Abstract
Objective:
To explore racial/ethnic differences in satisfaction with wait time of scheduled office visits by comparing electronic health record (EHR)-based, patient-reported, and patient satisfaction with wait time
Study Setting:
A large multispecialty ambulatory care organization in Northern California. Patient experience surveys were collected between 2010 and 2014. Surveys were mailed after randomly selected nonurgent visits. Returned survey data were linked to EHR data for surveyed visits.
Study Design:
Observational, retrospective study designed to assess differences in patient-reported wait time, wait-time satisfaction, and actual EHR-recorded wait time with respect to self-reported race/ethnicity. Multivariate regression models with provider random effects were used to evaluate differences.
Results:
Asian subgroups (Chinese, Asian Indian, Filipino, Japanese, Korean, and Vietnamese) and Latinos gave poorer ratings for wait time than non-Hispanic whites (NHWs). The average wait time reported by Asians was longer than that reported by NHWs. On the basis of EHR data, however, no minority group was likely to wait longer, and all, except for Japanese (10%), were more likely to be late for the appointment (16%: Filipino and 23%: Asian Indian), than NHWs (13%).
Conclusions:
Given actual wait times, Asians perceive longer wait time and were less satisfied with wait times. Asians may have different expectations about wait time at the clinic.
Keywords: patient satisfaction, wait time, outpatient care, racial/ethnic differences
Timeliness of care is a key pillar of healthcare quality and an important determinant of patient satisfaction.1,2 Despite this, relatively little attention has been paid to the metric of wait time in the health care setting. The exception is wait time in the emergency room, which has been studied largely because of the clinical ramifications of delayed care in this setting.3,4 Little is known about wait time for scheduled office visits, where timeliness matters less for clinical outcomes than it does for patient satisfaction. Wait time experience, however, can color patient’s overall experience about the visit. Leddy et al5 found that wait time explains 40% of the variance in overall patient ratings of office visits. Given increasing emphasis on patient experience of care as an important measure of patient-centered outcomes, further studies are needed to better understand patient experiences of wait time in ambulatory-care settings, how patients rate such experiences, and how experiences differ across specific groups.1,6
Although no one is pleased with having to wait, certain subgroups report lower satisfaction with wait time. Studies have shown that females and younger patients are less satisfied with longer wait times than males and older patients.4,5 In general, practices in the United Kingdom Asians have been shown to give poorer evaluations of wait time than whites.7 Studies to date have used patient-reported measures of wait time and satisfaction only.
In this study, we sought to evaluate differences in satisfaction with wait time across diverse racial/ethnic groups, and to assess factors that modify this relationship, including arrival time, actual wait time, and perceived wait time. For this analysis, we had the opportunity to use workflow time stamps in the electronic health records (EHRs) to compare actual wait time with patient-reported wait time and satisfaction with wait time.
METHODS
Setting and Study Design
This study was conducted at a large ambulatory-care organization in Northern California. The organization contracts with >1000 physicians and provides care for >1 million patients. The patient population is highly insured (98%) and thus underrepresents the medically underserved; however, in this setting, racial/ethnic comparisons are less likely to be confounded by differences in access to health care.
Study Sample
The patient experience of care survey data (2010–2014) was linked to EHR data for each surveyed encounter, and relevant patient and provider characteristics. All data were deidentified for research purposes, and the study was approved by the organization’s Institutional Review Board.
We used surveys from the following self-reported racial/ethnic groups: non-Hispanic/Latino white (NHW), non-Hispanic/Latino black (black), Hispanic/Latino, and Asian subgroups (Chinese, Asian Indian, Filipino, Japanese, Korean, and Vietnamese) with valid information on some wait time measures (N = 239,074). When there were multiple surveys from a patient to a specific provider, the most recent response of the patient-provider pair was used for the analysis, excluding 39,952 (16.7%) preceding responses. Surveys returned >6 months after the visit (n = 708; 0.36%) and surveys with patient-reported wait time >2 hours after scheduled time (n = 35; 0.02%) were excluded to ensure validity of the answers. Total 198,379 surveys were included in the analyses. Given that surveys to patients age less than 18 are likely completed by a parent/guardian, we ran separate analyses for pediatric versus adult visits; however, results for the 2 groups were almost identical (Appendix Table 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B81). Similarly, there was no difference in overall results between primary care visits (43.1%) and specialty visits. Thus, surveys on all office visits were combined in the main analysis.
Patient-reported Wait Time and Wait Time Satisfaction
The medical group has been conducting patient experience of care surveys for quality improvement purposes via an external survey organization Press-Ganey (http://www.press-ganey.com). Surveys are randomly sent to patients via mail following scheduled visits, with an average of 30 returned surveys per provider per 6 months. The survey queries patients’ experiences during a recent health care encounter. Overall response rate was 20%, which is comparable to rates of mail-only patient surveys reported elsewhere,8 and varied by patient demographics as reported in other settings (eg, higher for NHWs than minority groups).8–14 We examined whether racial/ethnic differences in response rates would potentially influence our results.
