Abstract
Background
Carotid artery plaque is an established marker of subclinical atherosclerosis with pronounced sex-dimorphism. Here, we aimed to identify genetic variants associated with carotid plaque burden (CPB) and to examine potential sex-specific genetic effects on plaque sizes.
Methods and results
We defined six operationalizations of CPB considering plaques in common carotid arteries, carotid bulb, and internal carotid arteries. We performed sex-specific genome-wide association analyses for all traits in the LIFE-Adult cohort (n = 727 men and n = 550 women) and tested significantly associated loci for sex-specific effects. In order to identify causal genes, we analyzed candidate gene expression data for correlation with CPB traits and corresponding sex-specific effects. Further, we tested if previously reported SNP associations with CAD and plaque prevalence are also associated with CBP. We found seven loci with suggestive significance for CPB (p<3.33x10-7), explaining together between 6 and 13% of the CPB variance. Sex-specific analysis showed a genome-wide significant hit for men at 5q31.1 (rs201629990, β = -0.401, p = 5.22x10-9), which was not associated in women (β = -0.127, p = 0.093) with a significant difference in effect size (p = 0.008). Analyses of gene expression data suggested IL5 as the most plausible candidate, as it reflected the same sex-specific association with CPBs (p = 0.037). Known plaque prevalence or CAD loci showed no enrichment in the association with CPB.
Conclusions
We showed that CPB is a complementary trait in analyzing genetics of subclinical atherosclerosis. We detected a novel locus for plaque size in men only suggesting a role of IL5. Several estrogen response elements in this locus point towards a functional explanation of the observed sex-specific effect.
Introduction
Atherosclerosis is a chronic disease characterized by arterial lumen reduction due to arterial wall thickening and development of plaques. Major risk factors are high cholesterol, age, sex, smoking and obesity [1]. As atherosclerosis has a long pre-clinical phase, non-invasive methods can be used for early detection. Those methods can be used to identify people who are at high risk of a cardiovascular event [2], and thus offers a means of prevention [3]. B-mode ultrasound measurement of the carotid arteries is one of these non-invasive methods with which the carotid intima media thickness (cIMT) and carotid plaques sizes can be measured [4].
Genetic predisposition also contributes to atherosclerosis risk: The latest meta-analyses with 34,541 cases of coronary artery disease (CAD) and 261,984 controls reported 169 genetic risk loci with genome-wide significance (p<5x10-8) [5]. For carotid plaques, 14 loci were described with at least suggestive significance (p<1x10-6) [6]. Both CAD and carotid plaques share genetic risk loci, such as the 9p21 locus [5–7], and are genetically correlated [6].
Male sex is an independent risk factor of several traits and diseases including atherosclerosis, although the underlying mechanisms are only partly understood [8,9]. Recent genome-wide analyses detected sex-specific effects across biomarkers [10,11], especially for steroid hormones [11]. It is yet unclear what causes the difference of effects, e.g. whether it is related to the role of the underlying enzyme in steroid metabolism, or due to hormone response elements within the genome controlling gene expression. Mendelian Randomization has shown male-specific causal effects of cortisol and androstenedione, and female-specific causal effects of dehydroepiandrosterone sulfate (DHEA-S) on CAD [11]. For cIMT, Dong et al. [12] reported SNP-sex interaction for two genetic loci.
Genetics of atherosclerosis onset and progression / severity could be different. Zeller et al. [13] only detected one hit for Gensini score [14] as a marker of cardiovascular disease severity. A recent GWAS on myocardial infarction risk among patients with stable CAD revealed a limited number of loci and detected pronounced differences of effects on CAD onset and MI (personal communication).
To the best of our knowledge there is only one published study on genetics of carotid plaque sizes. Della-Morte et al. [15] analyzed the interaction of SNPs and smoking on carotid plaque burden (CPB) in 665 people of Caribbean Hispanic ancestry, followed by replication analyses in 264 people of the same ancestry. While they detected two significant SNP-smoking interactions, they did not describe any genome-wide significant loci. However, this study was far less powered than studies of CAD or plaque prevalence making further efforts to understand genetics of atherosclerosis progression a worthwhile endeavor.
Here, we conducted a genome-wide association study (GWAS) of six CPB traits in 1277 Europeans, considering both the absolute sizes of and the relative lumen reductions by the plaques. We aimed to discover genetic markers for CPB and estimate the heritability of carotid plaque sizes. Since sex is one of the strongest risk factors, we attempted to find SNP-sex interactions at candidate loci both on genome and transcriptome level. We also analyzed known genetic CAD and carotid plaque loci for association with our CPB traits to check for a genetic overlap with these traits.
Material and methods
Cohort description
The LIFE-Adult cohort is a population-based study with a focus on civilization diseases such as type 2 diabetes and subclinical forms of cardiovascular diseases. 10,000 individuals were recruited in the city of Leipzig in an age- and sex-stratified manner. The baseline examination was conducted from August 2011 to November 2014. Details can be found elsewhere [16]. LIFE-Adult meets the ethical standards of the Declaration of Helsinki and has been approved by the Ethics Committee of the Medical Faculty of the University of Leipzig (Registration Number 263-2009-14122009). Written informed consent including agreement with genetic analyses was obtained from all participants.
Carotid ultrasound and plaque assessment
A standardized carotid ultrasound was applied to all participants of LIFE-Adult, except those with cervical spine disorder or wounds at the scanning area. High-resolution B-mode ultrasound images of carotid vessels were acquired using the GE Vivid ultrasound platform with a 12.0-MHz linear-array transducer (GE-Healthcare). During the assessments, subjects were in the supine position while trained study nurses scanned four anatomical regions for carotid plaques: common carotid artery (CCA), carotid bulb (Bulb) and proximal parts of the internal carotid artery (ICA) and the external carotid artery (ECA) on both sides of the neck. Details can be found elsewhere [7].
Carotid artery plaque was defined according to the American Society of Echocardiography Intima-Media Thickness Task Force [4]. In detail, a lesion was counted as plaque if one of the following three criteria was met:
echogenic thickening of intimal reflection that extends into the arterial lumen at least 0.5 mm;
swell of more than 50% of the surrounding intima-media thickness;
thickness of intima and media >1.5 mm.
Plaque presence was documented as ‘present’ or ‘absent’ or ‘missing’ if the quality of the image was insufficient.
While recruitment was still in process, 1300 samples were selected for a detailed assessment of the sizes of plaques in CCA, Bulb and ICA (ECA was neglected due to lower image qualities). The selection criterion was at least one plaque present in any region and genetic data available (first round of genotyping), with preference for samples with two or more plaques (n = 1804 with plaque present and genetic data available). Using cross-sectional images, total plaque area and total lumen area were determined. We defined and analyzed six traits of carotid plaque burden (CPB):
CPA_max: area of the largest plaque detected at any of the six regions
CPA_sum: sum of plaque areas at all six regions
CPA_mean: mean area of detected plaques
CPS_max: maximal degree of stenosis (plaque area / lumen area) at any of the six regions
CPS_sum: sum of stenosis at all six regions
CPS_mean: mean degree of stenosis
Due to the complex and time-consuming measuring in six regions, the sample selection for the subsequent rounds of genotyping was not updated.
Genotyping
We genotyped 7,838 participants of LIFE-Adult using the genome-wide SNP array Affymetrix Axiom CEU1 and the software Affymetrix Power Tools (version 1.20.6). Quality control (QC) of the genotype calling was performed following Affymetrix’s best practice steps [17].
Sample QC included dish-QC (<0.82), sample call rate (<97%), sex-mismatch, problematic relatedness (e.g. sample mix-up) and irregularities of XY intensity plots (e.g. XXY samples filtered for gonosomal analyses). We assessed genetic heterogeneity with principal component analyses and filtered outliers (>6 SD in any of the first 10 principal components) for further analysis.
SNP QC comprised SNP call rate, parameters of cluster plot irregularities according to Affymetrix’s recommendations, violation of Hardy-Weinberg equilibrium (p<10−6 in an exact test for autosomes, p<10−4 for chromosome X with women only [18]) and plate association (p<10−7).
After sample and SNP QC, 7669 samples and 532,676 SNPs were imputed on the reference 1000 Genomes Phase 3 [19], software SHAPEIT [20] v2r900 for prephasing and IMPUTE2 [21] v2.3.2 for genotype estimation. For chromosome X, the same settings were used.
