Abstract
Background
Musculoskeletal disorders are disabling diseases which affect work performance, thereby affecting the quality of life of individuals. Pharmacological and surgical management are the most recommended treatments. However, non-invasive physical therapies are said to be effective, for which the evidence is limited.
Aim/Purpose
To study the effect of non-invasive physical interventions in preventing surgery among patients recommended for surgery for musculoskeletal complaints, who attended sports and fitness medicine centres in India.
Settings
SPARRC (Sports Performance Assessment Research Rehabilitation Counselling) Institute) is a physical therapy centre with 13 branches spread all over India. This Institute practices a combination of manual therapies to treat musculoskeletal complaints.
Research Design
Descriptive cohort study involving the review of case records of the patients enrolled from June 2013 to July 2017, followed by the telephone survey of the patients who have completed treatment.
Intervention
Combination of physical therapies such as myofascial trigger release with icing, infra-red therapy, pulsed electromagnetic field therapy, stretch release, aqua therapy, taping, and acupuncture were employed to reduce the pain and regain functionalities.
Main Outcome Measures
Self-reported pains were measured using visual analogue scale at different levels of therapy—preand post-therapy and post-rehabilitation.
Results
In total, 909 patients were studied, of whom 152 (17%) patients completed the treatment protocol. Majority of patients presented with knee and low-back pain. The reduction in pain due to the treatment protocol in terms of mean VAS score from baseline to post-therapy and baseline to post-rehabilitation was statistically significant (p value = .00). Among those contacted post-rehabilitation, 82 patients remained without surgery, and the median surgery-free time was around two years.
Conclusion
Thus the study concluded that non-invasive physical therapies may prevent or postpone surgeries for musculoskeletal complaints.
Keywords: physical therapy, complementary therapy, manual therapy, musculoskeletal, rehabilitation, retrospective, SPARRC
INTRODUCTION
Musculoskeletal (MSK) disorders are considered as one of the most important factors affecting the quality of life. The disorders result in disability and, in turn, affect work performance, thereby decreasing the productivity of individuals. Hence they affect the individuals, communities, as well as the society, by increasing the economic burden.(1,2)
The management of these pains is often expensive in terms of treatment cost, as well as the unearned cost due to disability.(3) Various causes of the MSK disorders are repetitive strain on the system due to the activities of daily life, occupational hazards, traumatic injuries due to accidents, and diseases affecting musculoskeletal system. (4) The prevailing treatment modalities are pharmacological (oral and injectable), surgical, and non-invasive physical interventions.(5) Unlike pharmacological treatments, such as analgesics and injection therapies, surgery is the most prescribed intervention for most MSK complaints.
However, MSK surgeries have their own complications, such as degeneration of adjacent muscles and ligaments, which result in post-operative pains and restriction in mobility. Manchikanti et al.(6–9) explain this as post-surgery syndrome in their series of articles. In addition, systematic reviews explained that interventions used for management of MSK pains, in which steroidal injections and opioids were used to treat the post-surgical complications, were costly and produced short-term relief.(10,11) Moreover a recent article explains the recommendations, based on Danish, USA, and UK guidelines, for the management of low-back pain which may be applicable for all the MSK pains. In the study, it is strongly recommended to limit the usage of unnecessary imaging, rest, opioids, spinal injections, and surgery due to their limitations in results and long-term consequences. The suggestion is given to focus on functional activity, including work participation, instead of focusing on abnormality. The article further recommends considering exercise therapy as the first line of treatment option, along with other complementary therapies and education.(12)
Moreover, active complementary interventions, like massage therapy, trigger point release, acupuncture, aqua therapy, yoga, Tai Chi and other exercise prescriptions like aerobics, are found to reduce pain and help patients regain their functionalities thereby avoiding surgeries.(13–16)
This paper aimed at assessing the effect of combination of non-invasive physical interventions in preventing surgery among patients recommended for surgery for musculoskeletal complaints, and who attended sports and fitness medicine centres in India.
METHODS
Study Setting
SPARRC (Sports Performance Assessment Rehabilitation Research Counselling) Institute is a Fitness and Sports Medicine Institute with 13 centres spread across 5 states of India. The Institute provides a combination of physical and manual therapies, along with exercise therapy, to treat MSK complaints such as sports injuries, pains, degenerative diseases, and surgical complaints. Ergonomics, postural corrections, and fitness are also specializations of the Institute. One of its treatment protocols for preventing MSK surgeries comprises of non-invasive interventions whereby patients who are referred for surgeries from elsewhere are enrolled. These patients are self-referred, and attend the Institute seeking an alternate treatment option for surgery. Patients were enrolled under this protocol based on the referral for surgery from another hospital, the severity of pain measured by Visual Analogue Scale, and the severity of the complaints.
Non-invasive Treatment Protocol
This protocol consists of one counselling/education session and three phases: therapy/pain management, rehabilitation, and fitness.