Duration of wait time in the waiting area is queried in the survey with an open-ended question: “How many minutes did you wait after your scheduled appointment time before you were called to an exam room?” The survey then instructs respondents to: “Please rate the services you received from our practice….” One of service aspects asked was: “Wait time at clinic (from arriving to leaving).” Respondents are asked to rate their experience as: very poor, poor, fair, good, or very good. Most respondents chose “very good” (52%), followed by good (35%), fair (10%), poor (2%), and very poor (1%).
EHR-based Wait Time Indicators
For each visit on which a patient survey was based, we extracted time stamp data from the EHR to compute patient’s time in the waiting area (Fig. 1). By comparing patient’s arrival time to scheduled time, we created an indicator of “late arrival.” EHR-based “wait time (postscheduled appointment time) in the waiting area” is defined as elapsed time between scheduled appointment time or patient check-in time (later of the 2) and the time a patient’s vitals were recorded. We expect our EHR-based wait time to be consistently a few minutes longer than the actual time in the waiting area because vital measures are typically recorded 1–2 minutes after the patient enters to the examination room. The variable “early entrance to exam room” indicates that the patient arrived early and entered the examination room (ie, vitals entered) before scheduled appointment time.
FIGURE 1.
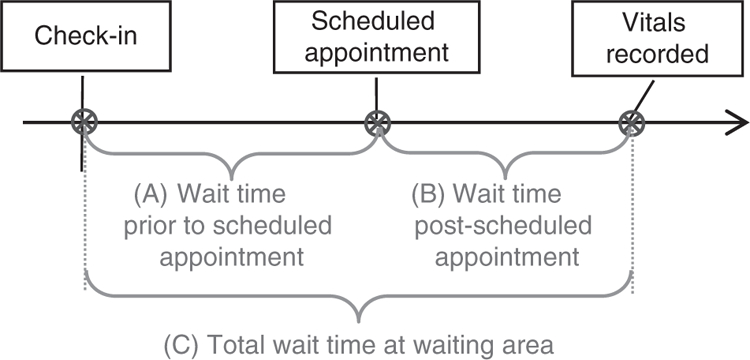
Definitions of EHR-based wait time outcomes in a typical scenario. A, Time before scheduled appointment = time from patient checked-in with receptionist to scheduled appointment time. B, Time after scheduled appointment = time from scheduled appointment time (or check-in time if a patient arrives late) to when vitals were recorded in the EHR by a nurse or medical assistant. C, Total wait time in waiting area = time between check-in and vitals recorded. EHR indicates electronic health record.
Finally, based on all the clinic visits a patient made in the year before the surveyed visit, we created variables indicating proportion of “late” visits (ie, checked-in after scheduled time) and proportion of “arrived too early” visits (ie, checked-in >15 min before scheduled time).
Visit Characteristics
We extracted from the EHR information on visit characteristics that may be relevant to wait time and wait time satisfaction, which includes time of visit, categorized as early morning (6 am–9:59 am), late morning (10 am–11:59 am), early afternoon (12 pm–2:59 pm), and late afternoon (3 pm–8:59 pm); long appointment (scheduled visit length is ≥30 min vs. 5–29 min); recency of visit (number of days between visit and survey return); visit type (preventive, visit for an acute condition, visit for a chronic condition); seeing one’s own primary care provider (PCP); and the number of years with the PCP.15 On the basis of the patient’s and provider’s race/ethnicity, and patient’s preferred language and provider’s proficiency in the language, we defined the visit to be “racial/ethnic concordant” (vs. discordant) and “language concordant as non-English” or “language discordant” (vs. language concordant as English).
Statistical Methods
Wait time measures, visit characteristics, and patient characteristics were compared across racial/ethnic groups, by pairwise χ2 tests and t tests as appropriate. Multivariate regression analyses were conducted to assess the relationship between patient-reported wait time and wait time satisfaction and patient race/ethnicity, with statistical adjustment for covariates. In addition to the covariates described above, patient age, sex, and insurance type, and provider’s years of medical practice, sex, clinic site, and specialty were also included. We included random effects for providers to account for multiple patient observations within each provider. In addition, several sensitivity analyses were performed to ensure the robustness of the findings. We considered between-group differences statistically significant when P < 0.001. All statistical analyses were performed using STATA 13.1.
RESULTS
Summary of Wait Time Measures and Patient and Visit Characteristics
Among 198,379 surveyed visits included, 71.2% were from NHW respondents (Table 1). A majority (52%) responded “very good” to the questions on satisfaction with wait time, and average patient-reported wait time in the waiting area was 8.4 minutes. On the basis of EHR time stamps, patients waited in the waiting area for an average of 9.2 minutes after scheduled time. Fourteen percent of patients arrived late for their appointment. See Table 1 for summary of other patient and visit characteristics.
TABLE 1.