Statistical analysis
All six CPB traits were log transformed to approximate normal distributions (see S1 Fig). If not stated otherwise, statistical analyses were performed with the software R [22]. We tested the correlation between CBPs and cIMT using spearman’s rank correlation. Univariate and multivariate associations of known risk factors of atherosclerosis (sex, age, BMI, hypertension (defined by positive anamnestic information, specific treatment or systolic blood pressure>140mmHg), diabetes type 2 (defined by positive anamnestic information, specific medication or HbA1c≥6.5%), smoking status (never vs. former vs. active smokers), and statin treatment) on CPBs were calculated using linear regression. We also analyzed the correlation of CPBs with total cholesterol, high and low density cholesterol (HDLC and LDLC, respectively), adjusting for sex and statin treatment.
Heritability
To estimate the heritability of carotid plaque burden we used the tool GCTA (version 1.92.0beta3) [23]. We calculated a genetic relationship matrix for each autosomal chromosome and estimated the variance explained by the SNPs of each chromosome by separate mixed model analyses. Finally, we combined the results assuming the autosomal chromosomes as statistically independent:
For each phenotype, we estimated the heritability in three models: unadjusted; adjusted for sex and age only; and adjusted for cardiovascular risk factors (sex, age, BMI, smoking status, statin treatment, type 2 diabetes, and hypertension).
Genome-wide association analyses
For each CPB trait, separate genome-wide analyses were performed for all samples (adjustment for sex and age) and for the subgroups of sexes (adjustment for age). All analyses were executed with PLINK 2.0 [24,25] using the additive frequentist model and expected genotype counts. X-chromosomal SNPs were analyzed assuming total X inactivation. We checked for associations with the genetic principal components, but detected none (see S1 Table), therefore, we refrained from adjusting for PCs in our GWAS analyses. We filtered SNPs with MAF<1% or imputation info-score<0.8. Adjusting for the three GWAS, we set the genome-wide and suggestive significance level to αgw = 1.67×10−8 and αsug = 3.33×10−7, respectively. Associations reaching at least suggestive significance in one of the GWAS were considered as “associated” in the following. Associated SNPs were ordered by significance and summarized to loci by building the set of associated SNPs in linkage disequilibrium (LD; r2>0.1) or in physical proximity (+/- 500 kb) to the respective lead SNP until all SNPs are assigned. For each locus, a regional association plot was generated. After manual inspection of these plots, we removed one locus showing no support of the lead SNP, as no other variant but the lead SNP was associated at this locus. LD was calculated using LIFE-Adult data for all samples with CPB traits, providing matching LD parameter for association statistics.
We merged all GWAS results and annotated them with the following bioinformatics resources: nearby Ensembl genes (+/-250 kb) [26], comparison with variants reported in the GWAS Catalog (LD r2>0.3) [27], expression quantitative trait loci data (LD r2>0.3; filtering for eQTLs with αcis = 0.05 and αtrans = 1×10−7 for cis- and trans-eQTLs, respectively) [28–32], and pathways from KEGG, GO, DOSE and Reactome [33,34]. LD to SNPs from GWAS Catalog or eQTL variants were calculated using data from 1000 Genomes Phase 3, Version 5 (2015) for European samples [19].
Subsequent analyzes of lead SNPs
We performed difference test [35] for all lead SNPs:
using a Bonferroni-corrected significance level αDiff = 0.0071, adjusting for 7 lead SNPs.
Furthermore, we analyzed robustness and sex-specificity of our detected loci by comparing the following models: 1) we additionally adjusted for the first ten genetic principal components to test for robustness. 2) We adjusted for cardiovascular risk factors (BMI, smoking status, statin treatment, type 2 diabetes, and hypertension) to analyze possible confounding effects. 3) We used all 16 SNPs in a multivariate model to detect combined effects. Models were analyzed for all individuals and for men and women separately.
For the top locus 5q31.1 and top phenotype CPA_mean, we performed credible set analyses, using 2,245 SNPs within +/-500 kb of the lead SNP rs201629990 [36,37], for all samples and the subset with men and women only, respectively. We used the R-package “gtx” to derive Approximate Bayes Factors (ABF) from the effect estimates and standard errors. Standard deviation priors were chosen depending on effect size ranges (95% range of SNP effects by (2*1.96)): 0.058 for all samples, 0.085 in men, and 0.055 in women. The ABFs were then used to calculate the posterior probability for the variant driving the association signal (e.g. causal variant). We ordered variants by their posterior probability and the calculated for each SNP the cumulative posterior, that is the sum of posterior probabilities of SNP with less than or equal order. The 99% credible sets contain with a 99% cumulative posterior probability the causal variant. To validate our results, we considered the association of SNPs at 5q31.1 with the carotid plaque score (PS), which we analyzed in a previous work [7]. In short, PS is the sum of carotid plaques at CCA and Bulb on both sides of the neck, taking values from 0 to 4. For PS we used a prior of 0.052.
Gene expression look-up
To functionally classify the observed SNP-sex interaction at 5q31.1, we analyzed blood gene expression profiles of candidate genes for association with CPBs. For 3,527 LIFE-Adult participants, whole blood was collected in Tempus Blood RNA Tubes (Life Technologies) and relocated to -80°C before further processing. Isolated RNA was processed and hybridized to Illumina HT-12 v4 Expression BeadChips (Illumina, San Diego, CA, USA) and measured on the Illumina HiScan. Raw data of 48,107 gene-expression probes were extracted by Illumina GenomeStudio without additional background correction. Data were further processed within R/Bioconductor. Expression values were log2-transformed and quantile-normalized. Batch effects of expression BeadChips were corrected using an empirical Bayes method [38]. Restricting on subjects with CPBs, a sample size of 935 (537 men, 398 women) was available. Of the 40 candidate genes obtained from eQTL data and nearby gene annotation of the lead SNP, 32 were available with high quality probes in our data. All gene-expressions were adjusted for age, lymphocytes and monocytes.
Analysis of known atherosclerosis SNPs
We analyzed SNPs known to be associated with CAD (n = 169 SNPs in van der Harst et al. [5]), carotid plaques or carotid intima media thickness (GWAS catalog search; n = 133 SNPs) [6,7,12,15,39–44]) in more detail to verify possible associations with plaque burden. For CAD, 159 SNPs were available in our data and for one we used a proxy in high LD (r2 = 0.993). For the carotid SNPs, 105 were available in our data, and for one we used a proxy (LD r2 = 0.732). SNPs were defined as verified for association with plaque burden if they reached at least p<0.05/6 (Bonferroni correction for six phenotypes of plaque burden) and had concordant direction of the effect. To test for enrichment of associated SNPs, we performed a binomial test.
In addition, we tested a polygenetic score (PGS) of CAD for association with CPB traits in men and women separately, and both. Effect weights were obtained from PGS Catalog [45] for 1,7 million variants using data from Inouye et al. [9] (PGS ID: PGS000018). We filtered variants with MAF<1%, imputation info score<0.8 and mismatching alleles in our data, and calculated the PGS as sum of effect weight times genedoses over 1,378,307 SNPs.
Results
Impact of non-genetic parameters on plaque burden
Basic characteristics of study subjects are summarized in Table 1. All participants had at least one carotid plaque, with 96% occurring in the carotid bulb. Irrespective of the considered CPB parameter, men had significantly higher plaque burden than women. On average, women had fewer plaques at ACC, bulb and ACI (2.2 plaques in women; 2.9 plaques in men). While the age distribution was the same for men and women (p = 0.127), all other known risk factors of atherosclerosis differed significantly. All CPB traits were highly correlated with each other (spearman ρ between 0.70 and 0.96, p<2x10-16, see S2 Fig).
