Abstract
The Africanised honey bee, vernacularly known as the ‘killer bee’, is a hybrid of the western honey bee species. These bees tend to be more aggressive with a greater tendency for swarm formation. Their stings are frequently encountered with a broad spectrum of clinical manifestations, ranging from local to systemic effects, even with recorded fatalities. We report a case of an elderly man, who experienced a cerebrovascular event confirmed by neuroimaging within 24 hours after a multitude of Africanised honey bee stings.
Keywords: stroke, toxicology
Background
The Africanised honey bee (hybrids of European-African honey bees) are now a public health hazard. They are produced by crossbreeding the East African lowland honey bee with various European honey bees. The inadvertent release from Brazilian breeding hives has led to a northern migration pattern, hence the presence of these bee colonies in the Southern Caribbean.
These crossbred honey bees have been farmed for honey to produce higher yields.1 Despite increased honey production, the behaviour of this particular hybrid differs from its predecessors, as they tend to be more aggressive and likely to attack in large numbers resulting in envenomation with higher concentrations of vasoactive venom constituents.1 2
These attacks can precipitate anaphylaxis, renal injury, cardiovascular and cerebrovascular events, even culminating in death.3 4 Herein, we describe a rare case of ischaemic stroke as a subacute phenomenon after a plethora of bee stings within a 24-hour period.
Case presentation
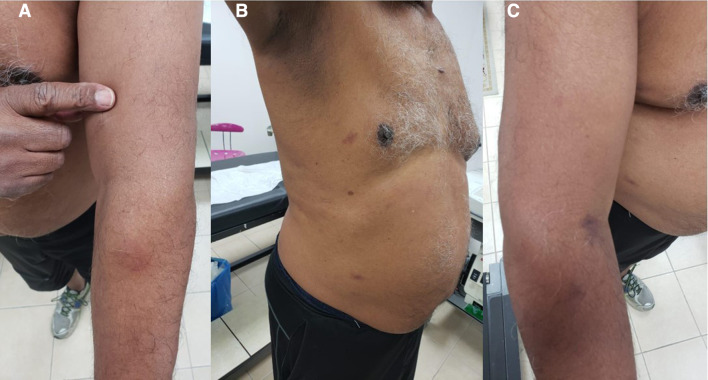
A 70-year-old South Asian man with no significant medical history was jogging through a mountainous, northern region of Trinidad (Caribbean island) when he became abruptly engulfed by an Africanised honey bee swarm. He experienced at least 50–100 stings throughout his body, including his face, forearms and upper shoulders and back (see figure 1A–C), even through his clothed, unexposed areas. He was initially managed as an outpatient with oral antihistamine and steroid therapies and subsequently returned to his usual activities the same day. Approximately 24 hours later, he experienced sudden right-sided weakness, resulting in a mechanical fall as well as an expressive dysphasia. On physical examination, his vital signs and cardiorespiratory assessment were normal, however neurologically, he did display a mild right hemiparesis, more so in the lower extremity. He also had a subtle expressive dysphasia, for example, calling a pedestal fan, an air conditioner. There were no other pertinent neurovascular findings.
Figure 1.
Local dermatological effects of Africanised honey bee stings, displaying wheals, with surrounding erythema and induration. (A) Sting on the left flexor forearm with induration. (B) Stings located on the anterolateral chest wall and lower abdomen. (C) Sting on the right upper arm. Local dermatologic effects of several bee stings, displaying wheals, with surrounding erythema, and induration.
Investigations
An initial MRI scan with dedicated diffusion weighted imaging and apparent diffusion weighted imaging sequences of his brain ascertained the presence of a left hemispheric ischaemic stroke (see figure 2).
Figure 2.
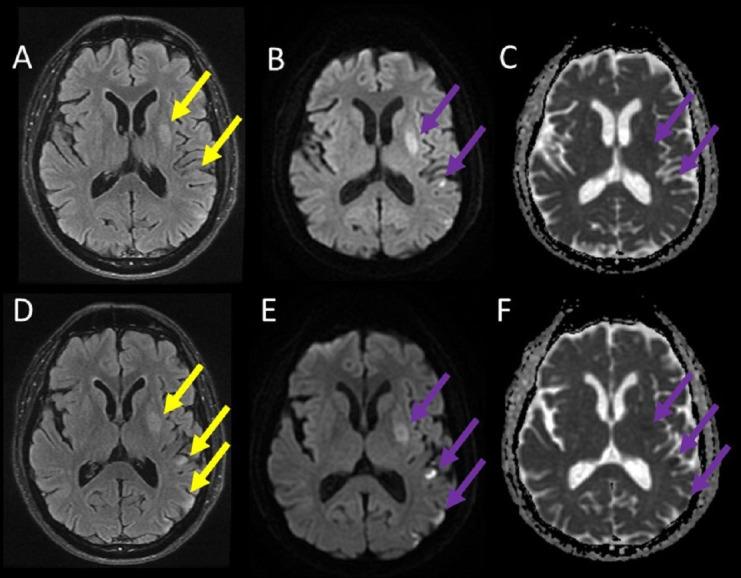
MRI of the brain. Images (A) and (D) demonstrate a hyperintensity signal on T2 sequences, affecting areas of the left parietal lobe and left basal ganglia (yellow arrows). Images (B) and (E) also demonstrate a hyperintensity signal on diffusion-weighted images (expected in acute cerebrovascular events) and respective hypointensity signal in the apparent diffusion coefficient images (C) and (F) (purple arrows).