In the counselling session, the patients are given clear information about the phases of the treatment protocol, modes of administration and action of therapies, and stretching and strengthening exercise during rehabilitation. The roles of the patients and the importance of adherence to all phases of the protocol are clearly explained to the patients in this session.
In the therapy phase, the specific muscle which is responsible for causing the ailments is treated with a combination of therapies such as myofascial trigger point release, acupuncture, aqua therapy, pulsed electromagnetic therapy, cryotherapy, inferential therapy, and stretch release. The choice of therapy is individualized by the sports medicine physicians based on the patient’s susceptibility, type, and severity of the complaints. The number of sessions varies between 3 and 15 based on the severity of the complaint. The duration of each session is 1 hour a day, and it is administered one-on-one by the trained physical and manual therapists.
The rehabilitation phase of the treatment is started when the self-reported pain intensity of the patient reduces to 60%–80%. In this phase, the patients are provided with specific exercise protocols to regain strength and total functioning of the affected muscles. Duration of this phase may be one to four months, depending upon the recovery of the patients. Once they are totally relieved from pain, the patients are moved to the next phase, fitness.
In the fitness phase, the patients are provided with a set of exercises to attain the recommended fitness level in order to prevent recurrence and to maintain the pain-free status. For the patients who are not able to come to the centres, these exercises are taught so they can continue to practice at home on their own.
Patients who completed up the rehabilitation phase were considered as having completed the treatment protocol; those who did not complete the rehabilitation phase were considered as dropouts.
Operational Definitions
Myofascial trigger point therapy
A manual therapy utilizing “trigger point release pressure”, neuromuscular techniques and stretching to relieve the chronically contracted segments of muscle and soft tissue causing painful knots (trigger points), muscle weakness, and restricting range of muscle motion. Myofascial Trigger Point Therapy is one of the treatment protocols for the treatment of myofascial pain and dysfunction.(17)
Cryotherapy
The application of cold temperature for the treatment of injuries and pain. Common method is icing, for which ice packs, ice towels, ice massage, gel packs, refrigerant gases, and inflatable splints are used. This method is also used to reduce the recovery time as part of the rehabilitation program after acute and chronic injuries.(18)
Acupuncture
Acupuncture is a Chinese practice of inserting fine needles through the skin at specific points especially to cure disease or relieve pain.(19)
Aqua therapy
A therapy program utilizing the properties of water, designed by a suitably qualified physiotherapist to improve function, carried out by appropriately trained personnel, ideally in a purpose-built, and suitably heated hydrotherapy pool.(20)
Pulsed electromagnetic field (PEMF) therapy
PEMF therapy is a non-invasive therapy where cellular level changes are stimulated by passing electromagnetic waves to the affected site in order to accelerate healing process, this compliments other therapies with regular exercise and a healthy diet.(21)
Stretch release
A rehabilitation technique which involves myofascial release that physical therapists or massage therapists use to stretch and release connective tissue, or fascia, tightness within and around the muscles that causes pain and stiffness.(22)
Taping
Taping is the technique employed to restrict the movement of injured joints and soft tissue compression to reduce swelling. It is commonly used as an adjunct therapy for the protection of an injured anatomical structure during the healing process. Rigid strapping tape, referred to as sports tape or athletic tape, is the commonly used; elastic strapping tape is also used where less rigidity is needed.(23)
Study Design
This was a descriptive cohort study involving record review with a before/after analytic component, followed by a telephone survey of patients who completed the treatment protocol up to the rehabilitation phase.
Data collection
Data for each patient are routinely collected in paper-based case record forms which are maintained at each centre. A specific data extraction sheet was designed and circulated to the centres. A physiotherapist was assigned for data extraction at each centre. Retrospective profiling of patients referred for surgery from elsewhere and attending one of the 13 SPARRC Institutes for further management and who enrolled between 2013 and 2017 was conducted.
There were 909 patients registered (having met the criteria) and their case records were reviewed. The demographic details (age, gender, and occupation) and clinical characteristics (site of the pain, onset mechanism and predisposing factors to the pain, treatment procedures, pain score before and after treatment, details of the recommended surgery, and the status of intervention completion) were extracted. Data from each centre were collated, processed, and analyzed by the principle investigator.
Telephone Follow-up
Among the patients who completed the treatment protocol [152 (17%)], 132 (87%) patients’ contacts were available and they were followed up by telephone in October 2018. During follow-up calls, a few questions were asked to assess the present status of the patient: Pain status in VAS?; How are you managing your pain?; Have you undergone surgery or not?; Are you practicing the exercises prescribed regularly or not? Telephone follow-up is the routine practice of the Institution. It was structured by the researcher using these four specific questions, and the calls were recorded. The answers to the specific questions were documented by the researcher from the recordings. There was no translation needed as the researchers were proficient in English as well as the local language.
