy purposes, conference hears. BMJ (Clinical research ed). 2013;347 (no pagination)(f7259). . [DOI] [PubMed] [Google Scholar]
- 184.Gulland A. Doctors urge Syrian government to allow them access to patients. BMJ (Clinical research ed). 2013;347:f5698 . [DOI] [PubMed] [Google Scholar]
- 185.Gulland A. Medical students perform operations in Syria's depleted health system. BMJ (Clinical research ed). 2013;346 (no pagination)(f3107). . [DOI] [PubMed] [Google Scholar]
- 186.Gulland A. WHO condemns attacks on healthcare workers in Yemen. BMJ (Online). 2015;350 (no pagination)(h2914). . [DOI] [PubMed] [Google Scholar]
- 187.Haar RJ, Footer KH, Singh S, Sherman SG, Branchini C, Sclar J, et al. Measurement of attacks and interferences with health care in conflict: validation of an incident reporting tool for attacks on and interferences with health care in eastern Burma. Conflict & Health [Electronic Resource]. 2014;8(1):23 10.1186/1752-1505-8-23 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Haber Y, Palgi Y, Hamama-Raz Y, Shrira A, Ben-Ezra M. Predictors of Professional Quality of Life among Physicians in a Conflict Setting: The Role of Risk and Protective Factors. Israel Journal of Psychiatry & Related Sciences. 2013;50(3):174–80. Language: English. Entry Date: 10.1038/ki.2009.504 Revision Date: 20150923. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 189.Hagopian A, Ratevosian J, Deriel E. Gathering in groups: Peace advocacy in health professional associations. Academic Medicine. 2009;84(11):1485 . [DOI] [PubMed] [Google Scholar]
- 190.Hallam R. Response to Syria's health crisis. The Lancet. 2013;382(9893):679–80. . [DOI] [PubMed] [Google Scholar]
- 191.Hameed Y. Dispatch from the medical front: A doctor and a grenade. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2009;181(3–4):E40 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Hampton T. Health care under attack in Syrian conflict. JAMA. 2013;310(5):465–6. 10.1001/jama.2013.69374 . [DOI] [PubMed] [Google Scholar]
- 193.Hathout L. The right to practice medicine without repercussions: ethical issues in times of political strife. Philosophy, ethics, and humanities in medicine: PEHM. 2012;7:11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.O’Connor K. Nursing Ethics and the 21st-Century Armed Conflict. Journal of Transcultural Nursing. 2017;28(1):6–14. 10.1177/1043659615620657 . Language: English. Entry Date: 20161208. Revision Date: 20161216. Publication Type: Article. Journal Subset: Core Nursing. [DOI] [PubMed] [Google Scholar]
- 195.O'Brien DP, Mills C, Hamel C, Ford N, Pottie K. Universal access: the benefits and challenges in bringing integrated HIV care to isolated and conflict affected populations in the Republic of Congo. Conflict & Health [Electronic Resource]. 2009;3:1 10.1186/1752-1505-3-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.O'Brien E. Bahrain: continuing imprisonment of doctors. Lancet. 2011;378(9798):1203–5. 10.1016/S0140-6736(11)61353-6 . [DOI] [PubMed] [Google Scholar]
- 197.Oulton JA. Inside view. Armed conflict: consequences and challenges for nurses. International Nursing Review. 2003;50(2):72–. . Language: English. Entry Date: 20030725. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Continental Europe. [DOI] [PubMed] [Google Scholar]
- 198.Simetka O, Reilley B, Joseph M, Collie M, Leidinger J. Obstetrics during Civil War: six months on a maternity ward in Mallavi, northern Sri Lanka. Medicine, conflict, and survival. 2002;18(3):258–70. . [DOI] [PubMed] [Google Scholar]
- 199.Sidel VW, Levy BS. Commentary: Guard against war: An expanded role for public health. European Journal of Public Health. 2006;16(3):232 . [DOI] [PubMed] [Google Scholar]
- 200.Physicians Sibbald B., health facilities targeted in war-torn Syria. CMAJ: Canadian Medical Association Journal. 2013;185(9):755–6. 10.1503/cmaj.109-4492 . Language: English. Entry Date: 20130927. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Shetty P. Protecting health-care workers in the firing line. Lancet. 2013;382(9909):e41–2. 10.1016/s0140-6736(13)62627-6 . [DOI] [PubMed] [Google Scholar]
- 202.Sheik M, Gutierrez MI, Bolton P, Spiegel P, Thieren M, Burnham G. Deaths among humanitarian workers. British Medical Journal. 2000;321(7254):166–8. 10.1111/1346-8138.14697 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Sheather J. The Sri Lankan doctors and the challenge for medical leadership. Indian journal of medical ethics. 2009;6(4):179–81. . [DOI] [PubMed] [Google Scholar]
- 204.Sharony Z, Eldor L, Klein Y, Ramon Y, Rissin Y, Berger Y, et al. The role of the plastic surgeon in dealing with soft tissue injuries: Experience from the second israel-lebanon war, 2006. Annals of Plastic Surgery. 2009;62(1):70–4. . [DOI] [PubMed] [Google Scholar]
- 205.Sharma GK, Osti B, Sharma B. Physicians persecuted for ethical practice in Nepal. Lancet. 2002;359(9316):1519 . [DOI] [PubMed] [Google Scholar]
- 206.Shanks L, Schull MJ. Rape in war: The humanitarian response. Cmaj. 2000;163(9):1152–6. 10.1094/PDIS.2000.84.11.1171 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Shamia NA, Thabet AAM, Vostanis P. Exposure to war traumatic experiences, post-traumatic stress disorder and post-traumatic growth among nurses in Gaza. Journal of Psychiatric & Mental Health Nursing. 2015;22(10):749–55. 10.1111/jpm.12264 . Language: English. Entry Date: 20151218. Revision Date: 20161130. Publication Type: Article. Journal Subset: Core Nursing. [DOI] [PubMed] [Google Scholar]
- 208.Shamia NA, Mousa Thabet AA, Vostanis P. 'Agencies need to prepare staff for trauma of war zone work'. Nursing Times. 2014;110(42):11–. . Language: English. Entry Date: 20141030. Revision Date: 20150712. Publication Type: Journal Article. [Google Scholar]
- 209.Shamai M. Using social constructionist thinking in training social workers living and working under threat of political violence. Social Work. 2003;48(4):545–55. sw/48.4.545. . Language: English. Entry Date: 20050425. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 210.Serle J, Fleck F. Keeping health workers and facilities safe in war. Bulletin of the World Health Organization. 2012;90(1):8–9. 10.2471/BLT.12.030112 . Language: English. Entry Date: 20120221. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Hawkes N. Attacks on doctors rise as rules of conduct in conflict zones are abandoned. BMJ (Clinical research ed). 2012;344:e2973 . [DOI] [PubMed] [Google Scholar]
- 212.Hays KE, Prepas R. The Professionalization of International Disaster Response: It Is Time for Midwives to Get Ready. Journal of Midwifery & Women's Health. 2015;60(4):348–59. 10.1111/jmwh.12339 . Language: English. Entry Date: 20150910. Revision Date: 20160630. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 213.Heisler M, Baker E, McKay D. Attacks on Health Care in Syria—Normalizing Violations of Medical Neutrality? New England Journal of Medicine. 2015;373(26):2489–91. 10.1056/NEJMp1513512 ; PubMed Central PMCID: PMCNIHMS759291 [Available on 12/24/16]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Hendel T, Fish M, Aboudi S. Strategies used by hospital nurses to cope with a national crisis: a manager's perspective. International nursing review. 2000;47(4):224–31. . [DOI] [PubMed] [Google Scholar]
- 215.Herbermann JD, Fleck F. Attacks depriving people of urgently needed health care. Bulletin of the World Health Organization. 2017;95(1):6–7. . Language: English. Entry Date: 20170124. Revision Date: 20170125. Publication Type: Article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Hinsenkamp M. Violence against healthcare workers. International Orthopaedics. 2013;37(12):2321–2. 10.1007/s00264-013-2129-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Holt E. Ukraine: Health workers fear for their safety. The Lancet. 2014;384(9945):735 . [DOI] [PubMed] [Google Scholar]
- 218.Hurley R. Who cares for the nine million displaced people of Syria? BMJ. 2013;347:f7374 10.1136/bmj.f7374 . [DOI] [PubMed] [Google Scholar]
- 219.Huss E, Sarid O, Cwikel J. Using art as a self-regulating tool in a war situation: a model for social workers. Health & Social Work. 2010;35(3):201–9. . Language: English. Entry Date: 20101029. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 220.Iacobucci G. Syrian doctors appeal to President Obama for help. BMJ (Clinical research ed). 2016;354:i4458 . [DOI] [PubMed] [Google Scholar]
- 221.Jabbour S. Healing and peace making in the Middle East: challenges for doctors. Lancet. 2005;365 North American Edition(9466):1211–2. . Language: English. Entry Date: 20050923. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 222.Izzeldin IM, Nagi EA. Neurological services in Darfur: A deprived rural community in a tropical zone affected by ongoing armed conflict. Journal of the Royal College of Physicians of Edinburgh. 2008;38(1):5–11. . [Google Scholar]
