Abstract
Angiosarcoma is a malignant neoplasm of mesenchymal origin arising from vascular endothelium and most commonly involves extremities. Gingival angiosarcoma is a rare sporadic occurring tumor. We report a case of primary angiosarcoma of gingiva along with a review of 31 cases of primary gingival angiosarcoma reported in literature till 2018. A 30-year-old lady presented with recurrent gingival swelling over central mandible. She had no palpable cervical lymphadenopathy. She underwent central marginal mandibulectomy. Final histological analysis with immunohistochemistry was suggestive of the angiosarcoma of the gingiva. She is 50 months postoperative and doing well.
Introduction
Angiosarcoma is a malignant mesenchymal tumor originating from vascular endothelium, most commonly arising in extremities with long-standing lymphoedema. Oral and salivary gland angiosarcomas are rare, constituting only 1% of all angiosarcoma cases and mostly reported as case reports which occur commonly in tongue and lips [1]. Gingival angiosarcomas are still rarer. We present a case of angiosarcoma of gingiva along with a review of 31 reported cases in the literature.
Case Report
Thirty-year-old woman with no comorbidities presented with recurrent lower jaw gingival swelling. She underwent excision of the swelling four times elsewhere in the past 1 year. Family history was not significant. On examination, there was 1.5 cm × 1 cm fleshy swelling located centrally over gingiva of the lower jaw near incisor teeth (Fig. 1). There was no cervical lymphadenopathy. Histopathology of excision was done elsewhere, and slides reviewed at our hospital revealed features of angiosarcoma. Contrast-enhanced CT scan of neck and chest revealed a small (11 × 5 mm) heterogeneously enhancing lesion along gingival mucosa of a lower alveolus in the midline with no erosion of underlying bone; lungs were normal.
Fig. 1.
Clinical photograph showing epilus like swelling arising from gingiva of mandible
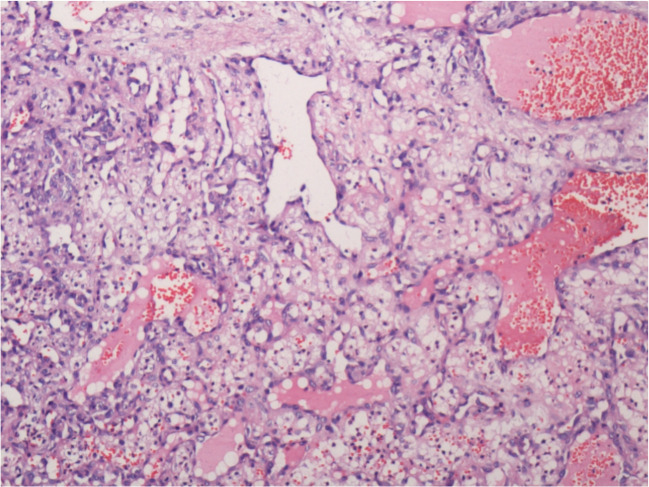
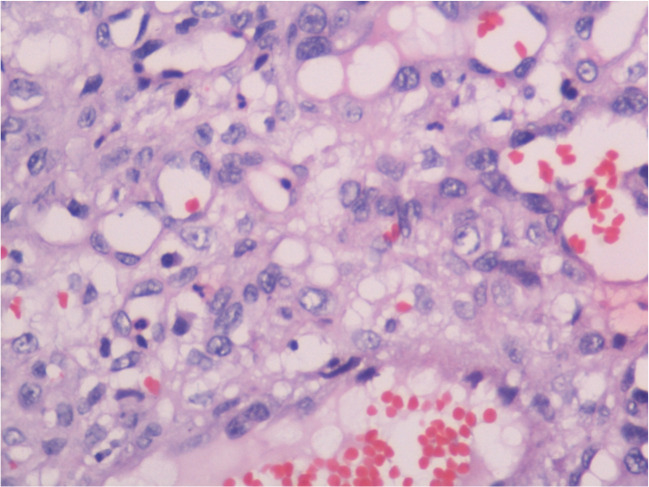
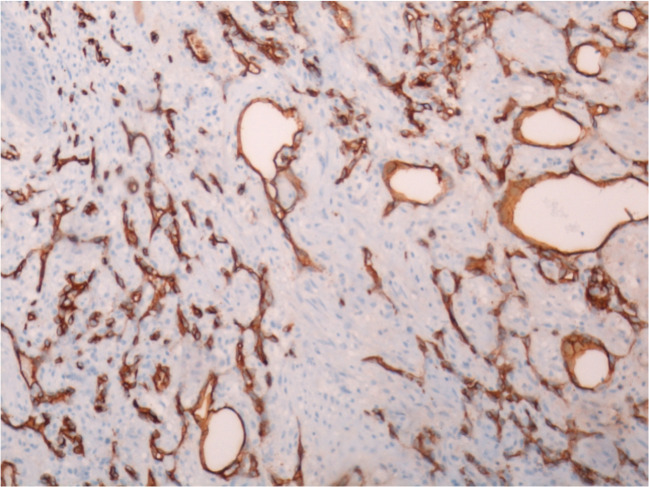
She underwent central marginal mandibulectomy with a 2-cm margin all around. Mobilization and approximation of floor of mouth mucosa with the lip mucosa to cover the exposed bone were done to close the defect. Rehabilitation was done by a removable partial denture. The final histopathological examination revealed polypoidal lesion lined by squamous epithelium; sub-epithelium tissue showed many thin congested vascular channels. The branching vascular channels were lined by round endothelial cells with atypia (Fig. 2). Stroma showed an inflammatory infiltrate of neutrophils, lymphocytes, and few atypical cells with scanty cytoplasm and hyperchromatic nuclei with 4–6 mitotic figures/10 HPF. Margins and bone were free of tumor. At high resolution (400×), pleomorphic tumor cells were seen (Fig. 3). Immunohistochemistry revealed strong positivity for CD 34(Fig. 4). Overall features were suggestive of well-differentiated angiosarcoma. The postoperative course was uneventful. Presently she is postoperative 50 months and doing well without any recurrence.
Fig. 2.
Photomicrograph showing branching vessels lined by atypical cells (100×)
Fig. 3.
Photomicrograph showing pleomorphic tumor cells (400×)
Fig. 4.