Wait Time Measures and Visit, Patient, and Provider Characteristics: Comparison by Patient Race/Ethnicity†
| Variables‡ | Overall | NHW | Hispanic/Latino | Black | Chinese | Asian Indian | Filipino | Japanese | Korean | Vietnamese |
|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | 198,379 | 141,214 (71.2) | 17,495 (8.8) | 2862 (1.4) | 15,566 (7.9) | 10,049 (5.1) | 5037 (2.5) | 3651 (1.8) | 1356 (0.7) | 1149 (0.6) |
| Patient-reported wait time and rating | ||||||||||
| Satisfaction: very good (N = 158,647) (%) | 52.1 | 55.4 | 52.9* | 53.7 | 37.7* | 36.8* | 44.9* | 44.1* | 37.1* | 39.7* |
| Postscheduled time at waiting area in minute (0–120) (N = 126,058) | 8.4 (9.9) | 8.1 (9.9) | 9.2 (10.6)* | 9.1 (9.7)* | 8.8 (9.5)* | 9.1 (9.8)* | 9.7 (9.4)* | 8.4 (9.0) | 8.6 (8.6) | 10.3 (11.8)* |
| EHR-based scheduled, arrived, and wait time indicators | ||||||||||
| Arrived late (N = 117,581) (%) | 14.3 | 12.7 | 17.8* | 17.7* | 18.2* | 23.0* | 16.0* | 9.7* | 17.7* | 18.3* |
| Time (postscheduled time) at waiting area (0–120) (N = 101,827) | 9.2 (11.5) | 9.3 (11.6) | 9.3 (11.3) | 9.5 (10.8) | 8.9 (11.1) | 9.0 (10.6) | 8.9 (11.0) | 9.0 (12.1) | 8.2 (10.2) | 9.3 (12.7) |
| Led to examination room before the scheduled time (N = 102,445) (%) | 16.8 | 16.7 | 17.9 | 16.2 | 16.5 | 15.3* | 20.0* | 17.9 | 20.2 | 18.6 |
| Long visit (scheduled for 30+ min) (%) | 65.7 | 66.9 | 60.8* | 65.2 | 65.6 | 60.1* | 62.6* | 67.2 | 63.2 | 62.1 |
| Visit time of the day (N = 118,137) | ||||||||||
| Early morning (6:00–9:59) (%) | 22.6 | 22.3 | 21.6* | 21.0 | 26.0* | 23.6* | 21.6 | 24.8 | 23.2 | 21.6 |
| Mid-morning (10:00–11:59) (%) | 28.8 | 29.2 | 28.1* | 30.5 | 27.3 | 26.6 | 28.6 | 29.8 | 32.0* | 27.3 |
| Early afternoon (12:00–14:59) (%) | 26.5 | 27.1 | 25.7* | 26.8 | 24.3 | 24.7 | 26.4 | 24.5 | 23.1 | 26.8 |
| Late afternoon (15:00–20:59) (%) | 22.1 | 21.4 | 24.6* | 21.7 | 22.4* | 25.1* | 23.4* | 21.0 | 21.7 | 24.3 |
| Other visit characteristics | ||||||||||
| Days between visit and survey return (11–183) | 29.7 (18.1) | 28.9 (17.2) | 31.4 (19.9)* | 33.2 (22.2)* | 30.1 (17.9)* | 34.5 (23.0)* | 32.9 (21.2)* | 29.4 (17.9) | 30.6 (18.1) | 31.6 (20.3)* |
| Primary care visit (%) | 42.3 | 38.3 | 48.7* | 40.6 | 54.4* | 62.4* | 51.4* | 40.9 | 58.3* | 57.3* |
| Own primary care physician visit (%) | 31.6 | 28.5 | 35.0* | 30.2 | 42.1* | 47.4* | 39.2* | 30.7 | 43.7* | 43.2* |
| No. years with the PCP | 2.6 (3.5) | 2.7 (3.6) | 2.1 (3.0)* | 3.0 (3.9) | 2.6 (3.3) | 2.0 (2.7)* | 2.5 (3.3)* | 2.8 (3.6) | 1.8 (2.8)* | 2.1 (3.0)* |
| Preventive visit (%) | 13.9 | 11.5 | 15.6* | 11.3 | 24.1* | 23.6* | 17.9* | 15.0* | 25.1* | 23.3* |
| Visit for chronic condition (%) | 23.8 | 24.9 | 22.2* | 29.5* | 19.5* | 17.6* | 25.0 | 24.5 | 16.2* | 19.2* |
| Patient-provider race/ethnicity concordant (%) | 54.1 | 69.4 | 4.4* | 2.3* | 36.8* | 22.1* | 1.9* | 4.7* | 16.4* | 2.3 |
| Patient-provider language concordant in non-English (%) | 0.7 | 0.1 | 2.1* | — | 4.4* | — | — | 2.1* | 3.2* | 2.3 |
| Patient-provider language discordant (%) | 3.9 | 1.4 | 12.7* | — | 18.4* | — | — | 8.2* | 16.5* | 16.5 |
| Other patient characteristics | ||||||||||
| Age (0–107) | 53.0 (24.0) | 57.4 (22.4) | 42.5 (24.9)* | 53.4 (20.1)* | 42.7 (24.6)* | 32.0 (23.0)* | 45.3 (22.8)* | 57.2 (21.6) | 34.3 (23.7)* | 39.6 (22.5)* |
| Female (%) | 62.8 | 62.3 | 66.6* | 66.3 | 63.3 | 53.8* | 70.1* | 69.2* | 65.5 | 66.8 |
| No. visits in the last year (0–10; top-coded) | 3.9 (5.7) | 4.2 (6.0) | 3.6 (5.1)* | 4.3 (6.0) | 2.7 (3.9)* | 2.9 (3.9)* | 3.3 (4.8)* | 3.3 (4.8)* | 2.6 (3.6)* | 2.6 (3.7)* |
| Proportion of visits late for the appointment (0–1) (N = 153,203) | 0.23 (0.22) | 0.21 (0.21) | 0.27 (0.22)* | 0.28 (0.23)* | 0.28 (0.23)* | 0.33 (0.24)* | 0.23 (0.21)* | 0.18 (0.19)* | 0.27 (0.23)* | 0.28 (0.24)* |
| Proportion of visits arrived >15 min before the scheduled time (0–1) (N = 153,203) | 0.22 (0.21) | 0.22 (0.21) | 0.22 (0.21) | 0.25 (0.22)* | 0.19 (0.20)* | 0.16(0.18)* | 0.29 (0.24)* | 0.25 (0.23)* | 0.20 (0.22) | 0.23 (0.23) |
Statistically significant at *P < 0.001.