- 223.Jaffe E, Aviel E, Aharonson-Daniel L, Nave M, Knobler HY. Factors influencing the willingness of volunteer paramedics to re-volunteer in a time of war. Israel Medical Association Journal. 2010;12(9):526–30. . [PubMed] [Google Scholar]
- 224.Selvakone M. Doctors in detention and the Hippocratic Oath. CMAJ Canadian Medical Association Journal. 2009;181(10):E243 10.1503/cmaj.091527 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Saunders S, London L. Health professionals should be speaking out about the victimisation of doctors in Bahrain. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2012;102(3 Pt 1):112 . [DOI] [PubMed] [Google Scholar]
- 226.Santa Barbara J, MacQueen G. Peace through health: key concepts. Lancet. 2004;364(9431):384–6. 10.1016/S0140-6736(04)16729-9 . [DOI] [PubMed] [Google Scholar]
- 227.Sankari A, Atassi B, Sahloul MZ. Syrian field hospitals: A creative solution in urban military conflict combat in Syria. Avicenna Journal of Medicine. 2013;3(3):84–6. 10.4103/2231-0770.118467 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Sambunjak D, Kovacic L. Guard against the oblivion: A role of public health in war. European Journal of Public Health. 2006;16(3):231–2. . [DOI] [PubMed] [Google Scholar]
- 229.Salvage J. Blessed are the peacemakers. Nursing Times. 2002;98(34):18–. . Language: English. Entry Date: 20030131. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Core Nursing. [Google Scholar]
- 230.Salih AM, Ahmed JM, Mohamed JF, Alfaki MM. Reinventing the political role of health professionals in conflict prevention & reconciliation: the Sudanese model. Medicine, Conflict & Survival. 2016;32(2):153–64. 10.1080/13623699.2016.1239172 . [DOI] [PubMed] [Google Scholar]
- 231.Sahloul MZ, Monla-Hassan J, Sankari A, Kherallah M, Atassi B, Badr S, et al. War is the Enemy of Health. Pulmonary, Critical Care, and Sleep Medicine in War-Torn Syria. Annals of the American Thoracic Society. 2016;13(2):147–55. 10.1513/AnnalsATS.201510-661PS . Language: English. Entry Date: 20160826. Revision Date: 20170104. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 232.Saben J. Medical training under fire. Western Journal of Medicine. 2000;173(3):213–4. 10.1136/ewjm.173.3.213 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Jargin SV. Nursing and Security in Iraqi hospitals: some problems can be solved without foreign help. International journal of nursing practice. 2009;15(3):129–30. . [DOI] [PubMed] [Google Scholar]
- 234.Jayawardene W, Youssefagha A, Lajoie S, Torabi M. Psychological distress among nurses caring for victims of war in sri lanka. Disaster Medicine & Public Health Preparedness. 2013;7(3):278–86. 10.1001/dmp.2011.36 . Language: English. Entry Date: 20141031. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 235.Jefee-Bahloul H, Barkil-Oteo A, Pless-Mulloli T, Fouad FM. Mental health in the Syrian crisis: Beyond immediate relief. The Lancet. 2015;386(10003):1531 . [DOI] [PubMed] [Google Scholar]
- 236.Johna S. The anatomy of crime: Physicians under the oppressive regime of Saddam Hussein. AMHA—Acta Medico-Historica Adriatica. 2009;7(2):303–8. . [PubMed] [Google Scholar]
- 237.Johnson S. Doctors in the cross hairs. Newsweek. 2006;147(2):36 . [PubMed] [Google Scholar]
- 238.Johnson TD. A glimpse of emergency care and strife in kosovo: One emergency nurse's experience. Journal of Emergency Nursing. 2005;31(1):124–8. . [DOI] [PubMed] [Google Scholar]
- 239.Jones A, Howard N, Legido-Quigley H. Feasibility of health systems strengthening in South Sudan: A qualitative study of international practitioner perspectives. BMJ Open. 2015;5 (12) (no pagination)(e009296). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Kassem M. A Syrian neurosurgeon's journey. Surgical Neurology International. 2016;7 (1) (no pagination)(6) 10.1016/0006-291x(75)90518-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Rubenstein LS, Bittle MD. Responsibility for protection of medical workers and facilities in armed conflict. Lancet. 2010;375 North American Edition(9711):329–40. 10.1016/S0140-6736(09)61926-7 . Language: English. Entry Date: 20100312. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 242.Rorie JA. War by any other name. Journal of midwifery & women's health. 2003;48(4):306 . [DOI] [PubMed] [Google Scholar]
- 243.Richard AJ, Lee CI, Richard MG, Oo EK, Lee T, Stock L. Essential trauma management training: addressing service delivery needs in active conflict zones in eastern Myanmar. Human Resources for Health [Electronic Resource]. 2009;7:19 10.1186/1478-4491-7-19 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Reiss-Koncar D. Bandaging Baghdad. Revolution: The Journal for RNs & Patient Advocacy. 2003;4(4):18–25. . Language: English. Entry Date: 20040227. Revision Date: 20150711. Publication Type: Journal Article. [PubMed] [Google Scholar]
- 245.Redwood-Campbell LJ, Sekhar SN, Persaud CR. Health care workers in danger zones: a special report on safety and security in a changing environment. Prehospital & Disaster Medicine. 2014;29(5):503–7. 10.1017/S1049023X14000934 . Language: English. Entry Date: 20150923. Revision Date: 20161001. Publication Type: journal article. Journal Subset: Allied Health. [DOI] [PubMed] [Google Scholar]
- 246.Qirbi N, Ismail SA. Health system functionality in a low-income country in the midst of conflict: the case of Yemen. Health Policy & Planning. 2017;32(6):911–22. 10.1093/heapol/czx031 . Language: English. Entry Date: In Process. Revision Date: 20170613. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 247.Pruginin I, Segal-Engelchin D, Isralowitz R, Reznik A. Shared War reality effects on the professional quality of life of mental health professionals. Israel Journal of Health Policy Research. 2016;5 (1) (no pagination)(17). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Poudyal AK, Jimba M, Wakai S. Difficulties of peace-building in Nepal. CMAJ Canadian Medical Association Journal. 2005;172(13):1663; author reply -4. 10.1503/cmaj.1050013 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Pollack RN. Doctors in conflict. Lancet. 2003;362(9392):1327 . [DOI] [PubMed] [Google Scholar]
- 250.Katz IT, Wright AA. Collateral damage—Medecins san Frontieres leaves Afghanistan and Iraq. New England Journal of Medicine. 2004;351(25):2571–3. . [DOI] [PubMed] [Google Scholar]
- 251.Kertcher C. Grassroots medical peace building: Training Palestinian physicians in Israel. Medicine, Conflict and Survival. 2014;30(3):190–212. . [DOI] [PubMed] [Google Scholar]
- 252.Kevat D, Lander F, Loff B. The growing threat to medical independence in conflict zones. The Lancet. 2012;379(9814):e31–e2. . [DOI] [PubMed] [Google Scholar]
- 253.Khan H, Al-Saadi N. Can Health Professionals Inform Policy in Regions of Conflict? World Medical and Health Policy. 2016;8(2):208–9. . [Google Scholar]
- 254.Kibris A, Metternich N. The flight of white-collars: Civil conflict, availability of medical service providers and public health. Social Science and Medicine. 2016;149:93–103. . [DOI] [PubMed] [Google Scholar]
- 255.Kienzler H. The social life of psychiatric practice: Trauma in postwar Kosova. Medical Anthropology: Cross Cultural Studies in Health and Illness. 2012;31(3):266–82. . [DOI] [PubMed] [Google Scholar]
- 256.Koren D, Caspi Y, Leiba R, Bloch D, Vexler B, Klein E. Acute stress reactions among medical and non-medical personnel in a general hospital under missile attacks. Depression and Anxiety. 2009;26(2):123–8. . [DOI] [PubMed] [Google Scholar]
- 257.Kuruppuarachchi KA, Williams SS. Conflict in Sri Lanka. Doctors can influence people and promote peace. BMJ (Clinical research ed). 2002;324(7333):361 . [PubMed] [Google Scholar]
- 258.Nickerson JW. Ensuring the security of health care in conflict settings: An urgent global health concern. Cmaj. 2015;187(11):E347–E8. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Nicholas B. Is war necessary? The American journal of nursing. 2003;103(2):15 . [DOI] [PubMed] [Google Scholar]
- 260.Namakula J, Witter S. Living through conflict and post-conflict: experiences of health workers in northern Uganda and lessons for people-centred health systems. Health Policy & Planning. 2014;29(suppl_2):ii6–ii14. 10.1093/heapol/czu022 . Language: English. Entry Date: 20150923. Revision Date: 20160817. Publication Type: journal article. Supplement Title: Sep2014 Supplement. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Murad MK, Husum H. Trained lay first responders reduce trauma mortality: a controlled study of rural trauma in Iraq. Prehospital & Disaster Medicine. 2010;25(6):533–9. . Language: English. Entry Date: 20110401. Revision Date: 20160216. Publication Type: journal article. [DOI] [PubMed] [Google Scholar]