Immunohistochemistry showing strong positivity for CD 34 highlighting vessels
Review of Literature (Table 1)
Table 1.
Depicting patients demographics and details of treatment and follow up
| Author, year | Age (years)/sex | Location | Treatment of primary tumor | Follow up | |
|---|---|---|---|---|---|
| 1 | Henny 1949 [4] | 3 months/M | Anterior part of maxilla | Electrocoagulation | Disease free till 2 years and 3 months |
| 2 | Blake and Blake 1956 [5] | 26 M | First molar area of left mandible | Surgical excision | Disease free till 2 years and 4 months |
| 3 | Quinn et al. 1970 [6] | 65 M | Maxillary and mandibular gingiva | Surgical excision, radiotherapy | Died after 1 month and 3 weeks (cause unknown) |
| 4 | Albright et al. 1970 [7] | 34 M | Anterior part right mandible | Surgical excision | Disease free till 6 months |
| 5 | Wesley et al. 1975 [8] | 18 F | Gingiva of left mandible | Enbloc resection of left mandible | Disease free till 2 years of surgery |
| 6 | Piscioli et al. 1986 [9] | 86 F | Gingiva of the left mandibular molar area | Surgical excision | Died after 1 month due to cardiac failure |
| 7 | Carr and green 1986 [10] | 66 M | Right maxillary gingiva with left upper arm, scalp, liver deposits | Nil | Died of renal failure, melena, abdominal pain and dyspnoea within few days of diagnosis (disseminated disease) |
| 8 | Kashima et al. 1994 [11] | 39 M | Anterior part of right mandible | mandibulectomy | Died after 3 years (metastasis) |
| 9 | Margiotta et al. 1994 [12] | 62 M | Right hemi mandible (chronic renal insufficiency) | Surgical excision | Follow up not available |
| 10 | Munoz et al. 1998 [13] | 68 M | Mandibular molar area gingiva | Partial mandibulectomy | 1-month post-surgery ➔ tonsillar, floor of mouth recurrence ➔Pharynx, larynx spread, denied any treatment ➔ Died within 2 months of surgery |
| 11 | Abdullah et al. 2000 [14] | 60 F | Mandibular gingiva with scalp, shoulder and back deposits | Treatment Refused | Follow up not available |
| 12 | Loudon et al. 2000 [15] | 68 F | Mandibular gingiva | Surgical excision | Died of local failure and complications (8 months) |
| 13 | Favia et al. 2002 [16] | 65 F | Mandibular gingiva | Radiation plus chemotherapy | Died of disease (3 months) |
| 14 | Favia et al. 2002 [16] | 82 F | Mandibular gingiva | Radiation plus chemotherapy | Died of disease (6 months) |
| 15 | Penner et al. 2002 [17] | 16 F | Right mandibular gingiva | Enbloc resection ➔ right nodal dissection for neck nodal relapse after 3 months➔ Bimodal adjuvant chemotherapy and radiotherapy | Disease free 12 months post-surgery |
| 16 | Florescu et al. 2005 [18] | 70 M | Mandibular gingiva | Surgical excision | Not reported |
| 17 | Driemel et al. 2008 [19] | 63 M | Maxillary gingiva | None | Pleural and ileum metastasis (1 month)➔ ileal segmental resection ➔ died of intestinal bleeding due to disease 2 months post diagnosis. |
| 18 | Uchiyama 2009 [2] | 59 M | Left maxilla | Chemotherapy including celmoleukin and teceleukin➔ partial maxillectomy➔ boron neutron capture therapy and lymphokine activated killer cell treatment | Disease free after 3 years post treatment |
| 19 | Mucke et al. 2010 [20] | 72 M | Maxillary and mandibular gingiva | Surgical excision and then concurrent chemoradiation | Died of disease (6 months) Recurrence |