Data Analysis
Demographic, clinical characteristics, and given treatment options of the patients were summarized as frequencies and percentages. Since there were combinations of therapies used, the frequency of the given therapies was obtained using multiple response set and presented. Severity of pain was taken as an outcome variable and measured with visual analogue scale (VAS: 0 for no pain and 10 for highest severity of pain). VAS score was measured at different phases of treatment: at the entry, at the end of therapy phase, and at the end of rehabilitation phase. Baseline VAS score was available for 760 (84%) patients. Only 324 (36%) patients had both baseline and post-therapy VAS scores recorded, and only 152 (17%) patients had the post-rehabilitation VAS score. These 152 (17%) patients based on the availability VAS score at entry, post-therapy and post-rehabilitation were taken as eligible for further analysis, as well as for the telephone follow-up. Repeated measures ANOVA (Analysis of Variance) was used to find out the significance of the treatment protocol in reducing the pain. Time to event (Kaplan Meyer Survival) analysis was done to find out the median surgery-free duration due to treatment for the patients who participated in the telephone calls [86 (65%)].
RESULTS
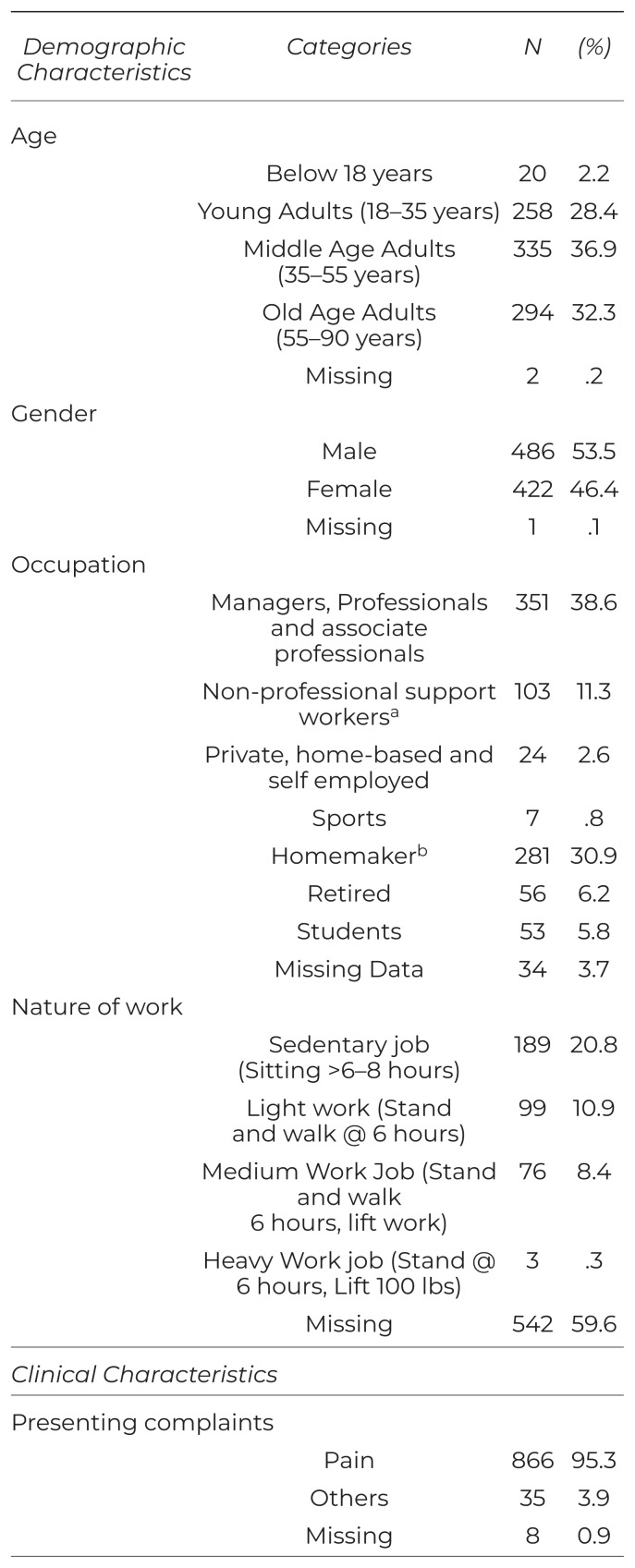
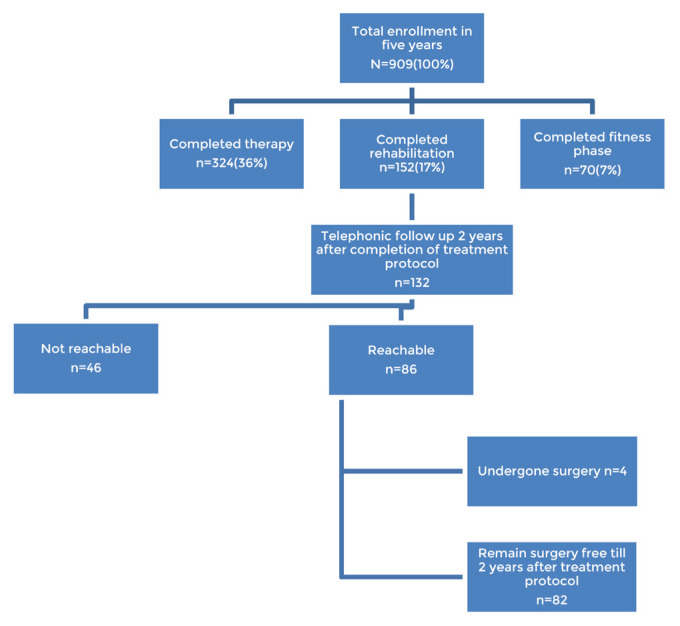
The socio-demographic and clinical characteristics of the patients are given in Table 1. The schematic representation of number of patients at different levels of treatment protocol is given in Figure 1. In total, there were 152 (17%) patients who completed the treatment protocol. Knee pain was the highest prevailing complaint, followed by low-back pain. Majority of the patients reported chronic pain which had gradual onset. The therapies offered were myofascial trigger release (MFTR) with icing (713, 78%), acupuncture (185, 20%), aqua therapy (142, 16%), interferential therapy (124, 14%), pulsed electromagnetic field (PEMF) therapy (55, 6%), taping (35, 4%), and stretch release (33, 4%). The details of the combinations of therapy are given in Table 2.
Table 1.
Demographic and Clinical Characteristics of Patients with Musculoskeletal Complaints Attending Physical Therapy Centres of a Sports Medicine Institute in India
| Demographic Characteristics | Categories | N | (%) |
|---|---|---|---|
| Age | |||
| Below 18 years | 20 | 2.2 | |
| Young Adults (18–35 years) | 258 | 28.4 | |
| Middle Age Adults (35–55 years) | 335 | 36.9 | |
| Old Age Adults (55–90 years) | 294 | 32.3 | |
| Missing | 2 | .2 | |
| Gender | |||
| Male | 486 | 53.5 | |
| Female | 422 | 46.4 | |
| Missing | 1 | .1 | |
| Occupation | |||
| Managers, Professionals and associate professionals | 351 | 38.6 | |
| Non-professional support workersa | 103 | 11.3 | |
| Private, home-based and self employed | 24 | 2.6 | |
| Sports | 7 | .8 | |
| Homemakerb | 281 | 30.9 | |
| Retired | 56 | 6.2 | |
| Students | 53 | 5.8 | |
| Missing Data | 34 | 3.7 | |
| Nature of work | |||