- 262.Mullany LC, Lee CI, Paw P, Shwe Oo EK, Maung C, Kuiper H, et al. The MOM Project: delivering maternal health services among internally displaced populations in eastern Burma. Reproductive Health Matters. 2008;16(31):44–56. . Language: English. Entry Date: 20090116. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 263.Mullan Z. Medical neutrality: Resetting the moral compass. The Lancet Global Health. 2016;4(4):e215 . [DOI] [PubMed] [Google Scholar]
- 264.Mowafi H, Hariri M, Alnahhas H, Ludwig E, Allodami T, Mahameed B, et al. Results of a Nationwide Capacity Survey of Hospitals Providing Trauma Care in War-Affected Syria. JAMA Surgery. 2016;151(9):815–22. 10.1001/jamasurg.2016.1297 . Language: English. Entry Date: 20170701. Revision Date: 20170701. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 265.Moszynski P. Only one doctor is left working in rebel controlled Nuba Mountains. BMJ (Clinical research ed). 2013;346 (no pagination)(f759). . [DOI] [PubMed] [Google Scholar]
- 266.Moszynski P. Sudanese doctor describes "hell on earth" in Darfur. BMJ. 2008;337:a951 10.1136/bmj.a951 . [DOI] [PubMed] [Google Scholar]
- 267.Morrison C. A symphony of frogs at night. The Canadian nurse. 2002;98(2):10–1. . [PubMed] [Google Scholar]
- 268.Miyake S, Speakman EM, Currie S, Howard N. Community midwifery initiatives in fragile and conflict-affected countries: a scoping review of approaches from recruitment to retention. Health Policy & Planning. 2017;32(1):21–33. 10.1093/heapol/czw093 . Language: English. Entry Date: In Process. Revision Date: 20170627. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 269.Missmahl I, Kluge U, Bromand Z, Heinz A. Teaching psychiatry and establishing psychosocial services—lessons from Afghanistan. European Psychiatry. 2012;27(SUPPL.2):S76–S80. . [DOI] [PubMed] [Google Scholar]
- 270.Palgi Y, Ben-Ezra M, Shrira A. The effect of prolonged exposure to war-related stress among hospital personnel with different affect types: lessons from the Second Lebanon War and the Gaza "Cast Lead" operation. European Journal of Psychotraumatology. 2012;3 10.3402/ejpt.v3i0.7165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Palgi Y, Ben-Ezra M, Langer S, Essar N. The effect of prolonged exposure to war stress on the comorbidity of PTSD and depression among hospital personnel. Psychiatry Research. 2009;168(3):262–4. . [DOI] [PubMed] [Google Scholar]
- 272.Parfitt T. Chechen doctors battle to treat the republic's ills. Lancet. 2005;365(9472):1675–976. . [DOI] [PubMed] [Google Scholar]
- 273.Parish C. The price of war. Nursing Standard. 2002;17(14/15):18–20. . Language: English. Entry Date: 20030411. Revision Date: 20150711. Publication Type: Journal Article. [PubMed] [Google Scholar]
- 274.Pincock S. Salam Ismael. Lancet. 2006;368(9533):359 10.1016/S0140-6736(06)69094-6 . [DOI] [PubMed] [Google Scholar]
- 275.The war in the Gulf: firsthand accounts from emergency nurses. JEN: Journal of Emergency Nursing. 1991;17(5):27A–47A. . Language: English. Entry Date: 19920201. Revision Date: 20150712. Publication Type: Journal Article. Journal Subset: Core Nursing. [Google Scholar]
- 276.Labat F, Sharma A. Qualitative study exploring surgical team members' perception of patient safety in conflict-ridden Eastern Democratic Republic of Congo. BMJ Open. 2016;6 (4) (no pagination)(e009379). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Lachter J, Beiran I, Wakai S, Segall M. Physicians for peace (multiple letters). Lancet. 2000;355(9212):1365–6. 10.3791/58067 . [DOI] [PubMed] [Google Scholar]
- 278.Lamberg L. Psychiatrists strive to help children heal mental wounds from war and disasters. JAMA—Journal of the American Medical Association. 2008;300(6):642–3. . [DOI] [PubMed] [Google Scholar]
- 279.Lavi T, Nuttman-Shwartz O, Dekel R. Therapeutic Intervention in a Continuous Shared Traumatic Reality: An Example from the Israeli-Palestinian Conflict. British Journal of Social Work. 2017;47(3):919–35. 10.1093/bjsw/bcv127 . Language: English. Entry Date: 20170616. Revision Date: 20170616. Publication Type: Article. Journal Subset: Allied Health. [DOI] [Google Scholar]
- 280.Lee CI, Smith LS, Shwe Oo EK, Scharschmidt BC, Whichard E, Kler T, et al. Internally displaced human resources for health: villager health worker partnerships to scale up a malaria control programme in active conflict areas of eastern Burma. Global Public Health. 2009;4(3):229–41. 10.1080/17441690802676360 . Language: English. Entry Date: 20090731. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 281.Lee PPS. An open letter from Concerned Medical Students on Iraq [6]. Cmaj. 2003;168(9):1115 . [PMC free article] [PubMed] [Google Scholar]
- 282.Leighton M. We must challenge war [8]. British Medical Journal. 2007;334(7593):550 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Lev-Wiesel R, Goldblatt H, Eisikovits Z, Admi H. Growth in the shadow of the war: the case of social workers and nurses working in a shared war reality. British Journal of Social Work. 2009;39(6):1154–74. doi: bjsw/bcn021 . Language: English. Entry Date: 20091106. Revision Date: 20150820. Publication Type: Journal Article. [Google Scholar]
- 284.Levy BS, Sidel VW. How academic medicine can contribute to peace-building efforts worldwide. Academic Medicine. 2009;84(11):1487 . [DOI] [PubMed] [Google Scholar]
- 285.Lim AG, Stock L, Shwe Oo EK, Jutte DP. Trauma and mental health of medics in eastern Myanmar's conflict zones: a cross-sectional and mixed methods investigation. Conflict & Health [Electronic Resource]. 2013;7(1):15 10.1186/1752-1505-7-15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Lindsay J. The impact of the 2nd Intifada: an exploration of the experiences of Palestinian psychosocial counselors and social workers. Illness, Crisis & Loss. 2007;15(2):137–53. . Language: English. Entry Date: 20070824. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 287.Mackay B. MDs mostly mum on Iraq. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2003;168(10):1307 . [PMC free article] [PubMed] [Google Scholar]
- 288.MacQueen G, Santa-Barbara J. Peace building through health initiatives. British Medical Journal. 2000;321(7256):293–6. 10.3390/children5120162 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.MacQueen G, Santa-Barbara J, Neufeld V, Yusuf S, Horton R. Health and peace: Time for a new discipline. Lancet. 2001;357(9267):1460–1. . [DOI] [PubMed] [Google Scholar]
- 290.Madsen AM, Pope R, Samuels A, Margolis CZ. Foreign students' experience during a time of war. Israel Medical Association Journal: Imaj. 2013;15(3):143–7. . [PubMed] [Google Scholar]
- 291.Magidson JF, Lejuez CW, Kamal T, Blevins EJ, Murray LK, Bass JK, et al. Adaptation of community health worker-delivered behavioral activation for torture survivors in Kurdistan, Iraq. Glob Ment Health. 2015;2 10.1017/gmh.2015.22 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Mahn M, Maung C, Shwe Oo EK, Smith L, Lee CI, Whichard E, et al. Multi-level partnership to promote health services among internally displaced in eastern Burma. Global Public Health. 2008;3(2):165–86. . [DOI] [PubMed] [Google Scholar]
- 293.Mahomed Z, Motara F, Bham A. Humanitarian Medical Response to the Syrian Arab Republic (April 7, 2013 to April 23, 2013). Prehospital & Disaster Medicine. 2016;31(1):114–6. 10.1017/S1049023X15005518 . Language: English. Entry Date: 20170228. Revision Date: 20170228. Publication Type: journal article. Journal Subset: Allied Health. [DOI] [PubMed] [Google Scholar]
- 294.Malke B. Ethical dilemmas for physicians in time of war. Israel Medical Association Journal: Imaj. 2010;12(3):172–3. . [PubMed] [Google Scholar]
- 295.Mansoor GF, Hashemy P, Gohar F, Wood ME, Ayoubi SF, Todd CS. Midwifery retention and coverage and impact on service utilisation in Afghanistan. Midwifery. 2013;29(10):1088–94. 10.1016/j.midw.2013.07.021 . Language: English. Entry Date: 20131002. Revision Date: 20150819. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 296.Marchbein D. Humanitarian surgery: a call to action for anesthesiologists. Anesthesiology. 2013;119(5):1001–2. 10.1097/ALN.0b013e3182a950fb . [DOI] [PubMed] [Google Scholar]
- 297.Markestad T. Physicians in war. [Norwegian]Leger i krig. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2009;129(7):650 . [DOI] [PubMed] [Google Scholar]
- 298.Marton R. Human rights violations during Israel's attack on the Gaza Strip: 27 December 2008 to 19 January 2009. Global Public Health. 2011;6(5):560–9. . [DOI] [PubMed] [Google Scholar]