| 20 | Gordón-Núñez et al. 2010 [21] | 17 F | Left mandibular gingiva | Surgery | Disease free after 14 months |
| 21 | Terada 2011 [22] | 77 M | Mandibular gingiva | Enucleation, planned for radical surgery | Not reported |
| 22 | Suzuki et al. 2011 [23] | 69 F | Right maxillary gingiva | Patient refused surgical treatment, so intra-arterial cisplatin and concurrent radiation | Died after 8 months with multiple lung metastasis |
| 23 | Sumida et al. 2012 [24] | 55 F | Mandibular gingival (anterior part) | Wide excision | Disease free after 4 years |
| 24 | Aditya and lele 2012 [25] | 75 F | Maxillary gingiva | Surgically unresectable. Patient declined further investigation and palliative radiation. | Not reported |
| 25 | Nagata et al. 2014 [3] | 55 M | Mandibular gingiva | Segmental mandibular resection + left radical neck dissection | Thoracic vertebrae metastasis, died of disease (3 months) |
| 26 | Nagata et al. 2014 [3] | 64 M | Maxillary gingiva | Maxillectomy + Bilateral radical neck dissection ➔ Chemotherapy (Cisplatin and Adriamycin) | Lung metastasis after 24 months ➔ lobectomy. No disease 10 months post lobectomy. |
| 27 | Sachadeva et al. 2015 [26] | 52 F | Mandibular gingiva | Hemimandibulectomy | Died in few day (cardiac and respiratory issues) |
| 28 | Hunasgi et al. 2016 [27] | 30 F | Mandibular anterior gingiva | Local excision ➔ Recurrence after 2 months ➔ Wide excision with 2 cm margin | Disease free till 2 years post radical surgery |
| 29 | Chamberland et al. 2016 [28] | 83 M | Mandibular gingiva with bilateral tonsillar and bilateral neck nodal metastasis | Bilateral tonsillectomy and nodal puncture in right level IIa➔After 1 month, bone metastasis, right tonsillar relapse, and gross hematuria➔ paclitaxel 5 cycles + hemostatic RT➔ Mediastinal disease and compression | Died of disease after 4 months of diagnosis of disease. |
| 30 | Aljadeff et al. 2016 [29] | 79 M | Maxillary anterior gingiva | Wide local excision ➔60 Gy of adjuvant radiation | Died 4 months after surgery due to respiratory distress presumably unrelated to disease. |
| 31 | Hartanto and Lau 2018 [30] | 52 F | Right maxillary region with metastasis to lung, liver, bone, multiple lymph nodes at bilateral posterior triangle | Nil | Died in short time after confirmation of diagnosis. |
| 32 | Present case | 30 F | Mandibular gingiva | Central marginal mandibulectomy | No disease (50 months) |
All case reports of primary gingival angiosarcoma were reviewed, excluding head and neck, other oral cavities, and secondary angiosarcomas. PubMed and Google Scholar were searched using the keywords primary gingival angiosarcoma; 31 cases were found to the best of our knowledge. The present series highlights the clinical details, treatment, follow up, and prognosis of 32 patients (including the present case) reported in literature till 2018. Uchiyama et al. reviewed 12 cases of primary gingival angiosarcoma reported until 2009 [2]. Nagata et al. reviewed 15 cases of primary oral angiosarcoma reported until 2014 [3]. Details are given in Table 1.
In the present series, the male to female ratio was 17:15. Age at presentation is extended from 3 months to 86 years, with a median of 62.5 years. The location of the tumor was mandibular gingiva in 21 cases (66%), maxillary gingiva in 9 (28%), and both mandibular and maxillary gingiva in 2 (6%).