| Sedentary job (Sitting >6–8 hours) | 189 | 20.8 | |
| Light work (Stand and walk @ 6 hours) | 99 | 10.9 | |
| Medium Work Job (Stand and walk 6 hours, lift work) | 76 | 8.4 | |
| Heavy Work job (Stand @ 6 hours, Lift 100 lbs) | 3 | .3 | |
| Missing | 542 | 59.6 | |
|
| |||
| Clinical Characteristics | |||
|
| |||
| Presenting complaints | |||
| Pain | 866 | 95.3 | |
| Others | 35 | 3.9 | |
| Missing | 8 | 0.9 | |
| Number of the complaints | |||
| Single complaint | 663 | 72.9 | |
| Multiple complaints | 238 | 26.2 | |
| Missing | 8 | 0.9 | |
| Anatomical site of the painc | |||
| Low-back pain | 310 | 34.1 | |
| Hip pain | 30 | 3.3 | |
| Thigh pain | 23 | 2.5 | |
| Knee pain | 479 | 52.7 | |
| Leg pain | 41 | 4.5 | |
| Ankle pain | 22 | 2.4 | |
| Heel pain | 18 | 2.0 | |
| Foot pain | 15 | 1.7 | |
| Neck pain | 83 | 9.1 | |
| Arm pain | 10 | 1.1 | |
| Shoulder pain | 110 | 12.1 | |
| Elbow pain | 6 | 0.7 | |
| Forearm pain | 1 | 0.1 | |
| Wrist pain | 17 | 1.9 | |
| Hand pain | 10 | 1.1 | |
| Radiation of pain and other complaints | |||
| Yes | 436 | 48 | |
| No | 435 | 47.9 | |
| Missing | 38 | 4.2 | |
| Direction/extent of radiation | |||
| Unilateral | 140 | 15.4 | |
| Bilateral | 64 | 7 | |
| Missing/Side not mentioned | 232 | 25.5 | |
| Mechanism of onset | |||
| Sudden | 268 | 29.5 | |
| Gradual | 583 | 64.1 | |
| Missing | 58 | 6.4 | |
| Duration of complaints | |||
| Acute | 140 | 15.4 | |
| Sub-acute | 206 | 22.7 | |
| Chronic | 538 | 59.2 | |
| Missing | 25 | 2.8 | |
| Presence of precipitating conditions leading to presenting complaints | |||
| Yes | 383 | 42.1 | |
| No | 526 | 57.9 | |
| Precipitating conditions leading to presenting complaints | |||
| Injury/Fall | 115 | 12.7 | |
| Medical or surgical conditions | 53 | 5.8 | |
| Sports/exercise injury | 93 | 10.2 | |
| Occupation-related | 49 | 5.4 | |
| Heavy weight lifted | 8 | .9 | |
| Road traffic injury | 49 | 5.4 | |
| Others | 16 | 1.8 | |
| Presence of functional disabilities | |||
| Yes | 747 | 82.2 | |
| No | 162 | 17.8 | |
| Functional disabilitiesc | |||
| Bending forward | 110 | 12.1 | |
| Sitting | 80 | 8.8 | |
| Standing | 137 | 15.1 | |
| Squatting | 230 | 25.3 | |
| Walking | 113 | 12.4 | |
| Climbing stairs | 338 | 37.2 | |
| Trunk twisting | 222 | 24.4 | |
| Overhead activities | 9 | 1.0 | |
| Others | 42 | 4.6 | |
| Missing | 96 | 10.6 | |
Non-professional support workers refers to workers from clerical, services and sales, agriculture and forestry related, craft-related trade, plant and machine operators and assemblers, media and entertainment field, armed forces, and elementary occupation categories.
A person who is responsible for domestic chores, including childcare, as their primary occupation. In this context, this refers to females.
Since multiple set analysis were employed to find out the frequencies of the anatomical sites of the pain, the total may not add up to 909 and the percentages may not add up to 100.
Figure 1.