- 299.Mason D. Nursing in a war zone. Nursing Standard. 2006;20(50):62–3. . Language: English. Entry Date: 20061117. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 300.Mason P, Ghareeb K. Iraqi pharmacists contend with violence, murder and uncertainty… but in northern Iraq the future looks brighter. Pharmaceutical Journal. 2007;279(7480):624 . [Google Scholar]
- 301.McQueen KA, Burkle FM Jr, Al-Gobory ET, Anderson CC. Maintaining baseline, corrective surgical care during asymmetrical warfare: a case study of a humanitarian mission in the safe zone of a neighboring country. Prehospital and disaster medicine: the official journal of the National Association of EMS Physicians and the World Association for Emergency and Disaster Medicine in association with the Acute Care Foundation. 2007;22(1):3–7; discussion 8. . [DOI] [PubMed] [Google Scholar]
- 302.Mihajlovic I, Vagenhofer B. Care for the wounded at Vukovar Medical Center: New task for two general practitioners. Croatian Medical Journal. 2011;52(1):95–9. . [Google Scholar]
- 303.Miles SH. Medical ethics and the interrogation of Guantanamo 063. American Journal of Bioethics. 2007;7(4):5–11. . Language: English. Entry Date: 20080215. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 304.Patel P, Gibson-Fall F, Sullivan R, Irwin R. Documenting attacks on health workers and facilities in armed conflicts. Bulletin of the World Health Organization. 2017;95(1):79–81. 10.2471/BLT.15.168328 . Language: English. Entry Date: 20170124. Revision Date: 20170125. Publication Type: Article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Patterson V, Swinfen P, Swinfen R, Azzo E, Taha H, Wootton R. Supporting hospital doctors in the Middle East by email telemedicine: Something the industrialized world can do to help. Journal of Medical Internet Research. 2007;9(4):e30 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Pedersen DM, Pedersen KJ, Santitamrongpan V. The burmese medic: An international physician assistant analogue. Journal of Physician Assistant Education. 2012;23(3):51–5. . [PubMed] [Google Scholar]
- 307.Pellegrino ED, Pellegrino ED. Medical ethics suborned by tyranny and war. Chicago, Illinois: American Medical Association; 2004. p. 1505–6. [DOI] [PubMed] [Google Scholar]
- 308.Penfold R, Ali M. Building medical education and research capacity in areas of conflict and instability: Experiences of the OxPal Medlink in the occupied Palestinian territories. Medicine, Conflict and Survival. 2014;30(3):166–74. . [DOI] [PubMed] [Google Scholar]
- 309.Petersen RB. [The wars in Gaza and the objectivity]. [Norwegian]Krigen i Gaza og objektivitet. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2009;129(21):2263–4. . [DOI] [PubMed] [Google Scholar]
- 310.Wick L, Hassan S. No safe place for childbirth: women and midwives bearing witness, Gaza 2008–09. Reproductive Health Matters. 2012;20(40):7–15. 10.1016/S0968-8080(12)40648-6 . Language: English. Entry Date: 20121226. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 311.Maglajlic RA. A new dawn: the changing face of mental health services in Bosnia and Herzegovina. Mental Health & Learning Disabilities Care. 2001;4(12):401–4. . Language: English. Entry Date: 20011109. Revision Date: 20150818. Publication Type: Journal Article. [Google Scholar]
- 312.Ahmad K. After years of war and misrule, Kabul struggles to rebuild. Lancet. 2003;362(9384):622–3. . [DOI] [PubMed] [Google Scholar]
- 313.Ahmad K. Warlords and bandits slow Afghanistan's efforts to rebuild: Attacks drive relief workers from some areas. Lancet. 2003;362(9385):710–1. . [DOI] [PubMed] [Google Scholar]
- 314.Akl EA, El-Asmar K, Maroun N, Adib SM, Khater-Menassa B. Did the post war repatriation of Lebanese physicians drive recent Lebanese medical graduates to emigrate? An observational study. BMC Health Services Research. 2008;8:195–. . Language: English. Entry Date: 20100730. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Akunjee M, Ali A. Healthcare under sanctions in Iraq: an elective experience. Medicine, conflict, and survival. 2002;18(3):249–57. . [DOI] [PubMed] [Google Scholar]
- 316.Al Hilfi TK, Lafta R, Burnham G. Health services in Iraq. The Lancet. 2013;381(9870):939–48. . [DOI] [PubMed] [Google Scholar]
- 317.Alakija P. The ravages of war. CMAJ Canadian Medical Association Journal. 2000;163(9):1148–9. . [PMC free article] [PubMed] [Google Scholar]
- 318.Al-Saffar S. Integrating rehabilition of torture victims into the public health of Iraq. Torture: quarterly journal on rehabilitation of torture victims and prevention of torture. 2007;17(2):156–68. . [PubMed] [Google Scholar]
- 319.Ariel S, Keith D, Martinez-Ortiz D, Prosky P, Shi L, Tiurean A, et al. The birth of family therapists: The kosova systemic family therapy training program. Journal of Family Psychotherapy. 2014;25(3):225–45. . [Google Scholar]
- 320.Armstrong J, Ager A. Physiotherapy in Afghanistan: An analysis of current challenges. Disability and Rehabilitation. 2006;28(5):315–22. . [DOI] [PubMed] [Google Scholar]
- 321.Atun RA, Kyratsis I, Jelic G, Rados-Malicbegovic D, Gurol-Urganci I. Diffusion of complex health innovations—implementation of primary health care reforms in Bosnia and Herzegovina. Health Policy & Planning. 2007;22(1):28–39. 10.1093/heapol/czl031 . [DOI] [PubMed] [Google Scholar]
- 322.Aziz C, Aziz C. Struggling to rebuild Iraq's health-care system. War, sanctions, and mismanagement have left health system in shambles. Lancet. 2003;362 North American Edition(9392):1288–9. . Language: English. Entry Date: 20050128. Revision Date: 20170414. Publication Type: journal article. [DOI] [PubMed] [Google Scholar]
- 323.Baingana F, Mangen PO. Scaling up of mental health and trauma support among war affected communities in northern Uganda: lessons learned. Intervention (15718883). 2011;9(3):291–303. 10.1097/WTF.0b013e32834dfcc3 . Language: English. Entry Date: 20120217. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [Google Scholar]
- 324.Balalian AA, Simonyan H, Hekimian K, Crape B. Adapting continuing medical education for post-conflict areas: assessment in Nagorno Karabagh—a qualitative study. Human Resources for Health. 2014;12(1):39–. 10.1186/1478-4491-12-39 . Language: English. Entry Date: 20150306. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Barbara JS. Medicine, peace, and public policy. Croatian Medical Journal. 2006;47(2):352–5. . [PMC free article] [PubMed] [Google Scholar]
- 326.Beesley M, Cometto G, Pavignani E. From drought to deluge: how information overload saturated absorption capacity in a disrupted health sector. Health policy and planning. 2011;26(6):445–52. . [DOI] [PubMed] [Google Scholar]
- 327.Bender GJ, Kennally K. Implementing a Neonatal Transport System With Simulation in Kosovo. Air Medical Journal. 2016;35(3):126–31. 10.1016/j.amj.2016.01.002 . Language: English. Entry Date: In Process. Revision Date: 20160610. Publication Type: Article. Journal Subset: Allied Health. [DOI] [PubMed] [Google Scholar]
- 328.Witter S, Falisse J-B, Bertone MP, Alonso-Garbayo A, Martins JS, Salehi AS, et al. State-building and human resources for health in fragile and conflict-affected states: exploring the linkages. Human Resources for Health. 2015;13(1):33–. 10.1186/s12960-015-0023-5 . Language: English. Entry Date: 20150923. Revision Date: 20160216. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Bertone MP, Samai M, Edem-Hotah J, Witter S. A window of opportunity for reform in post-conflict settings? The case of Human Resources for Health policies in Sierra Leone, 2002–2012. Conflict & Health [Electronic Resource]. 2014;8:11 10.1186/1752-1505-8-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Bonner P. Aussies nurse East Timor back to health. Australian nursing journal (July 1993). 2000;8(3):20–1. . [PubMed] [Google Scholar]
- 331.Bojaj G, Skeraj F, Czabanowska K, Burazeri G. Level of Competencies of Family Physicians in Kosovo from Different Perspectives. Materia Sociomedica. 2016;28(5):353–6. 10.5455/msm.2016.28.353-356 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Bristol N. Reconstructing Afghanistan's health system. Lancet. 2005;366(9503):2075–6. 10.1016/s0140-6736(05)67871-3 . [DOI] [PubMed] [Google Scholar]
- 333.Budy FC. Policy Options for Addressing Health System and Human Resources for Health Crisis in Liberia Post-Ebola Epidemic. International Journal of MCH & AIDS. 2015;4(2):1–7. . [PMC free article] [PubMed] [Google Scholar]
- 334.Campbell S. Improving quality of primary health care in a Sudanese dispensary. Nursing Standard. 2000;14(19):39–41. . Language: English. Entry Date: 20000401. Revision Date: 20150819. Publication Type: Journal Article. Supplement Title: 2000 Jan 26-Feb 1. Journal Subset: Double Blind Peer Reviewed. [DOI] [PubMed] [Google Scholar]