Table 1. Characteristics of study subjects.
| Parameter | Men | Women | p | |
|---|---|---|---|---|
| Sex | 727 (57.0%) | 550 (43.0%) | --- | |
| Age (years) | 64.9 (9.7) | 64.2 (9.6) | 0.127 | |
| BMI (kg/m2) | 28.1 (4.0) | 27.9 (5.0) | 0.046 | |
| smoking status | former current | 294 (44.1%) 153 (22.9%) |
97 (20.2%) 102 (21.2%) |
< 0.001 |
| Hypertensiona | 533 (73.9%) | 356 (66.4%) | 0.005 | |
| type 2 diabetesa | 142 (19.5%) | 73 (13.3%) | 0.004 | |
| Statin therapyb | 216 (29.7%) | 91 (16.5%) | < 0.001 | |
| CHOL (mmol/l) | 5.48 (1.10) | 6.04 (1.04) | < 0.001 | |
| HDL-C (mmol/l) | 1.38 (0.37) | 1.74 (0.44) | < 0.001 | |
| LDL-C (mmol/l) | 3.46 (0.99) | 3.72 (0.94) | < 0.001 | |
| CPA_max (max. area, mm2) | 27.2 (17.6) | 19.6 (13.3) | < 0.001 | |
| CPA_sum (sum of plaque area, mm2) | 56.4 (46.2) | 34.8 (31.4) | < 0.001 | |
| CPA_mean (mean area of plaque, mm2) | 18.0 (9.1) | 14.5 (7.9) | < 0.001 | |
| CPS_max (max. stenosis, in %) | 32 (19) | 27 (17) | < 0.001 | |
| CPS_sum (sum of stenosis, in %) | 71 (60) | 50 (47) | < 0.001 | |
| CPS_mean (mean degree of stenosis, in %) | 22 (11) | 20 (11) | 0.006 | |
| number of Carotid Plaques | 2.9 (1.5) | 2.2 (1.3) | < 0.001 | |
| Plaques at ACC | unilateral bilateral | 160 (22.0%) 112 (15.4%) |
95 (17.3%) 42 (7.6%) |
< 0.001 |
| Plaques at Bulbus | unilateral bilateral | 232 (32.2%) 462 (64.1%) |
250 (45.9%) 271 (49.7%) |
< 0.001 |
| Plaques at ACI | unilateral bilateral | 225 (33.1%) 153 (22.5%) |
132 (25.7%) 58 (11.3%) |
< 0.001 |
| cIMT mean | 0.85 (0.16) | 0.81 (0.14) | < 0.001 | |
| cIMT max | 1.12 (0.27) | 1.09 (0.24) | 0.351 | |
Binary / categorical variables are given in absolute counts (% per sex). Continuous variables are reported by mean (SD). Differences between sexes were tested with the Chi-squared test (categorical traits) or the Mann-Whitney U test (continuous traits). CPB statistics are given before transformation.
a Known, in therapy or acute
b ATC-code beginning with C10
We analyzed the correlation of CBP traits, cIMT and lipid parameters total, HDL, and LDL cholesterol. Considering all subjects, we detected a weak inverse correlation between CBPs and HDL cholesterol (spearman ρ about -0.10, see S2 Fig, S1 Table). Analyzing women only, the positive correlation with total and LDL cholesterol reached significance for three and four CBP traits, respectively. This correlation increased further when restricting to women without statin treatment (spearman ρ of all CPBs ranging from 0.11 to 0.21). There was a moderate positive correlation between mean cIMT and CPBs (spearman ρ between 0.21 and 0.36), which was stronger in men than in women. The correlation with maximal cIMT was weak, and not significant in the sex-separated analyses.
We tested the cardiovascular risk factors sex, age, BMI, smoking status, hypertension, type 2 diabetes, and statin therapy for effects on carotid plaque burden in all participants and separately in men and women (see S2 Table). BMI was weakly associated with the CPB traits, and this association was mainly driven by men. Of note, BMI had a negative effect on CPBs, e.g. a higher BMI is associated with smaller plaque area. Batagini et al. [46] also described lower BMI in patients with carotid artery stenosis compared to controls, which is in line with our findings for BMI and CPB. Type 2 diabetes was only univariately associated with traits considering the sum of plaques (area as well as stenosis). Although associated, all risk factors explained only small percentages of trait variance (e.g. 6% explained variance of CPS_mean, 19% of CPA_sum).
Heritability of CPBs
Using a univariate model, we could not detect any significant heritability for the CPB traits (see S3 Table). After adjusting for all above mentioned cardiovascular risk factors, the heritability estimates increased and ranged between 68% (CPA_max, maximal area, p = 0.039) and 82% (CPS_max, maximal stenosis, p = 0.013). For our previously considered plaque score (PS) we detected significant estimates for both models (univariate model: h2 = 21%, p = 0.025; adjusted for risk factors: h2 = 33%, p = 0.002). Here, a larger sample size was available (N = 4,023).
GWAS results
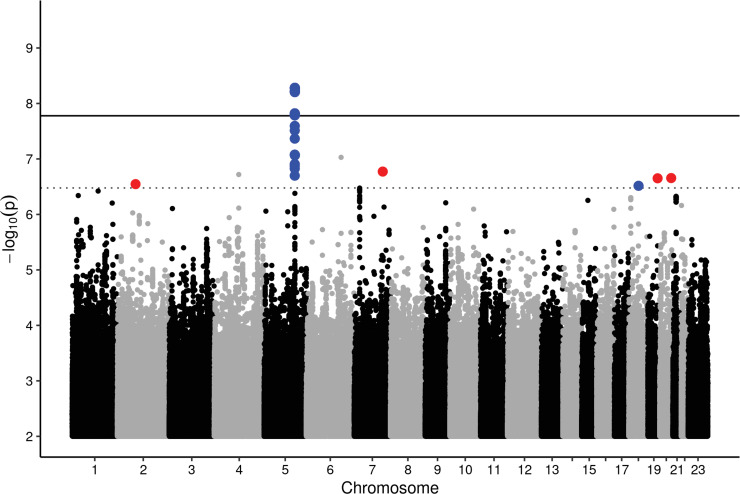
In our GWAS, we detected no signs for inflation of test statistics (λ ranged between 1.00 and 1.02). A Manhattan plot for all CPB traits is provided in Fig 1. After priority pruning with r2>0.1, we detected seven different loci reaching at least suggestive significance (αsug = 3.33×10−7) and one reaching genome-wide significance (αgw = 1.67×10−8). One of the suggestive loci was not supported in the regional association plot by any other variant and therefore excluded from further analysis. The remaining seven loci are presented in Table 2.
Fig 1. Manhattan-plot of all CPB traits.
Minimal p-values across the six traits and three setting were displayed. The line corresponds to a genome-wide significance threshold of 1.67x10-9. Blue points mark regions associated strongest in men, red associations in women.
Table 2. Lead-SNPs of associated loci.
| Cytoband | Lead SNP | Candidate | EA / OA | EAF | Info | associated CPBs | beta | SE | p-value | IA |
|---|---|---|---|---|---|---|---|---|---|---|
| Genes | ||||||||||
| 5q31.1 | rs201629990 | IL5 (78 kb) | GT / G | 0.038 | 0.982 | CPA_mean (A, M) CPA_max (A, M) | -0.401 | 0.068 | 5.22x10-9 | 6.85x10-3 |
| 6q21 | rs72942431 | SELL (trans-eQTL) | A / G | 0.300 | 0.940 | CPS_max (A) CPS_mean (A) | -0.151 | 0.029 | 5.36x10-8 | 0.466 |
| 4q22.3 | rs3821968 | BMPR1B (0 kb) | T / C | 0.118 | 0.961 | CPS_sum (A) | 0.299 | 0.057 | 1.91x10-7 | 0.840 |
| 20q13.31 | rs58056086 | TFAP2C (42 kb) | T / C | 0.088 | 0.887 | CPS_mean (W) CPS_max (W) | -0.319 | 0.061 | 2.21x10-7 | 2.60x10-4 |
| 19q13.33 | rs4539714 | FPR1 (989 kb) | C / T | 0.194 | 0.905 | CPA_sum (W) | 0.360 | 0.069 | 2.23x10-7 | 4.70x10-4 |
| 2p12 | rs6729048 | ABCC1 (trans eQTL) | A / T | 0.137 | 0.995 | CPA_sum (W) | -0.369 | 0.071 | 2.84x10-7 | 2.19x10-3 |
| 18q12.3 | rs7245281 | PSTPIP2 (160 kb) | A / G | 0.197 | 0.956 | CPS_sum (M) | -0.322 | 0.062 | 3.05x10-7 | 2.00x10-5 |
Per locus the most strongly associated variant is given. Beta estimate, standard error (SE) and p-value are reported for the best-associated phenotype and modus (marked bold). Biologically meaningful genes are listed as candidates (plausible in context with atherosclersosis and sex-specifity). For cis-eQTLs distance in kb is given. For statistics of the other CPBs and full annotation, see S4–S7 Tables. Abbreviations: EA/OA: effect/other allele; EAF: effect allele frequency; info: imputation info score; IA: p-value of difference test.