The schematic representation of number of patients at different levels of treatment protocol in a sports medicine institute in India between June 2013 and July 2017 (N=909).
Table 2.
Combinations of Therapies Given Under Non-invasive Treatment Protocol for the Patients with Musculoskeletal Complaints in this Study
| Combinations of Therapies Provided | n | (%) |
|---|---|---|
| MFTR + icing | 41 | 4.5 |
| Acupuncture alone | 5 | 0.6 |
| Aqua therapy alone | 7 | 0.8 |
| Direct rehabilitation | 70 | 7.7 |
| PEMF alone | 2 | 0.2 |
| MFTR+ icing +one other therapya | 190 | 20.9 |
| MFTR+ Icing +2 more therapiesa | 102 | 11.2 |
| MFTR+ Icing +3 more therapiesa | 150 | 16.5 |
| MFTR+ Icing +4 more therapiesa | 32 | 3.5 |
| MFTR+ Icing +5 more therapiesa | 143 | 15.7 |
| Acupuncture+1 more therapya | 4 | 0.4 |
| Acupuncture+2 more therapya | 16 | 1.8 |
| Aqua therapy+ one more therapya | 7 | 0.8 |
| Aqua therapy+2 more therapya | 2 | 0.2 |
| Othersb | 52 | 5.7 |
| Missing | 86 | 9.5 |
Along with MFTR, the other therapies combined may include acupuncture, aqua therapy, interferential therapy, PEMF, stretch release and tapping.
Category includes ischemic compression, JiJO points, ultrasound therapy, reflexology, Vitamin D3 supplements, and muscle relaxants prescription.
MFTR = myofascial trigger point release therapy; PEMF = pulsed electromagnetic field therapy.
The mean (standard deviation) VAS score at baseline, post-therapy and post-rehabilitation were 6.51 (2.18), 3.03 (1.51), and 1.67 (1.53), respectively. Repeated measures ANOVA was done to analyze the change in pain score (complete case analysis was done), with a Greenhouse-Geisser correction that determined that mean pain score measured in Visual Analogue Scale (VAS) differed statistically significantly between time points (F = 17.123, p < .0005). Post hoc tests using Bonferroni correction revealed that the non-invasive treatment protocol physical intervention reduced pain and the difference is statistically significant. The reduction in mean VAS score from baseline to post-therapy and baseline to post-rehabilitation was statistically significant (Table 3).
Table 3.
Results of the Repeated Measures ANOVA Test for Pre- and Post-Therapy and Post-Rehabilitation Visual Analogue Scale (VAS) Scoresa of the Patients with Various Musculoskeletal Complaints Who Completed the Treatment Protocol (N=152)
| Variables | Mean Difference | P Value b | 95% Confidence Interval | ||
|---|---|---|---|---|---|
|
| |||||
| Lower limit | Upper limit | ||||
| Pre-VAS score at entry | Post-therapy VAS score | 4.075 | .000 | 3.694 | 4.456 |
| Post-rehabilitation VAS score | 5.445 | .000 | 5.021 | 5.869 | |
| Post-therapy VAS Score | Pre-VAS score at entry | −4.075 | .000 | −4.456 | −3.694 |
| Post-rehabilitation VAS score | 1.370 | .000 | 1.048 | 1.692 | |
| Post-rehabilitation VAS Score | Pre-VAS score at entry | −5.445 | .000 | −5.869 | −5.021 |
| Post-therapy VAS score | −1.370 | .000 | −1.692 | −1.048 | |
The mean (SD) VAS score at baseline, post-therapy and post-rehabilitation were 6.51 (2.18), 3.03 (1.51) and 1.67 (1.53), respectively.