For each variable, % (for dichotomous variable) or mean (SD) (for continuous variable) is presented.
N = 198,379, unless otherwise indicated.
EHR indicates electronic health record; NHW, non-Hispanic whites; PCP, primary care provider.
Racial/Ethnic Differences in Arrival Time, Patient-reported Wait Time, and Satisfaction With Wait Time
Asian and Hispanic/Latino patients consistently rated wait time poorer than NHWs (very good: 55.4%) (Table 1). Asian Indians were least likely to respond “very good” (36.8%). Most Asian subgroups, except for Japanese and Koreans, Hispanic/Latino, and black patients reported longer waits in the waiting area (range, 8.8–10.3 min) than NHWs (8.1 min).
Most Asian (eg, 23.0% of Asian Indian), Hispanic/Latino (17.8%), and black (17.7%) patients were more likely to arrive late for the appointment than NHW patients (12.7%), with the exception of Japanese patients (9.7%) who were less likely to be late (Table 1; see Appendix Table 2, Supplemental Digital Content 1, http://links.lww.com/MLR/B81 for detailed numbers). Contrary to longer patient-reported wait time, EHR-based time (postscheduled time) in the waiting area for minority groups (8.2–9.5 min) were not different from NHW (9.3 min). See Table 1 for differences across racial/ethnic groups in other demographic and visit characteristics.
Racial/Ethnic Differences in Patient-reported Wait Time and Satisfaction With Wait Time: Multivariate Regression Analysis
After accounting for nesting within providers and controlling for EHR-based wait time and patient and visit characteristics, logistic regression models showed that Asians of all subgroups, but not Hispanic/Latino or black patients, were less likely than NHWs to be satisfied with wait time (or to rate wait time as “very good”) (Table 2). Asian Indians were the least likely be satisfied with wait time (OR = 0.46). Patients were more likely to be satisfied with wait time if: they arrived late for their appointment, waited less in the waiting area, made a visit in the early morning, saw own PCP, preferred English, or were older or female relative to their counterparts (Table 2).
TABLE 2.
Racial/Ethnic Difference in Wait Time and Satisfaction: Provider Random-Effects Model†
| Dependent Variables | Satisfaction: Very Good | Patient-reported (Postscheduled) Time at Waiting Area |
|---|---|---|
| Variables | Odds Ratio | Coefficient (min) |
| R/E (reference: NHW) | ||
| Hispanic/Latino | 0.96 | 0.86* |
| Black | 0.86 | 0.80 |
| Chinese | 0.50* | 1.09* |
| Asian Indian | 0.46* | 1.79* |
| Filipino | 0.58* | 1.92* |
| Japanese | 0.62* | 0.029 |
| Korean | 0.51* | 0.89 |
| Vietnamese | 0.56* | 2.15* |
| Visit characteristics | ||
| EHR-based scheduled, arrived, and wait time indicators | ||
| Arrived late for the appointment | 1.13* | −0.96* |
| Time (postscheduled) spent at waiting area | 0.98* | 0.20* |
| Led to examination room earlier than scheduled time | 1.07 | −0.023 |
| Long visit (scheduled for 30+ min) | 1.02 | −0.039 |
| Visit time of the day | ||
| (reference: 6 am-9:59 am) | ||
| 10 am–11:59 am | 0.90* | 0.75* |
| 12 pm–2:59 pm | 0.93 | 0.48* |
| 3 pm–9 pm | 0.87* | 1.34* |
| No. days between survey return and visit | 0.9988 | 0.0064* |
| Own PCP visit | 1.11* | −0.59* |
| No. years with the PCP | 1.01 | −0.034 |
| Preventive visit | 1.06 | −0.78* |
| Visit for chronic condition | 1.06 | −0.11 |
| Patient-provider R/E concordant (reference: R/E discordant) | 0.97 | −0.085 |
| Non-English language concordant (reference: concordant in English) | 0.85 | 0.97 |
| Language discordant (reference: concordant in English) | 0.76* | 1.07* |
| Other patient characteristics | ||
| Age (reference: 18–34) | ||
| 0–17 | 1.11 | −0.21 |
| 35–50 | 1.30* | −0.15 |
| 51–64 | 1.46* | −0.17 |
| 65 or older | 1.40* | 0.14 |
| Female | 1.06* | 0.13 |
| Insurance type (reference: PPO) | ||
| Health Maintenance Organization | 0.99 | 0.10 |
| Medicaid | 1.13 | 0.78 |
| Other insurance or self-pay | 1.16 | 0.45 |
| No. visits to the clinic in the last year (0–9, 10+) | 0.98* | 0.0081 |
| Proportion of visits late for the appointment | 0.97 | 0.49 |
| Proportion of visits arrived >15 min before scheduled time | 0.91 | 2.25* |
| Provider characteristics | ||
| Female | 0.90 | 0.068 |
| Physician (vs. nurse practitioner or physician assistant) | 0.94 | 0.999 |
| Years of medical practice | 0.997 | 0.024 |
| Constant | 5.01* | 0.24 |
| Rho | 0.057* | |
| Observations | 70,806 | 77,817 |
| No. providers | 833 | 856 |
P < 0.001.