The strongest association was detected for CPA_mean with the SNP rs201629990 at cytoband 5q31.1 in men (β = -0.401, p = 5.22x10-9). In the combined analysis, the association reached only suggestive significance (p = 1.19x10-7), but the SNP was not associated in women (p = 0.093). The variant was also associated with CPA_max at suggestive significance in men and the combined setting. It is a non-coding exon modifier of a Y-RNA, which are known to induce inflammation and an atherogenic effect was described [47,48]. It is also an intron modifier of C5orf56, which codes for an Interferon regulatory factor 1 (IRF1) antisense RNA. The lead SNP is supported by 29 variants in LD (r2>0.1) and is an eQTN or in LD with an eQTLn for 23 genes including the aforementioned genes IRF1 [29] and C5orf56 [28] (LD r2>0.3). Other GWAS previously reported “Red cell distribution width” [49], fibrinogen levels [50–52], and chronic inflammatory diseases [53] for this region (LD r2>0.75). Summary statistics, nearby genes, eQTL and GWAS Catalog look-up are provided in S4–S7 Tables, respectively.
Comparison of models
Using different models (univariate association, adjusting for up to 10 genetic PCs, adjusting for cardiovascular risk factors) did not significantly change the effect sizes (S8 Table). In a multivariate model including all seven top-SNPs, the explained variance by genetics was about 6% in men and 12% in women. Adding cardiovascular risk factors, the explained variance increased to similar values in men and women (e.g. CPA_mean with 10.7% and 12.5% in men and women, respectively). In all combined models, almost all SNPs remained significant, although no longer on suggestive but nominal level (see S8 Table).
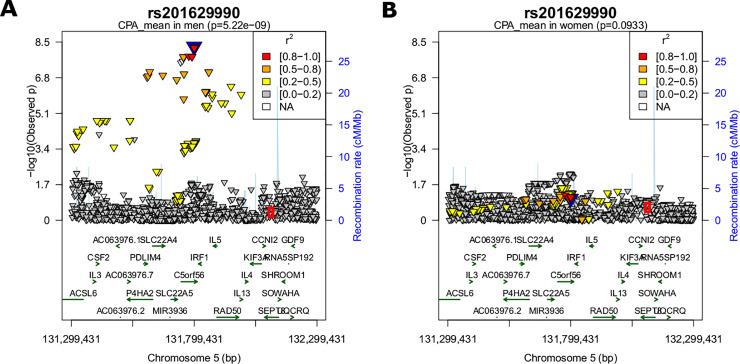
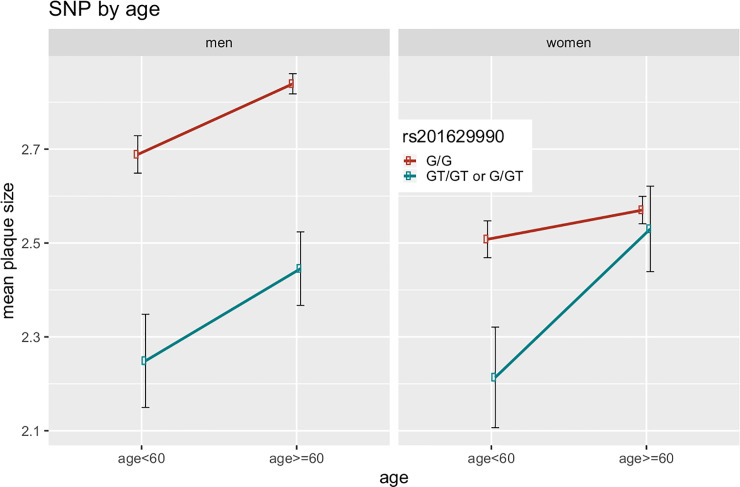
Testing for sex interaction, we compared the effect sizes calculated in the sex-stratified analyses. Here, we found significant difference in effect size for all sex-specific loci. We repeated this analysis for all associated SNPs at the top locus 5q31.1 and found SNPs in high LD with the lead SNP (r2>0.6) showing the same behavior. Less correlated variants showed no sex-specificity (see regional association plots for men and women in Fig 2 and S9 Table). Since estrogen-response elements were reported for this region, we tested whether this is an age-dependent phenomenon, e.g. menopausal status in women. For participants younger than 60 years, we detected no significant difference in effect sizes, but within the elderly, 29 SNPs showed significantly stronger effects in men than women (see Fig 3 for SNP-age interaction).
Fig 2. Regional association plots.
Regional association plot of locus 5q31.1 for (A) men and (B) women. P-value of SNPs were log10 transformed and colored by LD (r2 to lead SNP rs201629990). The red circle marks the position of the independent hit detected in the credible set analysis in women, rs33967116. This SNP is nominally associated with carotid plaque score (see S4 Fig).
Fig 3. SNP-by-sex interaction plots.
Interaction plot of Top-SNP rs201629990 by age (younger than 60 years, older than 60 years) for men and women. Since there were only two participants with genotype “GT/GT”, we pooled them with the genotype group “GT/G” (n = 108 for both “GT/GT” & “GT/G”, n = 1169 for”G/G”).
We performed joint analyses of 2,279 SNPs at this locus (+/- 500 kb of lead SNP rs201629990) for all samples, and separately for men and women. Each run produced one independent hit: rs114597978 for all (LD to rs201629990, r2 = 0.929), rs201629990 in men and rs33967116 in women (LD to lead SNP r2 = 0.003). All 24 associated SNPs generate an 82.7% credible set in the combined analysis, whereas in the subset of men, those SNPs produced a 91.9% credible set (S3 Fig). They had all shown a male-specific effect. In contrast, the 91.9% credible set for women contained 1903 SNPs due to lack of a strong signal. In men, the lead SNP was ranked third with a posterior probability of 0.063. In summary, the variant causing the association is most certainly one of the male-specific SNPs. However, we cannot use the credible set to reduce the SNP list of our GWAS, as all associated SNP are within the 95% credible set.
We repeated our analyses of this locus with the carotid plaque score PS, which we described in a previous work [7]. The region was nominally associated with PS, with lead SNP rs339671116 (p<10−5, see S4 Fig and S10 Table). Of note, this is the same SNP as detected as a single independent hit in women. However, this SNP does not display any sex-interaction. We repeated our credible set analyses conditioned on rs339671116, but the sets did not change, suggesting that rs201629990 and rs339671116 correspond to separate signals.
Gene expression lookup for 5q31.1
Since 5q31.1 displayed male-specific effects on CPA_mean, we created a candidate list of 29 nearby genes and 24 eQTL genes of all 24 SNPs in the 95% credible set (total n = 40 candidate genes). We could match 32 of them to high quality gene-expression probes including probes mapping to the same gene.
We tested these 32 probes for association with CPA_mean in all samples and in men and women separately. For men, we detected an association with IL5 and CCNI2. In women, GDF9 and P4HA2 reached nominal significance (see Table 3). However, these results were not robust to multiple testing. Comparing the effect sizes of those five genes in men and women, IL5 had a significantly greater effect size in men than in women (interaction p = 0.037). According to the GTex database, there are no eQTLs for IL5 probably due to a low expression except for testicular tissue (see S11 Table and S5 Fig).