Statistically significant.
Patients’ Health Status on Telephone Follow-Up
Of the total, 152 (17%) patients completed the full intervention protocol up to rehabilitation phase and were considered as qualified for telephone follow-up. Among the patients who completed the treatment protocol [152 (17%)], 132 (87%) patients’ contacts were available and they were followed up by telephone call in October 2018. Among the contacted patients, 86 (65%) attended the call and the remaining numbers were not reachable.
Among contacted patients (n = 86), 82 patients still have not undergone surgery and remain pain free. Of these, five patients reported that they were taking alternate medicine and two were taking allopathic medicine. The rehabilitation exercises taught in the Institute were followed up regularly by 37 patients, whereas 17 patients did not do them regularly. Survival analysis by Kaplan Meyer estimate method was used to find the median (IQR) surgery-free time period and was estimated to be 776 (676,995) days at 95% confidence interval.
DISCUSSION
The study has attempted reviewing the case record forms of patients with MSK complaints who were referred to undergo surgeries and who came to the sports and fitness medicine centres seeking non-invasive interventions as an alternate treatment option for surgeries. From reviewing the case record forms, it was evident that a combination of noninvasive complementary therapies had reduced the MSK pains and also prevented surgeries effectively.
Musculoskeletal Pain and its Associations
The highest prevailing complaint among the study participants was knee pain, whereas low-back pain is mentioned as the top most cause of disability in Institute of Health Metrics and Evaluation ranking. (4) The pains mostly were chronic in nature with gradual onset. The prevalence of MSK pain was found to be higher among working generation between the age group of 30–50 years in a study conducted in Japan. (24) Similarly in the present study, around 75% of the patients were over 35 years of age.
There are established evidences for the relationship between nature of job and musculoskeletal pains due to over exertion of upper limb and neck muscles. Current study findings also had high prevalence of MSK pains among professional, associate professional, and non-professional support workers which may be correlated with their nature of jobs, especially sitting jobs; however, this can be proven significantly in future studies. Housewives were also the more affected group in this study. This may be explained due to repeated strain on MSK system based on a review which listed the possible reasons for high prevalence such as the high amount of unpaid work, lifting of heavy objects and children, work requiring use of upper limbs like washing clothes and utensils, sweeping, and cooking. The same study stated psychosomatic stress also a risk factor for MSK pain.(25) However, these associations should be studied in detail with more prospective studies. Injuries due to fall at various places like house, during sports and exercises were the other reasons which were specifically related with the existing pains.
Non-invasive Complementary Interventions Can Prevent Surgery
Non-invasive complementary therapies are always considered as an effective alternate for surgeries. In a survey conducted in London, 81% of the patients didn’t preferred surgery for treating their MSK pain due to various reasons such as fear of risk involved, old age, post-operative pain, or they perceived it as an unnecessary option.(26) In the present context, the study population considered that surgery is not the appropriate treatment for MSK pains and unnecessary MSK surgeries can be prevented with other alternative methods of treatments.
There are existing evidences also suggesting that surgery is not superior to the other conservative treatments.(27) Present treatment guidelines discourage the use of surgical and other invasive therapies due to their long-term adverse effects. The guidelines also recommend the use of complementary therapies and exercise based interventions, along with education, for the management of MSK complaints.(12) Often multidisciplinary approaches involving complementary therapies, including exercise therapies, are employed in treating MSK pains.(28) The present study setting followed the multidisciplinary approach and used combinations of noninvasive therapies to treat the MSK complaints. By this approach, the reduction in MSK pain was promising, and the data support this with statistical significance in this study. Best practices from complementary therapies, such as acupuncture, aqua therapy, inferential therapy, and pulsed electromagnetic therapies, were combined with myofascial trigger point release therapy and exercise on patients for the effective relief from MSK complaints. Exercise-based interventions in the rehabilitation phase contributed in the strengthening of muscles in order to bring the patients to pain-free status and to maintain the healing. A Norwegian clinical trial postponed hip replacement surgery up to six years through a 12-week exercise therapy program, along with education.(29) Similarly, the present study has the evidence for postponing surgery effectively using non-invasive physical interventions for up to two years. However, this can be further studied by future prospective studies.