Routine laboratory investigations including glycosylated haemoglobin, fasting lipid panel were normal. Cardiovascular investigations such as a 12-lead ECG, 24-hour Holter monitoring, two-dimensional transthoracic echocardiography and carotid duplex ultrasonography were all unremarkable. Thrombophilia, rheumatological and immunological screens, as well as a two-dimensional transoesophageal echocardiogram, were not performed. Table 1 summarises the results of his routine stroke investigations.
Table 1.
Summary of the routine stroke investigations, cardiovascular investigations and MRI, magnetic resonance angiography
| Investigation | Comment |
| Blood investigations—HbA1c, fasting lipid profile | Normal. |
| Carotid Doppler ultrasonography scan | No plaque formation was seen in the right and left carotid arteries, with normal flow velocities. |
| Two-dimensional transthoracic echocardiogram | Normal left ventricular systolic function with an estimated ejection fraction of 60%–65%, normal valvular function and type one diastolic dysfunction. There were no visible atheromas in the ascending aorta. |
| 12-lead ECG | Normal sinus rhythm with no acute dynamic changes consistent with ischaemia or infarction. |
| 24-hour Holter monitor | Normal sinus rhythm with no significant arrhythmias such as atrial fibrillation, ventricular tachycardia or advanced heart block. |
| MRI of the brain magnetic resonance angiography (MRA) of the brain |
Left basal ganglia (lentiform nucleus) and left parietal cortical infarct, left middle cerebral artery territory infarction suggestive of an embolic aetiology. On the MRA sequence, normal calibre and contour of the internal carotid and basilar arteries with normal flow were demonstrated in the anterior cerebral, middle cerebral and posterior cerebral vessels. |
Differential diagnosis
The most likely diagnosis was an ischaemic stroke, which was subsequently confirmed by the MRI and temporally linked with the bee stings. Other tentative diagnoses such as encephalitis and seizure disorder were summarily dismissed as the clinical presentation was not consistent with either of these scenarios nor compatible with the MRI interpretation.
Treatment
After establishing the diagnosis, the patient was immediately initiated on high-dose aspirin (325 mg) and continued oral antihistamine and steroid therapies for a delayed postenvenomation reaction for 10 days, after which he was transitioned to low dose aspirin (81 mg). He did not require other rehabilitative services such as speech and swallow therapy, as well as physiotherapy due to his rapid, complete neurological recovery.
Outcome and follow-up
The patient’s stroke symptomatology quickly resolved after the index event (within a few hours), and he returned to his activities of daily living by the following day. He also resumed his jogging within a week. A routine follow-up appointment 6 months later affirmed a complete neurological recovery.
Discussion
The order, Hymenoptera, is composed of stinging insects including bees, wasps and yellow jackets. Honey bees live in well-organised communities and receive much attention due to the severe attacks these insects can initiate.5
There are several postulated mechanisms that account for the clinical manifestation of Hymenoptera envenomation. Severe hypersensitivity syndromes and anaphylaxis tend to occur with an estimated incidence of 1%–5%. These reactions have been linked to the interleukin and cytokine ‘storm’, after severe envenomation (usually observed after 50–100 bee stings).6 Negative prognosticators for fatal or severe allergic reactions are age of less than 20 years and male gender.7 Our patient did not display the clinical trajectory of anaphylaxis with refractory hypotension, despite the seemingly incalculable amount of venom injected. Our patient exhibited classic stroke symptomatology with focal neurological deficits. Other enigmatic syndromes can manifest such trigeminal neuralgia, myasthenia gravis, Guillain-Barré syndrome, parkinsonism, intracerebral haemorrhages; often with devastating complications.7 8 Other authors have described similar cerebrovascular events; however, the index event ensued almost an entire day after the swarm attack, whereas previous strokes appeared chronologically earlier (within a few hours). At the time of publication, the literature has described only 15 similar cases of Africanised honey bee sting-induced strokes worldwide, none of which hailed from the Caribbean region. The majority were, in fact, similar to our case, with ischaemic strokes being the predominant aetiology.9–11 In our patient, the left middle cerebral artery was involved as the culprit vessel; however, it has been reported that other perfused territories may also be affected. Currently, there is no evidence to suggest whether a particular vascular territory is more susceptible to the effects of envenomation.