Estimates from multivariate regression with provider random effects. Also included but not presented here variables are indicators for provider department, clinic, and division; (block level) % high school graduates, % college graduates, and median household income; and indicators of missing values in years of medical practice, insurance type, and appointment time.
EHR indicates electronic health record; NHW, non-Hispanic whites; PCP, primary care provider; R/E, race/ethnicity.
After controlling for EHR-based wait time indicators and other confounders, most Asian subgroups (except for Japanese and Koreans) and Hispanic/Latinos reported their wait time in the waiting area was longer compared with NHWs’; differences ranged from 0.86 minutes (Hispanic/Latino) to 2.15 minutes (Vietnamese) (Table 2). Factors influencing patient-reported wait time and wait time satisfaction were generally similar such that shorter EHR-based wait time, early morning visit, own PCP visit, and preferring English were predictors of shorter patient-reported wait time and higher satisfaction of wait time. Older patients or those who were female were more likely to be satisfied, but their reported wait time did not differ from younger or male patients, respectively. Patient were likely to report a shorter wait time for preventive visits and longer wait time when they arrived >15 minutes early.
To examine Asians’ reluctance to choose extreme choices as an explanation for their lower satisfaction rating, we examined an alternative specification for the satisfaction rating, combining “very good” and “good” categories (Table 3). The reduction in racial/ethnic difference with this new indicator was, however, negligible. We then assessed the possibility that Asians may be less satisfied with wait time because they overestimate their wait time. We found that patients who perceive their wait time longer had poorer wait time satisfaction, after controlling for actual wait time and other confounders, as expected, but adjusting for patient-reported wait time reduced little of the racial/ethnic differences in wait time satisfaction, except for Vietnamese patients.
TABLE 3.
Racial/Ethnic difference in Wait Time and Satisfaction: Provider Random-Effects Model†
| Dependent Variables | Satisfaction: Very Good or Good | Satisfaction: Very Good |
|---|---|---|
| Variables | Odds Ratio | Odds Ratio |
| R/E (reference: NHW) | ||
| Hispanic/Latino | 0.95 | 0.87 |
| Black | 0.94 | 0.83 |
| Chinese | 0.56* | 0.59* |
| Asian Indian | 0.48* | 0.59* |
| Filipino | 0.67* | 0.57* |
| Japanese | 0.59* | 0.64* |
| Korean | 0.45* | 0.55* |
| Vietnamese | 0.55* | 0.63 |
| Patient-reported (postscheduled) time at waiting area | 0.88* | |
| Patient-reported time at waiting area × R/E (reference: NHW) | ||
| Hispanic/Latino | 1.03* | |
| Black | 1.03 | |
| Chinese | 0.98 | |
| Asian Indian | 0.98 | |
| Filipino | 1.03 | |
| Japanese | 0.99 | |
| Korean | 1.00 | |
| Vietnamese | 1.01 | |
| Observations | 70,806 | 56,320 |
| No. providers | 833 | 824 |
P < 0.001.
Estimates from multivariate regression with provider random effects. Also included in the model but are not reported in the table are all the covariates in Table 2 including indicators of patient demographics, frequency of visits, tendency to arrive on time, EHR-based scheduled, arrived, and wait time measures, # days between survey return and visit, patient-provider relationship, and R/E and language concordance, visit type, provider characteristics, and department/clinic location).
NHW indicates non-Hispanic whites; R/E, race/ethnicity.