Adherence to Non-invasive Complementary Interventions
Adherence to the treatment protocol is the key to the effectiveness of the therapy. Not only completing the therapy, completing the exercise-based rehabilitation also has the significance in cure. However, adherence to the therapy in complementary system is found to be a challenge globally. There are various reasons for this which includes time constraints, lack of belief in the system, cost involved, travel to the facility, lack of privacy in the therapy, and intervening other medical therapies. (30) The present study also showed the low completion rates; only 36% (324) and 17% (152) had completed the treatment protocol up to therapy and rehabilitation phases, respectively. The above-mentioned factors could be given as reasons. Apart from this, in the treatment protocol, the patients from the therapy phase are transferred to the rehabilitation phase only if the pain was reduced by 60%–80%. Hence the pain reduction itself might be the reason for not continuing to the rehabilitation phase, in which case the patients feel that they are cured and it is not necessary to move into next phase. Moreover the exercise-based rehabilitation is more active process for the patient compared to the therapy, where the patient remains passive. Spending a regular time on rehabilitation might be challenging for the working population, as well as for others. Since majority of our study population comes under working category, this might explain the low completion rates observed. However, these facts may need to be studied with further prospective studies where the patients can be accessed even after discontinuing from the therapy/rehabilitation. Also, factors such as belief in the system, time factor, and socio-economic impact on adherence can be studied with future research.
CONCLUSION
The present study clearly reveals that surgery may not be the optional first line treatment for treating all MSK complaints. Multidisciplinary approach involving combination of non-invasive complementary interventions had effectively reduced of the MSK pains and prevented surgery in 95% of the patients who completed treatment. Thus this approach can be an effective alternate for surgical and pharmacological therapies for managing the majority of MSK complaints.
Footnotes
CONFLICT OF INTEREST NOTIFICATION
The authors declare there are no conflicts of interest.
REFERENCES
- 1.Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Health Metrics and Evaluation (IHME) Rethinking Development and Health - Findings from the the Global Burden of Disease Study. Seattle, WA: IHME; 2016. [Accessed September 8, 2017]. http://www.healthdata.org/sites/default/files/files/images/news_release/2016/IHME_GBD2015.pdf . [Google Scholar]
- 3.Tsertsvadze A, Clar C, Court R, Clarke A, Mistry H, Sutcliffe P. Cost-effectiveness of manual therapy for the management of musculoskeletal conditions: a systematic review and narrative synthesis of evidence from randomized controlled trials. [Accessed September 8, 2017];J Manipulative Physiol Ther. 2014 37(6):343–362. doi: 10.1016/j.jmpt.2014.05.001. http://linkinghub.elsevier.com/retrieve/pii/S0161475414000876 . [DOI] [PubMed] [Google Scholar]
- 4.International Association for the Study of Pain. Musculoskeletal Pain. Washington, DC: IASP; 2009. [Accessed September 8, 2017]. http://www.aped-dor.org/images/FactSheets/Dor-MusculoEsqueletica/en/MusculoskeletalPain.pdf . [Google Scholar]
- 5.Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Noninvasive Treatments for Low Back Pain. Report #16-ECH004-EF. Rockville, MD: Agency for Healthcare Research and Quality (US); 2016. [Accessed January 31, 2018]. http://www.ncbi.nlm.nih.gov/pubmed/26985522 . [PubMed] [Google Scholar]
- 6.Manchikanti L, Cash KA, McManus CD, Pampati V, Smith HS. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 1—Discogenic pain without disc herniation or radiculitis. [Accessed December 11, 2018];Pain Physician. 2008 11(6):785–800. http://www.ncbi.nlm.nih.gov/pubmed/19057626 . [PubMed] [Google Scholar]
- 7.Manchikanti L, Cash KA, McManus CD, Pampati V, Abdi S. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 4—Spinal stenosis. [Accessed December 11, 2018];Pain Physician. 2008 11(6):833–848. http://www.ncbi.nlm.nih.gov/pubmed/19057629 . [PubMed] [Google Scholar]
- 8.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 2—Disc herniation and radiculitis. [Accessed December 11, 2018];Pain Physician. 2008 11(6):801–815. http://www.ncbi.nlm.nih.gov/pubmed/19057627 . [PubMed] [Google Scholar]
- 9.Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 3—Post surgery syndrome. [Accessed December 11, 2018];Pain Physician. 2008 11(6):817–831. http://www.ncbi.nlm.nih.gov/pubmed/19057628 . [PubMed] [Google Scholar]