Table 3. Probes associated with CPA_mean.
| INFO | COMBINED | MEN | WOMEN | Interaction | |||||
|---|---|---|---|---|---|---|---|---|---|
| Probe | Gene | Beta | P | Beta | P | Beta | P | Diff. | P |
| ILMN_1709300 | IL5 | 0.537 | 0.102 | 1.117 | 0.007 | -0.297 | 0.581 | 1.414 | 0.037 |
| ILMN_2184575 | CCNI2 | -0.555 | 0.080 | -1.028 | 0.011 | 0.047 | 0.927 | -1.074 | 0.097 |
| ILMN_1738783 | GDF9 | 0.237 | 0.502 | -0.517 | 0.265 | 1.161 | 0.031 | -1.677 | 0.018 |
| ILMN_2381697 | P4HA2 | 0.556 | 0.154 | 0.069 | 0.890 | 1.289 | 0.040 | -1.220 | 0.126 |
| ILMN_1730025 | ACSL6 | -0.627 | 0.082 | -0.924 | 0.045 | -0.136 | 0.814 | -0.788 | 0.286 |
Association was calculated under adjustment for percentages of lymphocytes, monocytes, and age. The combined setting was additionally adjusted for sex. The first two probes reached Bonferroni-adjusted significance (α = 0.0167 adjusting for three tests). For interaction analyses, effect sizes for men and women were compared.
CAD and cIMT look-up
We successfully verified six carotid plaque or cIMT SNPs and one CAD SNP (see S12 and S13 Tables) for association with Plaque burden. For the carotid SNPs, we did not detect more SNPs than would be expected by chance (binomial test, p = 0.045) and for CAD, we found less SNPs than expected by chance (binomial test, p = 0.005).
The PGS was only associated with CPS_max in the combined setting (see S14 Table). Interestingly, PGS was not associated with any CPB trait in men, but with all traits in women (α = 0.05). We performed a difference test on the sex-specific PGS effects, and found for both CPA_max and CPS_max significant female-specific effects. We checked our results with the aforementioned score PS (n = 6639; 3198 men & 3441 women), and found a similar trend: in women the association was more significant and the effect size was greater. However, the difference test here was not significant.
Discussion
Carotid plaque burden is an understudied subclinical trait of atherosclerosis due to its time-consuming and complicated assessment. Indeed, people at high risk for cardiovascular events can be identified by carotid ultrasound and steps for prevention be taken. Carotid plaque burden can then be used to control the progress of plaque formation.
To the best of our knowledge, there is only one other small GWAS in people of Hispanic ancestry that analyzed carotid plaque area similar to our trait CPA_sum [15] with focus on smoking interaction. However, no genome-wide significant associations were reported there. Atherosclerosis is known for its sexual dimorphism, i.e. men have a higher risk for coronary artery disease than women [9]. However, genetic reasons have not been described so far [8]. Here, we conducted a genome-wide study of CPB traits and compared the effect sizes of suggestive genetic loci for sex-interactions.
We detected an association at 5q31.1 with CPA_mean and CPA_max at genome-wide significance in men. Our sex-interaction analyses showed a significant difference in effect sizes for men and women. Chen et al. [54] had also analyzed this genetic region in context of schizophrenia, where they also detected male-specific associations. As a possible explanation, they named estrogen-response elements in this region, which would be in line with recent findings of steroid hormones influencing the risk of coronary artery disease [11].
The locus is rich in genes and we identified 23 candidates from our secondary analyses comprising credible set analysis, nearby gene annotation, eQTL look up and gene-expression association analysis. The most plausible candidate is IL5, whose gene-expression displayed the same male-specific effect on CPA_mean. IL5 is released by mast cells, which are involved in the development of many diseases [55]. Silveira et al. [56] had analyzed plasma IL5 and its effect on cIMT, and had found a protective effect of IL5 for women. However, since the gene expression association is not robust for multiple testing, we cannot completely rule out that other genes are responsible for the observed genetic association: the lead SNP is an eQTL of IRF1 antisense RNA. IRF1 expression is downregulated by estradiol [57] and reported for being associated with fibrinogen levels [50–52], which is a known risk factor for atherosclerosis in carotid arteries [46,58]. Also the Y-RNA, in which the lead SNP is located, is a potential candidate, as it is known to induce inflammation and to have a atherogenic effect [47,48].
We detected six other hits with suggestive significance, which were in or nearby plausible genes. The hit at 6q21 was in LD (r2 = 0.35) with a trans-eQTL of SELL [31], coding for l-selectin. Low levels of l-selectin were shown to be associated with carotid artery plaque size [59]. We detected an independent locus at 4q22.3 near BMPR1B, which is a receptor necessary for the signal transduction of BMP2–Smad1/5/8 signaling pathway, known for its association with vascular calcification [60]. Common genetic variants within BMPR1B have been reported for association with cIMT [61]. Further sex-specific hits were at 20q13.31 (associated in women, candidate gene TFAP2C, coding for estrogen receptor 1), 19q13.33 (associated in women, candidate gene FPR1, coding for a receptor for N-formyl-methionyl peptides. These neutrophil chemotactic factors activate polymorphonuclear neutrophils, which contribute to the pathogenesis and progression of atherosclerosis [62]), 2p12 (associated in women, candidate gene ABCC1, coding for an ATP-binding cassette, which are involved in cholesterol homeostasis and vascular inflammation [63], and 18q12.3 (associated in men, candidate gene PSTPIP2, which has been detected as differentially expressed gene in the atherosclerosis [64]). However, these associations require validation in larger studies or meta-analyses.
Previous family-studies estimated heritability of carotid plaque area at 69.1% (adjusted for sex and age) [65] and of carotid plaque prevalence at 50% (adj. for age, hypertension, diabetes, smoking, BMI, and WHR) [66]. We estimated the heritability using unrelated samples, and achieved similar results: adjusted for sex and age, we estimated about 49.7% and adjusted for all cardiovascular risk factors 70.5%. This increase can be explained by the reduction of noise: after adjustment on risk factors, 70.5% of the remaining variance can be explained by genetics.
Using our seven independent SNPs, we could explain about 6–12% of the CPBs variance, depending mainly on sex: for all traits the explained variance in women was larger than in men. This is complementary to the non-genetic model, in which the cardiovascular risk factors explained more variance in men than in women. Using the polygenic score for CAD [9], we found similar results, as the score was only associated in women, explaining about 1% variance. These results suggest that the genetic influence on atherosclerosis is stronger in women, whereas non-genetic factors like BMI are more relevant for men.
Interestingly, the same SNPs in the same multivariate model explained more variance for men than for women, although only one SNP showed a significant sex-interaction. This still applies when rs114597978 was removed from the model as a sensitivity test.
Our previously published study on genetics of carotid plaque showed significant enrichment of CAD loci with carotid plaques [7], and other studies revealed a genetic correlation of carotid plaques, cIMT, coronary heart disease and stroke [6]. However, we could not detect such an enrichment for our CPB traits. Regarding CAD SNPs, we even detected less significant variants than expected by chance. We also tested for an enrichment of cIMT and carotid plaque loci in our data, but again we found not more than expected by chance. This suggests a different genetic mechanism for plaque formation and its growth. This is in line with findings of Zeller et al. [13], who could only confirm one CAD locus for CAD severity. The same was observed for the risk of myocardial infarction in stable CAD patients, where significant differences in the effects on CAD onset and MI were found (personal communication).
A major limitation of our study is the small sample size for genome-wide analyses caused by the fact that the phenotype is difficult to obtain. This issue is even more severe for the sex-stratified analyses. Therefore, replication of our GWAS results in independent cohorts is necessary.
In conclusion, we analyzed traits of carotid plaque burden and detected a genome-wide significant hit at 5q31.1 for men only. The locus includes several estrogen response elements, suggesting a new link between steroid hormone regulation and atherosclerosis. However, verification of the causal gene at this region requires further analysis, taking gene-expression and estrogen regulation into account. Using all suggestive hits, we could explain 10% of the CPBs variance, while our estimated heritability was about 35%, suggesting genetic loci still undetected. Larger studies and meta-analyses are required to verify the suggested loci and to unravel the underlying molecular mechanisms.
Supporting information
For all analyses, spearman rank was calculated. P-values are given in the upper triangle, Spearmans rho in the lower triangle. Significant p-values are marked in red (p<0.05).
(XLSX)
Significant p-values are marked in red (p<0.05).
(XLSX)
For all six CPB traits, we estimated the heritability (h2) without any adjustment (univariate), with adjustment for sex and age (as in GWAS), and with adjustment for sex, age, BMI, hypertension, statin treatment, amoking and type 2 diabetes. Significant p-values are marked in red (p<0.05). Yellow marked p-values indicated a trend (p<0.1).