- 335.Charlés LL. Scaling Up Family Therapy in Fragile, Conflict-Affected States. Family Process. 2015;54(3):545–58. 10.1111/famp.12107 . Language: English. Entry Date: 20150911. Revision Date: 20160831. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 336.Chi PC, Bulage P, Urdal H, Sundby J. Barriers in the delivery of emergency obstetric and neonatal care in post-conflict Africa: Qualitative case studies of Burundi and Northern Uganda. PLoS ONE. 2015;10 (9) (no pagination)(e0139120). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Cometto G, Belgrano E, De Bonis U, Giustetto G, Kiss A, Taliente P, et al. Primary surgery in rural areas of southern Sudan. World journal of surgery. 2012;36(3):556–64. . [DOI] [PubMed] [Google Scholar]
- 338.Crichton M. Midwifery in Somaliland. The practising midwife. 2013;16(10):20, 2–3. . [PubMed] [Google Scholar]
- 339.Crutcher RA, Shannon SE, Clayton J, Duop DM. Sudanese physicians' reintegration programme. Lancet. 2008;372(9641):788–9. 10.1016/S0140-6736(08)61319-7 . [DOI] [PubMed] [Google Scholar]
- 340.Dad Gadi A, Higuchi M, Warnasuriya N, Kawaguchi L, Aoyama A. Medical students' willingness to work in post-conflict areas: A qualitative study in Sri Lanka. Health (1949–4998). 2012;4(10):824–31. 10.4236/health.2012.410127 . Language: English. Entry Date: 20130308. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [Google Scholar]
- 341.De Jong JTVM Komproe IH. Closing the gap between psychiatric epidemiology and mental health in post-conflict situations. Lancet. 2002;359(9320):1793–4. . [DOI] [PubMed] [Google Scholar]
- 342.De Jong K, Kleber RJ. Emergency conflict-related psychosocial interventions in Sierra Leone and Uganda: lessons from Medecins Sans Frontieres. Journal of Health Psychology. 2007;12(3):485–97. 10.1177/1359105307076235 . [DOI] [PubMed] [Google Scholar]
- 343.Devkota B, van Teijlingen E. Demystifying the Maoist barefoot doctors of Nepal. Medicine, conflict, and survival. 2010;26(2):108–23. . [DOI] [PubMed] [Google Scholar]
- 344.Dunleavy K. Physical therapy education and provision in Cambodia: A framework for choice of systems for development projects. Disability and Rehabilitation. 2007;29(11–12):903–20. . [DOI] [PubMed] [Google Scholar]
- 345.Nuttman-Shwartz O, Sternberg R. Social Work in the Context of an Ongoing Security Threat: Role Description, Personal Experiences and Conceptualisation. British Journal of Social Work. 2017;47(3):903–18. 10.1093/bjsw/bcw053 . Language: English. Entry Date: 20170616. Revision Date: 20170616. Publication Type: Article. Journal Subset: Allied Health. [DOI] [Google Scholar]
- 346.Elalem S, Mull J. WORKING IN A WAR ZONE. Nursing Standard. 2011;26(2):64–. . Language: English. Entry Date: 20111021. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 347.Patel P, Cummings R, Roberts B. Exploring the influence of the Global Fund and the GAVI Alliance on health systems in conflict-affected countries. Conflict and Health. 2015;9(1):7 10.1186/s13031-015-0031-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Fehling M, Nelson BD, Ahn R, Eckardt M, Tiernan M, Purcell G, et al. Development of a community-based maternal, newborn and child emergency training package in South Sudan. Public Health. 2013;127(9):797–805. . [DOI] [PubMed] [Google Scholar]
- 349.Fujita N, Zwi AB, Nagai M, Akashi H. A comprehensive framework for human resources for health system development in fragile and post-conflict States. PLoS Medicine. 2011;8(12):e1001146–e. . Language: English. Entry Date: 20120511. Revision Date: 20150711. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Gabba AE. An assessment study on improving nursing education and nursing practice in Sierra Leone with focus on primary health care and health for all beyond 2000. West African Journal of Nursing. 2003;14(2):91–8. . Language: English. Entry Date: 20040514. Revision Date: 20150820. Publication Type: Journal Article. [Google Scholar]
- 351.Goepp JG, Johnson TD, Maddow CL. Challenges and promises for nurse education curriculum development in Kosovo: results of an 'accidental ethnography'. Nurse Education Today. 2008;28(4):419–26. . Language: English. Entry Date: 20080725. Revision Date: 20150819. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 352.Hart LJ, Carr C, Fullerton JT. Task Analysis as a Resource for Strengthening Health Systems. Journal of Midwifery & Women's Health. 2016;61(2):257–62. 10.1111/jmwh.12410 . Language: English. Entry Date: 20160407. Revision Date: 20170301. Publication Type: Article. Journal Subset: Core Nursing. [DOI] [PubMed] [Google Scholar]
- 353.Hasanovic M, Izet P, Avdibegovic E, Kravic N, Moro L, Franciskovic T, et al. Training of bosnia-herzegovina mental health professionals in group analysis as the factor of development of culture of dialogue in the aftermath of the 1992–1995 war. European Psychiatry Conference: 21st European Congress of Psychiatry, EPA. 2013;28(no pagination). .
- 354.Hasanovic M, Herenda S. Post traumatic stress disorder, depression and anxiety among family medicine residents after 1992–95 war in Bosnia and Herzegovina. Psychiatria Danubina. 2008;20(3):277–85. . [PubMed] [Google Scholar]
- 355.Hasanovic M, Morgan S, Oakley S, Pajevic I. EMDR training for bosnia-herzegovina mental health workers in sarajevo as continuity of the building of psychotherapy capacity aftermath the 1992–1995 war. European Psychiatry Conference: 21st European Congress of Psychiatry, EPA. 2013;28(no pagination). . [Google Scholar]
- 356.Hawkes M, Katsuva JP, Masumbuko CK. Use and limitations of malaria rapid diagnostic testing by community health workers in war-torn Democratic Republic of Congo. Malaria Journal. 2009;8 (1) (no pagination)(308). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Woodward A, Fyfe M, Handuleh J, Patel P, Godman B, Leather A, et al. Diffusion of e-health innovations in 'post-conflict' settings: a qualitative study on the personal experiences of health workers. Human Resources for Health. 2014;12(1):22–. 10.1186/1478-4491-12-22 . Language: English. Entry Date: 20150306. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Zafar S, Sikander S, Hamdani SU, Atif N, Akhtar P, Nazir H, et al. The effectiveness of Technology-assisted Cascade Training and Supervision of community health workers in delivering the Thinking Healthy Program for perinatal depression in a post-conflict area of Pakistan—study protocol for a randomized controlled trial. Trials [Internet]. 2016; 17:[188 p.]. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/503/CN-01307503/frame.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Wurie HR, Samai M, Witter S. Retention of health workers in rural Sierra Leone: findings from life histories. Human Resources for Health. 2016;14:1–15. 10.1186/s12960-016-0099-6 . Language: English. Entry Date: In Process. Revision Date: 20170104. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Witter S, Wurie H, Bertone MP. The free health care initiative: how has it affected health workers in Sierra Leone? Health Policy & Planning. 2016;31(1):1–9. 10.1093/heapol/czv006 . Language: English. Entry Date: 20170302. Revision Date: 20170302. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Williams JL, McCarthy B. Observations from a maternal and infant hospital in Kabul, Afghanistan—2003. Journal of Midwifery and Women's Health. 2005;50(4):e31–e5. . [DOI] [PubMed] [Google Scholar]
- 362.Wen LS, Char DM. Existing infrastructure for the delivery of emergency care in post-conflict Rwanda: An initial descriptive study. African Journal of Emergency Medicine. 2011;1(2):57–61. . [Google Scholar]
- 363.Webster PC. Iraq's health system yet to heal from ravages of war. Lancet. 2011;378 North American Edition(9794):863–6. 10.1016/S0140-6736(11)61399-8 . Language: English. Entry Date: 20110930. Revision Date: 20150712. Publication Type: Journal Article. Journal Subset: Biomedical. [DOI] [PubMed] [Google Scholar]
- 364.Warsame A, Handuleh J, Patel P. Prioritization in somali health system strengthening: A qualitative study. International Health. 2016;8(3):204–10. . [DOI] [PubMed] [Google Scholar]
- 365.Varpilah ST, Safer M, Frenkel E, Baba D, Massaquoi M, Barrow G. Rebuilding human resources for health: a case study from Liberia. Human Resources for Health [Electronic Resource]. 2011;9:11 10.1186/1478-4491-9-11 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Vanier VK, VanRooyen MJ, Lis J, Eliades MJ. Post-war Kosovo: part 1. Assessment of prehospital emergency services. Prehospital & Disaster Medicine. 2001;16(4):263–7. . Language: English. Entry Date: 20030627. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 367.Henderson DC, Mollica RF, Tor S, Lavelle J, Culhane MA, Hayden D. Building primary care practitioners' attitudes and confidence in mental health skills in a post-conflict society: a Cambodian example. Journal of Nervous & Mental Disease. 2005;193(8):551–9. 10.1097/01.nmd.0000172869.01711.33 . [DOI] [PubMed] [Google Scholar]