Sensitivity Analysis
We performed several analyses to examine whether observed racial/ethnic differences in wait time satisfaction and patient-reported wait time would be modified by other factors. We examined interaction between race/ethnicity and actual wait time on satisfaction of wait time, and found that the relationship between race/ethnicity and wait time satisfaction or patient-reported wait time did not change based on “length of wait time” (Appendix Table 3, Supplemental Digital Content 1, http://links.lww.com/MLR/B81). Further, we did not find an interaction between race/ethnicity and patient-reported wait time on satisfaction with wait time, except for Hispanic/Latino patients whose satisfaction was less affected by their reported wait time (Table 3).
We then examined the possibility that the observed racial/ethnic differences in wait time measures to be confounded by provider effects. That is, patients of certain racial/ethnic background may self-select certain providers, and unobserved provider practice characteristics may influence wait time satisfaction, even after adjusting for actual wait time and other patient, visit, and provider characteristics. This is, however, unlikely to be the reason for the racial/ethnic differences, as the results from provider fixed-effects model (which uses within-provider difference in the estimation; Appendix Table 4, Supplemental Digital Content 1, http://links.lww.com/MLR/B81) were almost identical to provider random-effects model (which uses both within and between-provider differences in the estimation) reported in Table 2.
Finally, to assess potential response bias and its impact on the overall results, we examined whether survey response is influenced by actual wait time and whether the relationship differs by race/ethnicity. We found no difference in actual wait time between respondents and nonrespondents in the overall sample as well as within each racial/ethnic group. Thus, lower response rates among minority groups would not have influenced our findings.
CONCLUSIONS
In our analysis of patient-reported wait time and wait time satisfaction versus EHR-based measures, we found that Asians rated their wait time experience poorer and tend to report longer wait time in the waiting area than NHWs. Actual (postscheduled) wait time in the waiting area, regardless of early or late arrival, varied little and did not differ across most racial/ethnic groups. Although longer actual wait time and longer patient-reported wait time were negative predictors of wait time satisfaction, neither explained lower satisfaction rating by Asians. In contrast, Hispanic/Latino and black patients did not rate wait time differently from NHWs, after controlling for confounders.
The heterogeneity in racial/ethnic satisfaction rating patterns (ie, lower ratings among Asians, but not among Hispanic/Latino and black patients) is generally consistent with previous studies on patient experience surveys. Asians tend to rate their health care experience lower than NHWs in the same settings,7,16–20 whereas black and Hispanic/Latino patients tend to give more favorable global ratings despite their lower ratings on more objective measures of care experience.21–24 Others have shown that relative to whites, Asians report lower ratings on “time to get an appointment with a general practitioner” in the UK, after adjusting for the actual time.7
We hypothesized that Asians report longer wait time because they reported arriving earlier than scheduled, and thus, have to wait longer to see their provider. This, however, was not the case. Most Asian subgroups—except for Japanese—were more likely to be late for the appointment, and most of the patients who were late were led to the examination room promptly, keeping their scheduled appointment rather than having their appointment canceled or moved to a later time. For example, average total waiting area time (including time before the scheduled time) was much longer for those who arrived early (eg, 16.5 min for those who arrived early by 4–10 min vs. 12.3 min for 1–5 min late arrivers) (Table 4). Similarly, most (79.2%) patients who arrived 6–15 minutes late were led to examination room within 15 minutes of arrival, but a half (55.7%) of patients who arrived 5–14 minutes early and only a third (31.9%) of patients who arrived 15–29 minutes early were led to examination room within 15 minutes of arrival (Table 4).
TABLE 4.
Relationship Between Arrival Time and Total Wait Time at Waiting Area
| Arrival Relative to Appointment | N (%) | Total Time at Waiting Area (min), Category (Row%) |
|||||
|---|---|---|---|---|---|---|---|
| Mean | SD | 0–4 min | 5–14 min | 15–29 min | 30–180 min | ||
| 30–120 min early | 5733 (5.6) | 36.6 | 23.0 | 0.9 | 15.3 | 27.7 | 56.1 |
| 15–29 min early | 18,268 (18.0) | 22.6 | 14.4 | 1.3 | 30.6 | 44.6 | 23.5 |
| 5–14 min early | 34,530 (33.9) | 16.5 | 12.1 | 3.0 | 52.7 | 34.0 | 10.3 |
| 0–4 min early | 19,506 (19.2) | 13.5 | 10.9 | 5.8 | 65.4 | 22.0 | 6.8 |
| 1–5 min late | 13,334 (13.1) | 12.3 | 10.6 | 7.9 | 68.6 | 17.8 | 5.7 |
| 6–15 min late | 8459 (8.3) | 11.7 | 10.6 | 11.8 | 67.4 | 15.6 | 5.2 |
| 16–120 min late | 1911 (1.9) | 13.1 | 13.3 | 17.6 | 55.3 | 17.8 | 9.3 |
| Overall | 101,741* | 17.2 | 14.2 | 4.8 | 52.4 | 29.3 | 13.5 |
Those with both preappointment and postappointment wait time measures.
Clinic arrival patterns vary substantially across racial/ethnic groups. Hispanic/Latino, Chinese, and Asian Indian patients generally arrived closer to or slightly late for scheduled appointments than NHWs. The tendency to be late was most prominent for Asian Indians. Contrarily, Japanese patients were more likely to arrive earlier than NHWs. Filipinos were likely to arrive either too early or late for the appointment.