- 10.Manchikanti L, Boswell MV, Datta S, Fellows B, Abdi S, Singh V, et al. Comprehensive review of therapeutic interventions in managing chronic spinal pain. [Accessed December 11, 2018];Pain Physician. 2009 12(4):E123–E198. http://www.ncbi.nlm.nih.gov/pubmed/19668281 . [PubMed] [Google Scholar]
- 11.Axon DR, Patel MJ, Martin JR, Slack MK. Use of multidomain management strategies by community dwelling adults with chronic pain: evidence from a systematic review. Scand J Pain. 2019;19(1):9–23. doi: 10.1515/sjpain-2018-0306. [DOI] [PubMed] [Google Scholar]
- 12.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 13.Iversen MD. Managing hip and knee osteoarthritis with exercise: what is the best prescription? [Accessed September 8, 2017];Ther Adv Musculoskelet Dis. 2010 2(5):279–290. doi: 10.1177/1759720X10378374. http://www.ncbi.nlm.nih.gov/pubmed/22870454 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yan J-H, Gu W-J, Sun J, Zhang W-X, Li B-W, Pan L. Efficacy of Tai Chi on pain, stiffness and function in patients with osteoarthritis: a meta-analysis. [Accessed September 8, 2017];PLoS One. 2013 8(4):e61672. doi: 10.1371/journal.pone.0061672. http://www.ncbi.nlm.nih.gov/pubmed/23620778 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Øiestad BE, Østerås N, Frobell R, Grotle M, Brøgger H, Risberg MA. Efficacy of strength and aerobic exercise on patient-reported outcomes and structural changes in patients with knee osteoarthritis: study protocol for a randomized controlled trial. BMC Musculoskelet Disord. 2013;14(1):266. doi: 10.1186/1471-2474-14-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang DG, Holt JA, Sklar M, Groessl EJ. Yoga as a treatment for chronic low back pain: a systematic review of the literature. [Accessed September 8, 2017];J Orthop Rheumatol. 2016 3(1):1–8. http://www.ncbi.nlm.nih.gov/pubmed/27231715 . [PMC free article] [PubMed] [Google Scholar]
- 17.Janssens LA. Trigger point therapy. Probl Vet Med. 1992;4(1):117–124. [PubMed] [Google Scholar]
- 18.Swenson C, Swärd L, Karlsson J. Cryotherapy in sports medicine. [Accessed December 18, 2018];Scand J Med Sci Sports. 1996 6(4):193–200. doi: 10.1111/j.1600-0838.1996.tb00090.x. http://www.ncbi.nlm.nih.gov/pubmed/8896090 . [DOI] [PubMed] [Google Scholar]
- 19.Acupuncture [definition] Merriam Webster Online. Retrieved May 9, 2020, from https://www.merriam-webster.com/dictionary/acupuncture.
- 20.ATACP. About the Aquatic Therapy Association of Chartered Physiotherapists (ATACP) [Accessed December 4, 2018]. https://atacp.csp.org.uk/content/about-atacp. Published 2014.
- 21.What types of conditions can PEMF therapy treat? [Accessed May 9, 2020]. https://www.news-medical.net/whitepaper/20180320/What-types-of-conditions-can-PEMF-therapy-treat.aspx .
- 22.Hip Stretches and Myofascial Release | Livestrong.com. [Accessed May 10, 2020]. https://www.livestrong.com/article/428668-hip-stretches-and-myofascial-release/
- 23.Physiopedia. Taping. [Accessed November 28, 2019]. https://www.physio-pedia.com/Taping .
- 24.Nakamura M, Nishiwaki Y, Ushida T, Toyama Y.Prevalence and characteristics of chronic musculoskeletal pain in Japan J Orthop Sci 2011164: 424–432. 10.1007/s00776-011-0102-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Habib RR, Fathallah FA, Messing K. Full-time homemakers: workers who cannot “go home and relax”. Int J Occup Saf Ergon. 2010;16(1):113–128. doi: 10.1080/10803548.2010.11076833. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell HL, Hurley MV. Management of chronic knee pain: a survey of patient preferences and treatment received. BMC Musculoskelet Disord. 2008;9(1):123. doi: 10.1186/1471-2474-9-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. [Accessed September 8, 2017];PLoS One. 2017 12(6):e0178621. doi: 10.1371/journal.pone.0178621. http://www.ncbi.nlm.nih.gov/pubmed/28640822 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharan D, Rajkumar JS, Mohandoss M, Ranganathan R. Myofascial low back pain treatment. Curr Pain Headache Rep. 2014;18(9):449. doi: 10.1007/s11916-014-0449-9. [DOI] [PubMed] [Google Scholar]
- 29.Svege I, Nordsletten L, Fernandes L, Risberg MA. Exercise therapy may postpone total hip replacement surgery in patients with hip osteoarthritis: a long-term follow-up of a randomised trial. Ann Rheum Dis. 2015;74(1):164–169. doi: 10.1136/annrheumdis-2013-203628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silva MA, Zablocki CJ. Predictors of Retention in Physical Therapy: Client-, Disease-, and Treatment-related Factors [online article] n.d. [Accessed June 13, 2018]. https://pdfs.semanticscholar.org/ba1e/e4a08be0fdfb45c6836f13ff3abd876ef2ea.pdf .