- 368.Herberg P. Nursing, midwifery and allied health education programmes in Afghanistan. International Nursing Review. 2005;52(2):123–33. . Language: English. Entry Date: 20050701. Revision Date: 20150819. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 369.Hexom B, Calvello EJB, Babcock CA, Fowler R, Theodosis C, Sirleaf JA, et al. A model for emergency medicine education in post-conflict Liberia. African Journal of Emergency Medicine. 2012;2(4):143–50. . [Google Scholar]
- 370.Himmler B. Health care diplomacy: the Iraq experience and how it can shape the future. Military medicine. 2009;174(12):xviii–xx. . [PubMed] [Google Scholar]
- 371.Maylin M, Monsuez JJ, Ibata P, Rizet R. Health and war in Congo-Brazzaville [11]. Lancet. 2001;357(9256):640–1. 10.1136/oemed-2020-106432 . [DOI] [PubMed] [Google Scholar]
- 372.Mbanjumucyo G, DeVos E, Pulfrey S, Epino HM. State of emergency medicine in Rwanda 2015: An innovative trainee and trainer model. International Journal of Emergency Medicine. 2015;8 (1) (no pagination)(20). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Medeiros E. Integrating mental health into post-conflict rehabilitation: The case of Sierra Leonean and Liberian 'child soldiers'. Journal of Health Psychology. 2007;12(3):498–504. . [DOI] [PubMed] [Google Scholar]
- 374.Mirzoev TN, Green AT, Newell JN. Progress towards health reform in Tajikistan. Journal of Health, Organisation and Management. 2007;21(6):495–505. . [DOI] [PubMed] [Google Scholar]
- 375.Morikawa MJ. Primary care training in Kosovo. Family Medicine. 2003;35(6):440–4. . [PubMed] [Google Scholar]
- 376.Moyo NT. ICM assists at a 'rebirth': the Midwives Association of Sierra Leone. International Midwifery. 2008;21(1):10–1. . Language: English. Entry Date: 20080926. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 377.Najafizada SA, Labonte R, Bourgeault IL. Community health workers of Afghanistan: a qualitative study of a national program. Conflict & Health [Electronic Resource]. 2014;8:26 10.1186/1752-1505-8-26 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Pavignani E. Human resources for health through conflict and recovery: Lessons from African countries. Disasters. 2011;35(4):661–79. . [DOI] [PubMed] [Google Scholar]
- 379.Palmer JJ, Surur EI, Checchi F, Ahmad F, Ackom FK, Whitty CJ. A mixed methods study of a health worker training intervention to increase syndromic referral for gambiense human African trypanosomiasis in South Sudan. PLoS Neglected Tropical Diseases [electronic resource]. 2014;8(3):e2742 10.1371/journal.pntd.0002742 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Petit D, Sondorp E, Mayhew S, Roura M, Roberts B. Implementing a Basic Package of Health Services in post-conflict Liberia: Perceptions of key stakeholders. Social Science and Medicine. 2013;78(1):42–9. . [DOI] [PubMed] [Google Scholar]
- 381.Prodan-Bhalla N. My journey to Sri Lanka. The Canadian nurse. 2003;99(9):8–10. . [PubMed] [Google Scholar]
- 382.Reamy J, Gedik G. Health human resource reform in Tajikistan: part of a masterplan for change. Cahiers de sociologie et de demographie medicales. 2001;41(3–4):327–45. . [PubMed] [Google Scholar]
- 383.Yagos WO, Olok GT, Ovuga E, Tabo Olok G. Use of information and communication technology and retention of health workers in rural post-war conflict Northern Uganda: findings from a qualitative study. BMC Medical Informatics & Decision Making. 2017;17:1–8. 10.1186/s12911-016-0403-3 . Language: English. Entry Date: In Process. Revision Date: 20170122. Publication Type: journal article. Journal Subset: Biomedical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Roome E, Raven J, Martineau T. Human resource management in post-conflict health systems: review of research and knowledge gaps. Conflict & Health [Electronic Resource]. 2014;8:18 10.1186/1752-1505-8-18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Tawfik-Shukor A, Khoshnaw H. The impact of health system governance and policy processes on health services in Iraqi Kurdistan. BMC International Health and Human Rights. 2010;10 (1) (no pagination)(14). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Tribe R, Weerasinghe D, Parameswaran S. Increasing mental health capacity in a post-conflict country through effective professional volunteer partnerships: A series of case studies with government agencies, local NGOs and the diaspora community. International Review of Psychiatry. 2014;26(5):558–65. . [DOI] [PubMed] [Google Scholar]
- 387.Stevens JC, Reilley B, Hargreaves S, Sattar A. A year in Afghanistan—Herat hospital paediatric ward. British Journal of General Practice. 2004;54(507):794–5. . [PMC free article] [PubMed] [Google Scholar]
- 388.Thompson E, Harding AL, Pond F, Hammond C, Taylor M. A partnership to improve health care in Kosovo. American Journal of Nursing. 2006;106(11):72CC-HH . Language: English. Entry Date: 20070112. Revision Date: 20150819. Publication Type: Journal Article.16481861 [Google Scholar]
- 389.Turkmani S, Currie S, Mungia J, Assefi N, Javed Rahmanzai A, Azfar P, et al. 'Midwives are the backbone of our health system': lessons from Afghanistan to guide expansion of midwifery in challenging settings. Midwifery. 2013;29(10):1166–72. . [DOI] [PubMed] [Google Scholar]
- 390.van der Veen A, van Pietersom T, Lopes Cardozo B, Rushiti F, Ymerhalili G, Agani F. Integrating staff well-being into the Primary Health Care system: a case study in post-conflict Kosovo. Conflict & Health [Electronic Resource]. 2015;9:21 10.1186/s13031-015-0048-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.van der Veer G, Francis FT. Field based training for mental health workers, community workers, psychosocial workers and counsellors: a participant-oriented approach. Intervention (15718883). 2011;9(2):145–53. 10.1097/WTF.0b013e32834902f1 . Language: English. Entry Date: 20110819. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [Google Scholar]
- 392.Ventevogel P, Ndayisaba H, van de Put W. Psychosocial assistance and decentralised mental health care in post conflict Burundi 2000 S 2008. Intervention (15718883). 2011;9(3):315–31. 10.1097/WTF.0b013e32834dffea . Language: English. Entry Date: 20120217. Revision Date: 20150712. Publication Type: Journal Article. [DOI] [Google Scholar]
- 393.Wilson W. Foya Hospital, Liberia; Medicine in a Post Conflict Setting. Heart Lung and Circulation. 2008;17(SUPPL. 4):S32–S6. . [DOI] [PubMed] [Google Scholar]
- 394.Hodgetts G, Broers T, Godwin M, Bowering E, Hasanovic M. Post-traumatic stress disorder among family physicians in Bosnia and Herzegovina. Family Practice. 2003;20(4):489–91. . [DOI] [PubMed] [Google Scholar]
- 395.Homan FF, Hammond CS, Thompson EF, Kollisch DO, Strickler JC. Post-conflict transition and sustainability in Kosovo: establishing primary healthcare-based antenatal care. Prehospital & Disaster Medicine. 2010;25(1):28–33. . Language: English. Entry Date: 20100528. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 396.Howard N, Woodward A, Patel D, Shafi A, Oddy L, ter Veen A, et al. Perspectives on reproductive healthcare delivered through a basic package of health services in Afghanistan: a qualitative study. BMC health services research. 2014;14:359 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Jerliu N, Burazeri G, Ramadani N, Hyska J, Brand H. Knowledge and practices of physicians regarding health status and health care services for older people in transitional Kosovo. Medical archives (Sarajevo, Bosnia and Herzegovina). 2013;67(3):164–7. . [DOI] [PubMed] [Google Scholar]
- 398.Kabeza AB, George N, Nyundo M, Levine AC. Development of emergency medicine in Rwanda. African Journal of Emergency Medicine. 2013;3(3):103–9. . [Google Scholar]
- 399.Keough ME, Samuels MF. The Kosovo Family Support Project: offering psychosocial support for families with missing persons. Social Work. 2004;49(4):587–94. doi: sw/49.4.587 . Language: English. Entry Date: 20050107. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 400.Khodjamurodov G, Rechel B. Health systems in transition. Health systems in transition. 2010;12(2):v-xix, 1–154. . [PubMed] [Google Scholar]
- 401.Kronfol NM. Rebuilding of the Lebanese health care system: Health sector reforms. Eastern Mediterranean Health Journal. 2006;12(3–4):459–73. . [PubMed] [Google Scholar]
- 402.Kuypers B. Assessing maternity services: 'collateral damage' of the Iraq war. RCM Midwives. 2005;8(4):160–2. . Language: English. Entry Date: 20050701. Revision Date: 20150818. Publication Type: Journal Article. [PubMed] [Google Scholar]