(XLSX)
Lead SNPs are marked green in column A. Suggestive significant associations are marked red in column M (p<3.33x10e-7). Results for all CPBs are given at the end.
(XLSX)
Lead SNPs are marked green in column A.
(XLSX)
Lead SNPs are marked green in column A.
(XLSX)
Lead SNPs are marked green in column A.
(XLSX)
Comparison of different models for all subjects (a, d, g), male subjects (b, e, h) and female subjects (c, f, i). In Tables a-c, single SNPs results are shown (CPB ~ SNP + …), with respect only to the top phenotype per SNP. In Tables d-f, all SNPs were analyzed together (CPB ~ SNP1 + SNP2 +… + SNP9), and in Tables g-i with additional adjustment for cardiovascular risk factors (CPB ~ SNP1 +…+ SNP9 + CV risk factors). Here, all traits were analyzed. Suggestive significant p-values are marked red (p<1E-6) and nominal sigificant p-values are marked yellow (p<0.05).
(XLSX)
Table a) We compared SNP effect sizes of men and women for all lead SNPs. Only the difference of effect of rs114597978 (cytoband 5q31.1) reached significance. Table b) We compared effect sizes of all SNPs at 5q31.1 for sex-interaction, sex-interaction within the elderly (older than 60 years) and interaction regarding statin treatment (in men only). Significant p-values are marked red (p<0.05).
(XLSX)
We listed all SNPs associated with PS or CPA_MEAN at at least suggestive level (p<1E-6). Association statistics of PS are taken from our previous publication (Pott et al. Genome-wide meta-analysis identifies novel loci of plaque burden in carotid artery. Atherosclerosis, 2017) and their newly analzed subgroups for men and women. There is no significant interaction for PS.
(XLSX)
Associations of all analyzed probes are shown.
(XLSX)
(XLSX)
(XLSX)
Significant results are marked in red (α = 0.05). Sample sizes are 1277 (757 men + 550 women) for the burden traits (CPAs and CPS) and 6639 (3198 men + 3441 women) for the plaque score PS.
(XLSX)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
We thank all study participants of the LIFE Adult study whose personal dedication and commitment have made this project possible. LIFE-Adult genotyping (round 3) was done at the Cologne Center for Genomics (CCG, University of Cologne, Peter Nürnberg and Mohammad R. Toliat). For LIFE-Adult genotype imputation, compute infrastructure provided by ScaDS (Dresden/Leipzig Competence Center for Scalable Data Services and Solutions) at the Leipzig University Computing Centre was used.
Data Availability
All summary statistics are available from the LHA database (No login is required). URL to our study: https://www.health-atlas.de/studies/37 URL to summary statistics: https://www.health-atlas.de/assays/31 Datafiles for CPA_max, CPA_sum, CPA_mean, CPS_max, CPS_sum, and CPS_mean: https://www.health-atlas.de/data_files/274https://www.health-atlas.de/data_files/275https://www.health-atlas.de/data_files/276https://www.health-atlas.de/data_files/277https://www.health-atlas.de/data_files/278https://www.health-atlas.de/data_files/279 Raw genetic data cannot be shared publicly because of consent restrictions of LIFE-Adult participants. Data are available after an approved project agreement from the LIFE Leipzig Research Center for Civilization Diseases. Please contact Dr. Matthias Nüchter (Head of Managing Office, contact via matthias.nuechter[at]life.uni-leipzig.de) for data access requests.
Funding Statement
LIFE-Adult is funded by the Leipzig Research Center for Civilization Diseases (LIFE). LIFE is an organizational unit affiliated to the Medical Faculty of the University of Leipzig. LIFE is funded by means of the European Union, by the European Regional Development Fund (ERDF) and by funds of the Free State of Saxony within the framework of the excellence initiative. JP was funded by the Federal Ministry of Education and Research (BMBF), Germany, FKZ: 01EO1501.AD2-7117 and a grant of the Medical Faculty of Leipzig (HIMAG-108, SAHSA). We acknowledge support from Leipzig University for Open Access Publishing. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kessler T, Erdmann J, Schunkert H. Genetics of Coronary Artery Disease and Myocardial Infarction—2013. Curr Cardiol Rep. 2013; 15: 933 10.1007/s11886-013-0368-0 [DOI] [PubMed] [Google Scholar]
- 2.Frieden TR, Berwick DM. The "Million Hearts" initiative—preventing heart attacks and strokes. N Engl J Med. 2011; 365: e27 10.1056/nejmp1110421 [DOI] [PubMed] [Google Scholar]
- 3.Weissgerber A, Scholz M, Teren A, Sandri M, Teupser D, Gielen S, et al. The value of noncoronary atherosclerosis for identifying coronary artery disease: results of the Leipzig LIFE Heart Study. Clin Res Cardiol. 2016; 105: 172–181. 10.1007/s00392-015-0900-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008; 21: 93–111; quiz 189–90. 10.1016/j.echo.2007.11.011 [DOI] [PubMed] [Google Scholar]
- 5.van der Harst P, Verweij N. Identification of 64 Novel Genetic Loci Provides an Expanded View on the Genetic Architecture of Coronary Artery Disease. Circ Res. 2018; 122: 433–443. 10.1161/CIRCRESAHA.117.312086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franceschini N, Giambartolomei C, Vries PS de, Finan C, Bis JC, Huntley RP, et al. GWAS and colocalization analyses implicate carotid intima-media thickness and carotid plaque loci in cardiovascular outcomes. Nat Commun. 2018; 9: 5141 10.1038/s41467-018-07340-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pott J, Burkhardt R, Beutner F, Horn K, Teren A, Kirsten H, et al. Genome-wide meta-analysis identifies novel loci of plaque burden in carotid artery. Atherosclerosis. 2017; 259: 32–40. 10.1016/j.atherosclerosis.2017.02.018 [DOI] [PubMed] [Google Scholar]
- 8.Loley C, Alver M, Assimes TL, Bjonnes A, Goel A, Gustafsson S, et al. No Association of Coronary Artery Disease with X-Chromosomal Variants in Comprehensive International Meta-Analysis. Sci Rep. 2016; 6: 35278 10.1038/srep35278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inouye M, Abraham G, Nelson CP, Wood AM, Sweeting MJ, Dudbridge F, et al. Genomic Risk Prediction of Coronary Artery Disease in 480,000 Adults: Implications for Primary Prevention. J Am Coll Cardiol. 2018; 72: 1883–1893. 10.1016/j.jacc.2018.07.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flynn E, Tanigawa Y, Rodriguez F, Altman RB, Sinnott-Armstrong N, Rivas MA. Sex-specific genetic effects across biomarkers; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pott J, Bae YJ, Horn K, Teren A, Kühnapfel A, Kirsten H, et al. Genetic association study of eight steroid hormones and implications for sexual dimorphism of coronary artery disease. J Clin Endocrinol Metab. 2019. 10.1210/jc.2019-00757 [DOI] [PubMed] [Google Scholar]
- 12.Dong C, Della-Morte D, Beecham A, Wang L, Cabral D, Blanton SH, et al. Genetic variants in LEKR1 and GALNT10 modulate sex-difference in carotid intima-media thickness: a genome-wide interaction study. Atherosclerosis. 2015; 240: 462–467. 10.1016/j.atherosclerosis.2015.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeller T, Seiffert M, Müller C, Scholz M, Schäffer A, Ojeda F, et al. Genome-Wide Association Analysis for Severity of Coronary Artery Disease Using the Gensini Scoring System. Front Cardiovasc Med. 2017; 4: 57 10.3389/fcvm.2017.00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983; 51: 606 10.1016/s0002-9149(83)80105-2 [DOI] [PubMed] [Google Scholar]
- 15.Della-Morte D, Wang L, Beecham A, Blanton SH, Zhao H, Sacco RL, et al. Novel genetic variants modify the effect of smoking on carotid plaque burden in Hispanics. J Neurol Sci. 2014; 344: 27–31. 10.1016/j.jns.2014.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loeffler M, Engel C, Ahnert P, Alfermann D, Arelin K, Baber R, et al. The LIFE-Adult-Study: objectives and design of a population-based cohort study with 10,000 deeply phenotyped adults in Germany. BMC Public Health. 2015; 15: 691 10.1186/s12889-015-1983-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thermo Fisher Scientific (02 September 2017. Axiom Genotyping Solution Data Analysis Guide (Pub. No. 702961 Rev. 5).