Poorer satisfaction of wait time experience among most Asians may be due to several factors related to cultural norms and expectations. Asian immigrants may have different norms about arrival time relative to appointment time and different expectations about wait time. Japanese and Filipino are less likely to be recent immigrants25; thus, they may be more assimilated to US cultural norms. In our study population, Chinese and Asian Indians were the largest Asian subgroups. Most of these subpopulations ( > 60%) are recent immigrants and their cross-cultural differences in experience and expectation may be particularly strong.25 Although we do not have a measure of immigration status in the EHR, in our study population 77% of Asians (vs. 2% of NHWs) reported a language other than English as a primary language. Indeed, non-English as primary language (and seeing language-discordant provider) was significantly associated with lower odds of rating wait time experience as “very good” and an increased patient-reported wait time in the waiting area, controlling for actual wait time (Table 2).
In contrast, a majority of Hispanic/Latinos in our population are also a relatively new immigrant population, but they show patterns different from Asians in our study. While Hispanic/Latinos were more likely than NHW to arrive late for the appointment, as were most Asians, their rating of wait time and self-reported wait time did not differ from NHWs after controlling for actual wait time. One explanation would be the tendency of Asians not to give extreme positive or negative responses on surveys, as noted in the literature on general survey response patterns.26,27 In our study, however, combining “very good” and “good” satisfactory rating categories did not substantially reduce the “Asian effect.” Further, although wait-time was asked with an open-ended question and thus was not expected to be influenced by response pattern, it was longer for Asians.
Our overall findings suggest that the “expectation” and “perception” of wait time among Asians may be fundamentally different from NHWs, that is, the difference is not explained by differential treatment (ie, actual wait time), survey response pattern, or punctuality style. Expectations based on prior experience are a major psychological determinant of patient satisfaction.28,29 Most NHWs may expect to wait before scheduled time for a clinic visit, whereas many Asians may perceive it as unnecessary and avoidable, regardless of whether they were early or late for the scheduled time. We did not have direct measures of expectation based on prior experience with other health care settings. Alternatively, we inferred a patient’s tendency to be on time based on their previous visits to the organization we studied; however, it did not explain their satisfaction or reported wait time in the multivariate model (Table 2). Future studies should explore the role of expectations (using direct measures based on their previous experience from other countries) in the patient’s perceived wait time experience and how such expectation’s effects on satisfaction rating could be mitigated or effectively addressed with culturally tailored care delivery interventions.
Our study has several potential limitations. First, roughly one of 5 people responded to the survey, and respondents were not a random sample of all patients seen. We, however, detected no difference in actual wait time between respondents and nonrespondents, and further controlled for a comprehensive set of patient demographic, visit, and provider characteristics in multivariate analyses, and thus expect that racial/ethnic differences in response rate may not have influenced our main findings. Second, we did not have a reliable objective measure of wait time in the examination room. Time spent in the examination room waiting for the provider, which is not examined here, may have influenced satisfaction of wait time as well. We do not, however, expect that examination room wait time would differ by race/ethnicity, after other potential confounding factors taken into account here. Third, we did not have information on the acculturation of each individual, and thus could not directly test cultural difference with a direct measure. We instead used patient’s preferred language and patient-provider race/ethnicity and language concordance to assess potential differences in patient experience and rating of care based on cultural background and language barrier. Better measures of degree of acculturation would have helped tease out race/ethnicity, culture of the country of origin, and other influencing factors of arrival/wait time and expectation and satisfaction with wait time. Finally, patients included in the study were mostly privately insured (2% uninsured; <5% with Medicaid) and spoke English relatively well (< 1.5% indicated need for an interpreter). Patients with lower socioeconomic status may show different patterns of arrival and wait time from what we reported; they may be more likely to rely on public transportation and to arrive very early or late for an appointment. Similarly, special arrangements often need to be made for interpreter services, which may also influence a patient’s wait time. Wait time patterns in other clinical settings with more representation of patients with low socioeconomic status may be different. In our study, we focused on racial/ethnic differences within a setting where patients received similar care.
In conclusion, although the actual wait time among Asians was not longer than that of patients in other racial/ethnic groups in the same outpatient-care setting, they report longer wait times and greater dissatisfaction with wait time. Wait time in clinics is an objective measure, but is assessed subjectively, based on their expectation shaped by prior experiences, in patient experience surveys. Further studies are needed to assess these subjective disparities in wait time experience as we strive to provide excellent care to an increasingly diverse patient population in the United States.
Supplementary Material
Acknowledgments
Supported by AHRQ K01 HS019815 (PI: S.C.).
Footnotes
The abstract of this study has been presented at the AcademyHealth Annual Research Meeting, June 14–16, 2015, Minneapolis, MN, and the 21th Annual HMO Research Network Conference, April 10–13, 2015 at Long Beach, CA.
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Website, www.lww-medicalcare.com.