- 403.Kuypers B. Healing the wounds of war. Practising Midwife. 2005;8(11):38–40. . Language: English. Entry Date: 20060526. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 404.Leather A, Ismail EA, Ali R, Abdi YA, Abby MH, Gulaid SA, et al. Working together to rebuild health care in post-conflict Somaliland. Lancet. 2006;368 North American Edition(9541):1119–25. . Language: English. Entry Date: 20070518. Revision Date: 20170412. Publication Type: journal article. [DOI] [PubMed] [Google Scholar]
- 405.Lee PT, Kruse GR, Chan BT, Massaquoi MBF, Panjabi RR, Dahn BT, et al. An analysis of Liberia's 2007 national health policy: lessons for health systems strengthening and chronic disease care in poor, post-conflict countries. Globalization and Health. 2011;7 (no pagination)(37). . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Lori JR, Majszak CM, Martyn KK. Home-based life-saving skills in Liberia: acquisition and retention of skills and knowledge. Journal of Midwifery & Women's Health. 2010;55(4):370–7. 10.1016/j.jmwh.2009.09.016 . [DOI] [PubMed] [Google Scholar]
- 407.Lori JR, Munro ML, Moore JE, Fladger J. Lessons learned in Liberia: preliminary examination of the psychometric properties of trust and teamwork among maternal healthcare workers. BMC Health Services Research. 2013;13(1):134–. 10.1186/1472-6963-13-134 . Language: English. Entry Date: 20150508. Revision Date: 20161123. Publication Type: journal article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Low S, Tun KT, Mhote NP, Htoo SN, Maung C, Kyaw SW, et al. Human resources for health: task shifting to promote basic health service delivery among internally displaced people in ethnic health program service areas in eastern Burma/Myanmar. Global health action. 2014;7:24937 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Magnusson L, Ahlstrom G. Experiences of providing prosthetic and orthotic services in Sierra Leone—the local staff's perspective. Disability and rehabilitation. 2012;34(24):2111–8. . [DOI] [PubMed] [Google Scholar]
- 410.Mansoor GF, Hill PS, Barss P. Midwifery training in post-conflict Afghanistan: tensions between educational standards and rural community needs. Health Policy & Planning. 2012;27(1):60–8. . Language: English. Entry Date: 20120511. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 411.Marlowe P, Mahmood MA. Public health and health services development in postconflict communities: a case study of a Safe Motherhood project in East Timor. Asia-Pacific Journal of Public Health. 2009;21(4):469–76. 10.1177/1010539509345520 . Language: English. Entry Date: 20091204. Revision Date: 20150819. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 412.Smith JM, Currie S, Azfar P, Rahmanzai AJ. Establishment of an accreditation system for midwifery education in Afghanistan: maintaining quality during national expansion. Public Health. 2008;122(6):558–67. 10.1016/j.puhe.2008.03.009 . [DOI] [PubMed] [Google Scholar]
- 413.Smitz MF, Witter S, Lemiere C, Eozenou PH, Lievens T, Zaman RU, et al. Understanding Health Workers' Job Preferences to Improve Rural Retention in Timor-Leste: Findings from a Discrete Choice Experiment. PLoS ONE [Electronic Resource]. 2016;11(11):e0165940 10.1371/journal.pone.0165940 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Stambolovic V, Duric M, Donic D, Kelecevic J, Rakocevic Z. Patient-physician relationship in the aftermath of war. Journal of Medical Ethics. 2006;32(12):739–42. . Language: English. Entry Date: 20080208. Revision Date: 20150711. Publication Type: Journal Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Swan BA. Nursing infrastructure in Iraq: rebuilding a war-torn country. AAACN Viewpoint. 2004;26(6):6–7. . Language: English. Entry Date: 20050722. Revision Date: 20150711. Publication Type: Journal Article. [Google Scholar]
- 416.Eliades MJ, Lis J, Barbosa J, VanRooyen MJ. Post-war Kosovo: part 2. Assessment of emergency medicine leadership development strategy. Prehospital & Disaster Medicine. 2001;16(4):268–74. . Language: English. Entry Date: 20030627. Revision Date: 20150820. Publication Type: Journal Article. [DOI] [PubMed] [Google Scholar]
- 417.Ayiasi RM, Rutebemberwa, E., Martineau, T. (2016). Understanding deployment policies and systems for staffing rural areas in Northern Uganda during and after the conflict: synthesis report: ReBUILD consortium. https://rebuildconsortium.com/media/1509/deploymentugandaworkingdraft16dec16b.pdf.
- 418.Center for Public Health and Human Rights at Johns Hopkins Bloomberg School of Public Health. (2013). Protection of health workers pafitovRf.
- 419.Namakula J, Witter S., Ssengooba R. (2014). Health worker incentives during and after the conflict in Northern Uganda. ReBuild Consortium; (August 2014). [Google Scholar]
- 420.Zachariah R, Bienvenue B, Ayada L, Manzi M., Maalim A., Engy E.,… Harries A. D. (2012).Zachariah,: tele-consultations and tele-mentoring for improving paediatric care in a conflict setting in Somalia? Trop Med Int Health, 17(9), 1156–1162. 10.1111/j.1365-3156.2012.03047.x [DOI] [PubMed] [Google Scholar]
- 421.Martineau T. RE, Mangwi R., Chirwe Y., & Raven J. (2012). Understanding deployment policies and systems for staffing rural areas. ReBuold Consortium; 2012. [Google Scholar]
- 422.Oyerinde K, Harding Y., Amara P., Kanu R., Shoo R., & Daoh K. (2011). The status of maternal and newborn care services in Sierra Leone 8 years after ceasefire. International Journal of Gynecology and Obstetrics, 114(2), 168–173. [DOI] [PubMed] [Google Scholar]
- 423.Percival V, Richards E., MacLean T., & Theobald S. (2014). Health systems and gender in post-conflict contexts: building back better? Conflict and Health, 8(1), 19 10.1186/1752-1505-8-19 [DOI] [Google Scholar]
- 424.Murray SHhfhwifsFRfhfch-h-f-h-w-i-f-s.
- 425.Ssengooba F, Kawooya V., Namakula J., & Fustukian S. (2017). Application of social network analysis in the assessment of organization infrastructure for service delivery: a three district case study from post-conflict northern Uganda. Health Policy Plan, 32(8), 1193–1202. 10.1093/heapol/czx071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Youngs (2006). Human Resources for Health Programs for Countries in Conflict and Post-Conflict Situations. IntraHealth International (December 2006).
- 427.ReBUILD Consortium (2013). The Health Worker Incentives Uganda Briefing. October 2013. https://rebuildconsortium.com/media/1104/ugandaproject2briefingnote_22-10-2013.pdf
- 428.Clark P. A. (2006). Reinvigorated activity among midwives in Liberia after 14 years of civil war. International Midwifery, 19(4), 58–59. [Google Scholar]
- 429.Clarke S. (2010). A grave new world. Hands Up For Health Workers. Merlin. [Google Scholar]
- 430.Integrated Regional Information Networks (IRIN). (2006). Iraq: Neglected nurses fight their own war [Report]. Retrieved from http://www.irinnews.org/report/61948/iraq-neglected-nurses-fight-their-own-war
- 431.Sollom R. & Atkinson H. (2012). Under the Gun Ongoing Assaults on Bahrain's Health System. Physicians for Human Rights; (May 2012) [Google Scholar]
- 432.Amnesty International. (2011). Health crisis: Syrian government targets the wounded and health workers. Retrieved from: https://www.amnesty.org/en/documents/mde24/059/2011/en/
- 433.International Council of Nurses (ICN). (2012). Armed conflict nursing's perspective [Position Statement]. Retrieved from: https://www.icn.ch/sites/default/files/inline-files/E01_Armed_Conflict.pdf
- 434.International Committee of the Red Cross (ICRC). (2012). Health care in danger violent incidents affecting health care [Interim report]. Retrieved from https://www.icrc.org/en/doc/assets/files/reports/4050-002_violent-incidents-report_en_final.pdf https://www.icrc.org/en/doc/assets/files/reports/4050-002_violent-incidents-report_en_final.pdf
- 435.International Committee of the Red Cross (ICRC). (2011). Health care in danger a sixteen country study [Report]. Retrieved from: https://www.icrc.org/en/doc/resources/documents/report/hcid-report-2011-08-10.htm
- 436.International Committee of the Red Cross (ICRC). (2011). Health care in danger making the case. Retrieved from: https://www.icrc.org/en/publication/4072-health-care-danger-making-case
- 437.International Committee of the Red Cross (ICRC). (2011). Healthcare in danger a harsh reality [Brochure]. Retrieved from: https://www.icrc.org/en/publication/4074-health-care-danger-harsh-reality-brief-brochure
- 438.International Committee of the Red Cross (ICRC). (2012). Health care in danger violent incidents affecting health care [Interim report]. Retrieved from: https://www.icrc.org/en/publication/4237-health-care-danger-violent-incidents-affecting-delivery-health-care-january-2012
- 439.ReBUILD Consortium-Maintaining an effective health workforce during and after conflict Evidence from ReBUILD’s research in northern Uganda.