- 18.König IR, Loley C, Erdmann J, Ziegler A. How to include chromosome X in your genome-wide association study. Genet Epidemiol. 2014; 38: 97–103. 10.1002/gepi.21782 [DOI] [PubMed] [Google Scholar]
- 19.Consortium, The 1000 Genomes Project. A global reference for human genetic variation. Nature. 2015; 526: 68 10.1038/nature15393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Delaneau O, Howie B, Cox AJ, Zagury J-F, Marchini J. Haplotype estimation using sequencing reads. Am J Hum Genet. 2013; 93: 687–696. 10.1016/j.ajhg.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howie BN, Donnelly P, Marchini J. A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 2009; 5: e1000529 10.1371/journal.pgen.1000529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. [Google Scholar]
- 23.Yang J, Lee SH, Goddard ME, Visscher PM. GCTA: a tool for genome-wide complex trait analysis. Am J Hum Genet. 2011; 88: 76–82. 10.1016/j.ajhg.2010.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015; 4: 7 10.1186/s13742-015-0047-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaun Purcell CC. PLINK.
- 26.Zerbino DR, Achuthan P, Akanni W, Amode MR, Barrell D, Bhai J, et al. Ensembl 2018. Nucleic Acids Res. 2018; 46: D754–D761. 10.1093/nar/gkx1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buniello A, MacArthur JAL, Cerezo M, Harris LW, Hayhurst J, Malangone C, et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 2019; 47: D1005–D1012. 10.1093/nar/gky1120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Battle A, Brown CD, Engelhardt BE, Montgomery SB. Genetic effects on gene expression across human tissues. Nature. 2017; 550: 204–213. 10.1038/nature24277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joehanes R, Zhang X, Huan T, Yao C, Ying S-X, Nguyen QT, et al. Integrated genome-wide analysis of expression quantitative trait loci aids interpretation of genomic association studies. Genome Biol. 2017; 18: 16 10.1186/s13059-016-1142-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Westra H-J, Peters MJ, Esko T, Yaghootkar H, Schurmann C, Kettunen J, et al. Systematic identification of trans eQTLs as putative drivers of known disease associations. Nat Genet. 2013; 45: 1238–1243. 10.1038/ng.2756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xia K, Shabalin AA, Huang S, Madar V, Zhou Y-H, Wang W, et al. seeQTL: a searchable database for human eQTLs. Bioinformatics. 2012; 28: 451–452. 10.1093/bioinformatics/btr678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirsten H, Al-Hasani H, Holdt L, Gross A, Beutner F, Krohn K, et al. Dissecting the genetics of the human transcriptome identifies novel trait-related trans-eQTLs and corroborates the regulatory relevance of non-protein coding loci†. Hum Mol Genet. 2015; 24: 4746–4763. 10.1093/hmg/ddv194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu G, He Q-Y. ReactomePA: an R/Bioconductor package for reactome pathway analysis and visualization. Mol Biosyst. 2016; 12: 477–479. 10.1039/c5mb00663e [DOI] [PubMed] [Google Scholar]
- 34.Yu G, Wang L-G, Yan G-R, He Q-Y. DOSE: an R/Bioconductor package for disease ontology semantic and enrichment analysis. Bioinformatics. 2015; 31: 608–609. 10.1093/bioinformatics/btu684 [DOI] [PubMed] [Google Scholar]
- 35.Winkler TW, Justice AE, Cupples LA, Kronenberg F, Kutalik Z, Heid IM. Approaches to detect genetic effects that differ between two strata in genome-wide meta-analyses: Recommendations based on a systematic evaluation. PLoS ONE. 2017; 12: e0181038 10.1371/journal.pone.0181038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wakefield J. Bayes factors for genome-wide association studies: comparison with P-values. Genet Epidemiol. 2009; 33: 79–86. 10.1002/gepi.20359 [DOI] [PubMed] [Google Scholar]
- 37.Wakefield J. A Bayesian measure of the probability of false discovery in genetic epidemiology studies. Am J Hum Genet. 2007; 81: 208–227. 10.1086/519024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics. 2007; 8: 118–127. 10.1093/biostatistics/kxj037 [DOI] [PubMed] [Google Scholar]
- 39.Bis JC, Kavousi M, Franceschini N, Isaacs A, Abecasis GR, Schminke U, et al. Meta-analysis of genome-wide association studies from the CHARGE consortium identifies common variants associated with carotid intima media thickness and plaque. Nat Genet. 2011; 43: 940–947. 10.1038/ng.920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.López-Mejías R, Carmona FD, Genre F, Remuzgo-Martínez S, González-Juanatey C, Corrales A, et al. Identification of a 3'-Untranslated Genetic Variant of RARB Associated With Carotid Intima-Media Thickness in Rheumatoid Arthritis: A Genome-Wide Association Study. Arthritis & rheumatology (Hoboken, N.J.). 2019; 71: 351–360. 10.1002/art.40734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O'Donnell CJ, Cupples LA, D'Agostino RB, Fox CS, Hoffmann U, Hwang S-J, et al. Genome-wide association study for subclinical atherosclerosis in major arterial territories in the NHLBI's Framingham Heart Study. BMC Med Genet. 2007; 8 Suppl 1: S4 10.1186/1471-2350-8-S1-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shendre A, Wiener HW, Irvin MR, Aouizerat BE, Overton ET, Lazar J, et al. Genome-wide admixture and association study of subclinical atherosclerosis in the Women's Interagency HIV Study (WIHS). PLoS ONE. 2017; 12: e0188725 10.1371/journal.pone.0188725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shrestha S, Irvin MR, Taylor KD, Wiener HW, Pajewski NM, Haritunians T, et al. A genome-wide association study of carotid atherosclerosis in HIV-infected men. AIDS. 2010; 24: 583–592. 10.1097/QAD.0b013e3283353c9e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xie G, Myint PK, Voora D, Laskowitz DT, Shi P, Ren F, et al. Genome-wide association study on progression of carotid artery intima media thickness over 10 years in a Chinese cohort. Atherosclerosis. 2015; 243: 30–37. 10.1016/j.atherosclerosis.2015.08.034 [DOI] [PubMed] [Google Scholar]
- 45.Lambert Samuel A., Jupp Simon, Abraham Gad, Parkinson Helen, Danesh John, MacArthur Jacqueline A.L., et al. The Polygenic Score (PGS) Catalog: a database of published PGS to enable reproducibility and uniform evaluation; 2019. [Google Scholar]
- 46.Batagini NC, da Silva ES, Pinto CAV, Puech-Leão P, Luccia N de. Analysis of risk factors and diseases associated with atherosclerosis in the progression of carotid artery stenosis. Vascular. 2016; 24: 59–63. 10.1177/1708538115571404 [DOI] [PubMed] [Google Scholar]
- 47.Hizir Z, Bottini S, Grandjean V, Trabucchi M, Repetto E. RNY (YRNA)-derived small RNAs regulate cell death and inflammation in monocytes/macrophages. Cell Death Dis. 2017; 8: e2530 10.1038/cddis.2016.429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hizir Z, Trabucchi M, Repetto E. Valeur diagnostique des petits ARN dérivés des ARNY (ou RNY) dans les cardiopathies coronariennes. Med Sci (Paris). 2016; 32: 248–251. 10.1051/medsci/20163203008 [DOI] [PubMed] [Google Scholar]