REFERENCES
- 1.IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2.Bleustein C, Rothschild DB, Valen A, et al. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care. 2014;20:393–400. [PubMed] [Google Scholar]
- 3.Boudreaux ED, O’Hea EL. Patient satisfaction in the emergency department: a review of the literature and implications for practice. J Emerg Med 2004;26:13–26. [DOI] [PubMed] [Google Scholar]
- 4.Thompson DA, Yarnold PR, Williams DR, et al. Effects of actual waiting time, perceived waiting time, information delivery, and expressive quality on patient satisfaction in the emergency department. Ann Emerg Med 1996;28:657–665. [DOI] [PubMed] [Google Scholar]
- 5.Leddy KM, Kaldenberg DO, Becker BW. Timeliness in ambulatory care treatment: an examination of patient satisfaction and wait times in medical practices and outpatient test and treatment facilities. J Ambul Care Manage. 2003;26:138–149. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed F, Burt J, Roland M. Measuring patient experience: concepts and methods. Patient. 2014;7:235–241. [DOI] [PubMed] [Google Scholar]
- 7.Mead N, Roland M. Understanding why some ethnic minority patients evaluate medical care more negatively than white patients: a cross sectional analysis of a routine patient survey in English general practices. BMJ 2009;339:b3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elliott MN, Zaslavsky AM, Goldstein E, et al. Effects of survey mode, patient mix, and nonresponse on CAHPSs Hospital Survey Scores. Health Serv Res 2009;44(2 pt 1):501–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elliott MN, Edwards C, Angeles J, et al. Patterns of unit and item nonresponse in the CAHPSs Hospital Survey. Health Serv Res 2005;40(6 pt 2):2096–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klein DJ, Elliott MN, Haviland AM, et al. Understanding nonresponse to the 2007 Medicare CAHPS Survey. Gerontologist 2011;51:843–855. [DOI] [PubMed] [Google Scholar]
- 11.Campbell JL, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients’ assessments of primary health care. Qual Health Care. 2001;10:90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sitzia J, Wood N. Response rate in patient satisfaction research: an analysis of 210 published studies. Int J Qual Health Care. 1998;10:311–317. [DOI] [PubMed] [Google Scholar]
- 13.Nieman CL, Benke JR, Ishman SL, et al. Whose experience is measured?: a pilot study of patient satisfaction demographics in pediatric otolaryngology. Laryngoscope 2014;124:290–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boscardin CK, Gonzales R. The impact of demographic characteristics on nonresponse in an ambulatory patient satisfaction survey. Jt Comm J Qual Patient Saf 2013;39:123–128. [DOI] [PubMed] [Google Scholar]
- 15.Van Walraven C, Oake N, Jennings A, et al. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract 2010;16:947–956. [DOI] [PubMed] [Google Scholar]
- 16.Campbell J, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients’ assessments of primary health care. Qual Health Care. 2001;10:90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract 2010;11:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lyratzopoulos G, Elliott M, Barbiere J, et al. Understanding ethnic and other socio-demographic differences in patient experience of primary care: evidence from the English General Practice Patient Survey. BMJ Qual Saf 2012;21:21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murray-Garcia JL, Selby JV, Schmittdiel J, et al. Racial and ethnic differences in a patient survey: patients’ values, ratings, and reports regarding physician primary care performance in a large health maintenance organization. Med Care. 2000;38:300–310. [DOI] [PubMed] [Google Scholar]
- 20.Ngo-Metzger Q, Legedza AT, Phillips RS. Asian Americans’ reports of their health care experiences. J Gen Intern Med 2004;19:111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morales LS, Elliott MN, Weech-Maldonado R, et al. Differences in CAHPS adult survey reports and ratings by race and ethnicity: an analysis of the National CAHPS benchmarking data 1.0. Health Serv Res 2001;36:595–617. [PMC free article] [PubMed] [Google Scholar]
- 22.Weech-Maldonado R, Elliott MN, Oluwole A, et al. Survey response style and differential use of CAHPS rating scales by Hispanics. Med Care. 2008;46:963–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weech-Maldonado R, Morales LS, Elliott M, et al. Race/ethnicity, language, and patients’ assessments of care in Medicaid managed care. Health Serv Res 2003;38:789–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinick RM, Elliott MN, Volandes AE, et al. Using standardized encounters to understand reported racial/ethnic disparities in patient experiences with care. Health Serv Res 2011;46:491–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Census Bureau. Table S0201. Selected population profile in the United States. 2008 American Community Survey 1-Year Estimates.
- 26.Chen C, Lee S-y, Stevenson HW. Response style and cross-cultural comparisons of rating scales among East Asian and North American students. Psychol Sci 1995;6:170–175. [Google Scholar]
- 27.Lee JW, Jones PS, Mineyama Y, et al. Cultural differences in responses to a Likert scale. Res Nurs Health. 2002;25:295–306. [DOI] [PubMed] [Google Scholar]
- 28.Linder-Pelz S Social psychological determinants of patient satisfaction: a test of five hypothesis. Soc Sci Med 1982;16:583–589. [DOI] [PubMed] [Google Scholar]
- 29.Williams B Patient satisfaction: a valid concept? Soc Sci Med 1994;38:509–516. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