- 440.Medact (2008). Rehabilitation Under Fire- Health Care in Iraq 2003–2007.
- 441.Chirwa Y, Mashange, W., Chandiwana, P., Buzuzi, S., Munyati, S., Witter, S., et al. (2014). Understanding health worker incentives in three districts of Zimbabwe survey report.
- 442.Elyan DS, Monestersky J. H., Wasfy M. O, Noormal B., & Oyofo B. A. (2014). Capacity building of public health laboratories in Afghanistan: challenges and successes (2007–2011). Eastern Mediterranean Health Journal, 20(2), 112–119. [PubMed] [Google Scholar]
- 443.So S. & Witter S. (2016). The evolution of human resources for health policies in post-conflict Cambodia. ReBUILD Consortium. Working paper no. 19 (February 2016.)
- 444.Silove D, Rees S., Tam N., Liddell B., & Zwi A. (2011). Staff management and capacity building under conditions of insecurity: Lessons from developing mental health service and research programs in post-conflict Timor-Leste. Australasian Psychiatry, 19(SUPPL. 1), S90–S94. [DOI] [PubMed] [Google Scholar]
- 445.So S. A-GA, Witter S. (2016). Learning from the experiences of health workers in conflict-affected Cambodia to improve motivation and retention: analysis of life histories. ReBuild Consortium. Working paper no. 23. November 2016.
- 446.Wurie H. & Witter S. (2014).Serving through and after conflict life histories of health workers in Sierra Leone. ReBuild Consortium; (June 2014). [Google Scholar]
- 447.Wurie H.n Samai M. H., Witter S. (2014).Staffing the public health sector in Sierra Leone, 2005‐11: findings from routine data analysis. ReBuild Consortium. September 2014. [Google Scholar]
- 448.Witter S. CY, Namakula J., Samai M., So S. (2012). Understanding health worker incentives in post conflict settings. ReBuild Consortium, Project protocol summary 2012. [Google Scholar]
- 449.Witter S, Bertone M. P., Chirwa Y., Namakula J., So S., & Wurie H. R. (2016). Evolution of policies on human resources for health: opportunities and constraints in four post-crisis settings. Conflict & Health, 10:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Witter S. TO, Martineau T. (Witter, S., Tulloch, O. and Martineau, T. 2012. Health workers’ incentives in post-conflict settings–a review of the literature and framework for research. ReBUILD RPC research report.). Health workers’ incentives in post-conflict settings–a review of the literature and framework for research
- 451.Witter S. WH, Bertone M. P. (2014). Witter, S., Wurie, H. and Bertone, M. 2014. The Free Health Care Initiative: how has it affected health workers in Sierra Leone? ReBUILD RPC Research Report The Free Health Care Initiative- How Has it Affected Health Workers in Sierra Leone. [DOI] [PMC free article] [PubMed]
- 452.ReBUILD Consortium (2014). Managing human resources in post-conflict health systems: a review of research and knowledge gaps. (October 2014). [DOI] [PMC free article] [PubMed]
- 453.ReBUILD Consortium (2015). Evidence for supporting a skilled health workforce for all in Sierra Leone. October 2015
- 454.ReBUILD Consortium (2015). Research to inform health systems development: An overview of the ReBUILD RPC in Cambodia. November 2015.
- 455.ReBUILD Consortium (2016). Evidence submitted by the ReBUILD Research Programme Consortium to the High-Level Commission on Health Employment and Economic Growth. (16 June 2016).
- 456.ReBUILD Consortium (2016). Maintaining an effective health workforce during and after conflict Evidence from ReBUILD’s research in northern Uganda. April 2016.
- 457.ReBUILD Consortium (2015). The challenge of retaining health workers in Zimbabwe Implications for Universal Health Coverage. August 2015.
- 458.Boulton J. (2016). ‘Ebola don go’: nursing in Sierra Leone. British Journal of Nursing, 25(9), 505–507. [Google Scholar]
- 459.ReBUILD Consortium (2015). Incentives to improve health workers’ retention and motivation: implementation challenges and informal practices at district level. The role of DHMTs and NGOs. Policy Brief. Reterived from: https://rebuildconsortium.com/media/1268/rebuild-sl-policy-brief-3-hrh-practices-at-district-level.pdf
- 460.ReBUILD Consortium. Exploring the remuneration of primary healthcare workers: findings on incomes and income use strategies. What lessons can be learnt to design effective financial incentives?
- 461.Schmidt-Ehry G. (2000). Training and research for implementation of health care system reform in Cambodia. Asia-Pacific journal of public health / Asia-Pacific Academic Consortium for Public Health, 12 Suppl, S21–27. [PubMed] [Google Scholar]
- 462.ReBUILD Consortium. Key messages from ReBUILD Research in Uganda. Reterived from: https://rebuildconsortium.com/media/1471/rebuild-uganda-key-messages_final.pdf
- 463.ReBUILD Consortium (2015). The challenge of retaining health workers in Zimbabwe findings from ReBUILD research. August 2015
- 464.The Capacity Project. (2007). Ready to Rebuild: Sudanese Doctors Return Home. IntraHealth International. Retrieved from: https://www.capacityproject.org/index.php%3Foption=com_content&task=view&id=139&Itemid=108.html The
- 465.Smith JR, Ho LS, Langston A, Mankani N, Shivshanker A, Perera D. Clinical care for sexual assault survivors multimedia training: a mixed-methods study of effect on healthcare providers' attitudes, knowledge, confidence, and practice in humanitarian settings. Confl Health. 2013;7:14 Epub 2013/07/04. 10.1186/1752-1505-7-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.So S, Alonso-Garbayo, A. and Witter, S. 2016. Learning from the experiences of health workers in conflict-affected Cambodia to improve motivation and retention: analysis of life histories. ReBUILD RPC Working Paper.
- 467.Tosevski DL, Milovancevic M. P., Pejuskovic B., Deusic S. P., Mikulec E. T., & Hofvedt B. O. (2006). Burnout syndrome of general practitioners in post-war period [1]. Epidemiologia e Psichiatria Sociale, 15(4), 307–310. [PubMed] [Google Scholar]
- 468.Tulloch O, Raven J., & Martineau T. (2011). Human Resources for Health in post-conflict settings. Liverpool: ReBUILD Consortium. [Google Scholar]
- 469.Witter S. BMP, Wurie H., Samai M., Edem-Hotah J., Amara R. (2015). Health worker incentives- survey report, Sierra Leone. ReBuild Consortium (January 2015).
- 470.World Health Organization (2005). Guide to Health Workforce Development in Post-Conflict Environments. World Health Organization G, Switzerland. [Google Scholar]
- 471.Sen K, Hussain H, Al-Faisal W. Ethics in times of conflict: some reflections on Syria, in the backdrop of Iraq. BMJ Global Health. 2016;1(3):e000149 10.1136/bmjgh-2016-000149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Iyer AR. Authorship trends in The Lancet Global Health. The Lancet Global health. 2018;6(2):e142 Epub 2018/02/02. 10.1016/s2214-109x(17)30497-7 . [DOI] [PubMed] [Google Scholar]
- 473.Bowsher G, Papamichail A, El Achi N, Ekzayez A, Roberts B, Sullivan R, et al. A narrative review of health research capacity strengthening in low and middle-income countries: lessons for conflict-affected areas. Globalization and health. 2019;15(1):23 Epub 2019/03/28. 10.1186/s12992-019-0465-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Ismail SA, McDonald A, Dubois E, Aljohani FG, Coutts AP, Majeed A, et al. Assessing the state of health research in the Eastern Mediterranean Region. Journal of the Royal Society of Medicine. 2013;106(6):224–33. Epub 2013/06/14. 10.1258/jrsm.2012.120240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Mandil A, El-Jardali F, El-Feky S, Nour M, Al-Abbar M, Bou-Karroum L. Health research institutional mapping: an Eastern Mediterranean Regional perspective. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2018;24(2):189–97. Epub 2018/05/12. . [PubMed] [Google Scholar]
- 476.Tugwell P, Sitthi-Amorn C, Hatcher-Roberts J, Neufeld V, Makara P, Munoz F, et al. Health Research Profile to assess the capacity of low and middle income countries for equity-oriented research. BMC public health. 2006;6:151 Epub 2006/06/14. 10.1186/1471-2458-6-151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Gonzalez Block MA, Mills A. Assessing capacity for health policy and systems research in low and middle income countries*. Health Res Policy Syst. 2003;1(1):1 Epub 2003/03/21. 10.1186/1478-4505-1-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Mills A. Health care systems in low-and middle-income countries. New England Journal of Medicine. 2014;370(6):552–7. [DOI] [PubMed] [Google Scholar]
- 479.Ford N, Mills EJ, Zachariah R, Upshur R. Ethics of conducting research in conflict settings. Conflict and health. 2009;3(1):7 10.1186/1752-1505-3-7 [DOI] [PMC free article] [PubMed] [Google Scholar]