- 49.Kichaev G, Bhatia G, Loh P-R, Gazal S, Burch K, Freund MK, et al. Leveraging Polygenic Functional Enrichment to Improve GWAS Power. Am J Hum Genet. 2019; 104: 65–75. 10.1016/j.ajhg.2018.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Danik JS, Paré G, Chasman DI, Zee RYL, Kwiatkowski DJ, Parker A, et al. Novel loci, including those related to Crohn disease, psoriasis, and inflammation, identified in a genome-wide association study of fibrinogen in 17 686 women: the Women's Genome Health Study. Circ Cardiovasc Genet. 2009; 2: 134–141. 10.1161/CIRCGENETICS.108.825273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sabater-Lleal M, Huang J, Chasman D, Naitza S, Dehghan A, Johnson AD, et al. Multiethnic meta-analysis of genome-wide association studies in 100 000 subjects identifies 23 fibrinogen-associated Loci but no strong evidence of a causal association between circulating fibrinogen and cardiovascular disease. Circulation. 2013; 128: 1310–1324. 10.1161/CIRCULATIONAHA.113.002251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vries PS de, Chasman DI, Sabater-Lleal M, Chen M-H, Huffman JE, Steri M, et al. A meta-analysis of 120 246 individuals identifies 18 new loci for fibrinogen concentration. Hum Mol Genet. 2016; 25: 358–370. 10.1093/hmg/ddv454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ellinghaus D, Jostins L, Spain SL, Cortes A, Bethune J, Han B, et al. Analysis of five chronic inflammatory diseases identifies 27 new associations and highlights disease-specific patterns at shared loci. Nat Genet. 2016; 48: 510–518. 10.1038/ng.3528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen X, Wang X, Hossain S, O'Neill FA, Walsh D, Pless L, et al. Haplotypes spanning SPEC2, PDZ-GEF2 and ACSL6 genes are associated with schizophrenia. Hum Mol Genet. 2006; 15: 3329–3342. 10.1093/hmg/ddl409 [DOI] [PubMed] [Google Scholar]
- 55.Dumitraşcu D. Mast cells as potent inflammatory cells. Rom J Intern Med. 1996; 34: 159–172. [PubMed] [Google Scholar]
- 56.Silveira A, McLeod O, Strawbridge RJ, Gertow K, Sennblad B, Baldassarre D, et al. Plasma IL-5 concentration and subclinical carotid atherosclerosis. Atherosclerosis. 2015; 239: 125–130. 10.1016/j.atherosclerosis.2014.12.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lengi AJ, Phillips RA, Karpuzoglu E, Ahmed SA. 17beta-estradiol downregulates interferon regulatory factor-1 in murine splenocytes. J Mol Endocrinol. 2006; 37: 421–432. 10.1677/jme.1.02122 [DOI] [PubMed] [Google Scholar]
- 58.Bots ML, Breslau PJ, Briët E, Bruyn AM de, van Vliet HH, van den Ouweland FA, et al. Cardiovascular determinants of carotid artery disease. The Rotterdam Elderly Study. Hypertension. 1992; 19: 717–720. 10.1161/01.HYP.19.6.717 [DOI] [PubMed] [Google Scholar]
- 59.Andersson J, Sundström J, Kurland L, Gustavsson T, Hulthe J, Elmgren A, et al. The carotid artery plaque size and echogenicity are related to different cardiovascular risk factors in the elderly: the Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study. Lipids. 2009; 44: 397–403. 10.1007/s11745-009-3281-y [DOI] [PubMed] [Google Scholar]
- 60.Wang S, Hu S, Wang J, Liu Y, Zhao R, Tong M, et al. Conditioned medium from bone marrow-derived mesenchymal stem cells inhibits vascular calcification through blockade of the BMP2-Smad1/5/8 signaling pathway. Stem Cell Res Ther. 2018; 9: 160 10.1186/s13287-018-0894-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu Y-J, Lee Y-N, Wu T-W, Chou C-L, Wang L-Y. Common Genetic Variants on Bone Morphogenetic Protein Receptor Type IB (BMPR1B) Gene Are Predictive for Carotid Intima-Media Thickness. Circ J. 2019; 83: 749–756. 10.1253/circj.CJ-18-1046 [DOI] [PubMed] [Google Scholar]
- 62.Marino F, Tozzi M, Schembri L, Ferraro S, Tarallo A, Scanzano A, et al. Production of IL-8, VEGF and Elastase by Circulating and Intraplaque Neutrophils in Patients with Carotid Atherosclerosis. PLoS ONE. 2015; 10: e0124565 10.1371/journal.pone.0124565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schumacher T, Benndorf RA. ABC Transport Proteins in Cardiovascular Disease-A Brief Summary. Molecules. 2017; 22 10.3390/molecules22040589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu L, Liu Y, Liu C, Zhang Z, Du Y, Zhao H. Analysis of gene expression profile identifies potential biomarkers for atherosclerosis. Mol Med Rep. 2016; 14: 3052–3058. 10.3892/mmr.2016.5650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tarnoki AD, Baracchini C, Tarnoki DL, Lucatelli P, Boatta E, Zini C, et al. Evidence for a strong genetic influence on carotid plaque characteristics: an international twin study. Stroke. 2012; 43: 3168–3172. 10.1161/STROKEAHA.112.666016 [DOI] [PubMed] [Google Scholar]
- 66.Dong C, Beecham A, Slifer S, Wang L, Blanton SH, Wright CB, et al. Genomewide linkage and peakwide association analyses of carotid plaque in Caribbean Hispanics. Stroke. 2010; 41: 2750–2756. 10.1161/STROKEAHA.110.596981 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For all analyses, spearman rank was calculated. P-values are given in the upper triangle, Spearmans rho in the lower triangle. Significant p-values are marked in red (p<0.05).
(XLSX)
Significant p-values are marked in red (p<0.05).
(XLSX)
For all six CPB traits, we estimated the heritability (h2) without any adjustment (univariate), with adjustment for sex and age (as in GWAS), and with adjustment for sex, age, BMI, hypertension, statin treatment, amoking and type 2 diabetes. Significant p-values are marked in red (p<0.05). Yellow marked p-values indicated a trend (p<0.1).
(XLSX)
Lead SNPs are marked green in column A. Suggestive significant associations are marked red in column M (p<3.33x10e-7). Results for all CPBs are given at the end.
(XLSX)
Lead SNPs are marked green in column A.
(XLSX)
Lead SNPs are marked green in column A.
(XLSX)
Lead SNPs are marked green in column A.
(XLSX)
Comparison of different models for all subjects (a, d, g), male subjects (b, e, h) and female subjects (c, f, i). In Tables a-c, single SNPs results are shown (CPB ~ SNP + …), with respect only to the top phenotype per SNP. In Tables d-f, all SNPs were analyzed together (CPB ~ SNP1 + SNP2 +… + SNP9), and in Tables g-i with additional adjustment for cardiovascular risk factors (CPB ~ SNP1 +…+ SNP9 + CV risk factors). Here, all traits were analyzed. Suggestive significant p-values are marked red (p<1E-6) and nominal sigificant p-values are marked yellow (p<0.05).
(XLSX)
Table a) We compared SNP effect sizes of men and women for all lead SNPs. Only the difference of effect of rs114597978 (cytoband 5q31.1) reached significance. Table b) We compared effect sizes of all SNPs at 5q31.1 for sex-interaction, sex-interaction within the elderly (older than 60 years) and interaction regarding statin treatment (in men only). Significant p-values are marked red (p<0.05).
(XLSX)
We listed all SNPs associated with PS or CPA_MEAN at at least suggestive level (p<1E-6). Association statistics of PS are taken from our previous publication (Pott et al. Genome-wide meta-analysis identifies novel loci of plaque burden in carotid artery. Atherosclerosis, 2017) and their newly analzed subgroups for men and women. There is no significant interaction for PS.
(XLSX)
Associations of all analyzed probes are shown.
(XLSX)
(XLSX)
(XLSX)
Significant results are marked in red (α = 0.05). Sample sizes are 1277 (757 men + 550 women) for the burden traits (CPAs and CPS) and 6639 (3198 men + 3441 women) for the plaque score PS.
(XLSX)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All summary statistics are available from the LHA database (No login is required). URL to our study: https://www.health-atlas.de/studies/37 URL to summary statistics: https://www.health-atlas.de/assays/31 Datafiles for CPA_max, CPA_sum, CPA_mean, CPS_max, CPS_sum, and CPS_mean: https://www.health-atlas.de/data_files/274https://www.health-atlas.de/data_files/275https://www.health-atlas.de/data_files/276https://www.health-atlas.de/data_files/277https://www.health-atlas.de/data_files/278https://www.health-atlas.de/data_files/279 Raw genetic data cannot be shared publicly because of consent restrictions of LIFE-Adult participants. Data are available after an approved project agreement from the LIFE Leipzig Research Center for Civilization Diseases. Please contact Dr. Matthias Nüchter (Head of Managing Office, contact via matthias.nuechter[at]life.uni-leipzig.de) for data access requests.