The pathophysiology of these strokes is complex and multifactorial, including vascular thromboembolic phenomenon, refractory hypotension with hypoxemia, malignant hypertension with resultant haemorrhage, arrhythmias, hypercoagulability and immune hyper-reactivity. Bee venom contains several humoral vasoactive mediators such as histamine, serotonin, thromboxanes and leukotrienes, and as a result, this endogenous milieu can induce vasoconstriction, augmented by exogenous epinephrine and platelet aggregation. There are also direct toxic effects of bee venom, mediated by polypeptide toxins (melittin), which damages cell membranes and hyaluronidase, phospholipase enzymes.10 11 We suspect that our patient experienced an ischaemic event as a result of a hypersensitivity reaction to vasoactive amines with activation of the coagulation system by venom constituents, as well as severe transient vasoconstriction.
Learning points.
This article highlights a rare case of an ischaemic stroke occurring after extensive Hymenoptera envenomation by Africanised honey bees.
Africanised honey bee envenomation can precipitate ischaemic strokes as a delayed phenomenon.
The pathophysiology of Hymenoptera envenomation is not fully elucidated and likely attributed to several mechanisms such as transient vasoconstriction, thrombophilia and arrhythmias.
Emergency management guidelines and strategies should be instituted with an insightful approach in anticipating and mitigating catastrophic sequelae. It is prudent not to overlook these rare but fatal effects.
Footnotes
Contributors: AFR was involved with the early management of this patient and wrote the original manuscript. NS was involved with preforming all cardiology investigations and the editing of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Marques MRdeV, Araújo KAMde, Tavares AV, et al. Epidemiology of envenomation by Africanized honeybees in the state of Rio grande do Norte, northeastern Brazil. Rev Bras Epidemiol 2020;23:e200005. 10.1590/1980-549720200005 [DOI] [PubMed] [Google Scholar]
- 2.Ferreira RS, Almeida RAMB, Barraviera SRCS, et al. Historical perspective and human consequences of Africanized bee stings in the Americas. J Toxicol Environ Health B Crit Rev 2012;15:97–108. 10.1080/10937404.2012.645141 [DOI] [PubMed] [Google Scholar]
- 3.Gupta PN, Kumar BK, Velappan P, et al. Possible complication of bee stings and a review of the cardiac effects of bee stings. BMJ Case Rep 2016:pii: bcr2015213974 10.1136/bcr-2015-213974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes RL. A fatal case of acute renal failure from envenoming syndrome after massive bee attack: a case report and literature review. Am J Forensic Med Pathol 2019;40:52-57–7. 10.1097/PAF.0000000000000451 [DOI] [PubMed] [Google Scholar]
- 5.Fan HW, Kalil J. Massive bee envenomation. Critical Care Toxicology 2017:2627–36. [Google Scholar]
- 6.Bourgain C, Pauti MD, Fillastre JP, et al. [Massive poisoning by African bee stings]. Presse Med 1998;27:1099–101. [PubMed] [Google Scholar]
- 7.Kalyoncu AF, Demir AU, Ozcan U, Fuat Kalyoncu A, Uğur Demir A, et al. Bee and wasp venom allergy in turkey. Ann Allergy Asthma Immunol 1997;78:408–12. 10.1016/S1081-1206(10)63203-6 [DOI] [PubMed] [Google Scholar]
- 8.Dikici S, Aydin LY, Saritas A, et al. An unusual presentation of bee sting: subarachnoid hemorrhagia. Am J Emerg Med 2012;30:1663.e5–1663.e6. 10.1016/j.ajem.2011.09.012 [DOI] [PubMed] [Google Scholar]
- 9.Jain J, Banait S, Srivastava AK, et al. Stroke intracerebral multiple infarcts: rare neurological presentation of honey bee bite. Ann Indian Acad Neurol 2012;15:163. 10.4103/0972-2327.95008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crawley F, Schon F, Brown MM. Cerebral infarction: a rare complication of wasp sting. J Neurol Neurosurg Psychiatry 1999;66:550–1. 10.1136/jnnp.66.4.550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riggs JE, Ketonen LM, Wymer JP, et al. Acute and delayed cerebral infarction after wasp sting anaphylaxis. Clin Neuropharmacol 1994;17:384. 10.1097/00002826-199408000-00011 [DOI] [PubMed] [Google Scholar]