Twenty-eight patients had non-metastatic disease (87.5%), and four metastatic disease at presentation (12.5%). Seventeen patients (53%) were treated by surgical modality alone (surgery arm), four patients by combined surgical modality and adjuvant therapy (combined arm) (16%), four primarily by radiation, chemotherapy, or electrofulguration modality (12%), 2 received no treatment (6%).
Seventeen patients who underwent primary surgical modality treatment, 4 died due to the disease at a median period of 5.5 months; two died due to causes unrelated to disease, 8 were disease free at a median follow up of 24 months (including the present case). Follow up was not available for three patients.
Five patients were treated by combined modality treatment with primary surgical treatment and adjuvant radiation therapy with or without chemotherapy. One was disease-free at 3-year follow up. Other patient treated by surgery and adjuvant chemotherapy underwent lobectomy for lung metastasis at 2 years posttreatment and was disease-free 10 months post-lobectomy. Two patients died of disease unrelated to cancer, and one died of disease recurrence at 6 months.
Three of 4 patients treated by radiation and chemotherapy only without surgery died of disease at a median follow up of 6 months period posttreatment, one patient who underwent electrocoagulation ablative therapy was disease free at 27 months of follow up.
Two patients did not undergo any treatment for the primary. One patient developed pleural and ileum metastasis a month after diagnosis and later died of the disease. Others had unresectable maxillary gingival angiosarcoma with extension to paranasal sinuses and infratemporal area.
Discussion
Oral angiosarcoma constitutes only 2% of all angiosarcoma [1]. Among primary oral angiosarcomas, the most common site is tongue, salivary glands, and lip [1]. Gingiva is an infrequent site among all oral subsites for angiosarcoma. Angiosarcoma may present as a bluish macule on the face and scalp, or against a background of chronic lymphedema or in association with exposure to radiation or chronic pyothorax. Symptoms include swelling on gingiva with a history of the recent increase in size, frequently accompanied by bleeding.
Angiosarcoma is an aggressive tumor with an unfavorable prognosis that, despite aggressive multimodality, therapy tends to recur locally and metastasize early most commonly to the lung. Most of them occur within the initial 2–3 years from the diagnosis. The 2-year survival is 15–20% [2,3] It is chemotherapy and radiotherapy resistant. The role of adjuvant therapy is not known. Surgery remains the only form of curative treatment.
As shown in this study, surgery with or without adjuvant treatment, chemotherapy/radiotherapy is the only therapeutic option and remains the cornerstone of the treatment. Long-term survivors were only present in surgery containing arm. The current reviews also show that angiosarcoma is chemo-resistant and radio-resistant. Outcomes were not affected by adjuvant therapy. Neck dissection is necessary if there is any suspicion of lymph node metastases, although the use of prophylactic neck dissection is not warranted. Few selected patients with isolated pulmonary metastasis after a durable disease-free interval post-radical surgery for a primary tumor can be treated with metastasectomy with curative intent.
Owing to the rarity of the disease, only literature available is in the form of case reports. Biology of the disease needs to be studied in detail, and larger prospective multicentric studies need to performed to evaluate the optimal therapy, the role of adjuvant therapy.
Conclusion
Early diagnosis is crucial for survival as the wrong diagnosis can delay definitive treatment. Radical surgery is an only curative option. Even in recurrent cases, timely and adequate surgery can prolong survival. The chemotherapy/radiotherapy role is not established. The role of adjuvant treatment after surgery is not proven.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Syed Nusrath, Email: dr.nusrath2008@gmail.com.
Vipin Goel, Email: vipinrgoel@gmail.com.
KVVN Raju, Email: drkvvnraju2002@yahoo.com.
T Subramanyeshwar Rao, Email: subramanyesh@gmail.com.
LM Chandrashekhar Rao, Email: drlmcsraos@gmail.com.
Sujit Chyau Patnaik, Email: drsujit888@gmail.com.
Sudha Murthy, Email: sudha.s@induscancer.com.
References
- 1.Fanburg-Smith JC, Furlong MA, Childers EL. Oral and salivary gland angiosarcoma: a clinicopathologic study of 29 cases. Mod Pathol. 2003;16(3):263–271. doi: 10.1097/01.MP.0000056986.08999.FD. [DOI] [PubMed] [Google Scholar]
- 2.Uchiyama Y, Murakami S, Kishino M, Furukawa S. A case report of primary gingival angiosarcoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(6):e17–e21. doi: 10.1016/j.tripleo.2009.07.051. [DOI] [PubMed] [Google Scholar]
- 3.Nagata M, Yoshitake Y, Nakayama H, Yoshida R, Kawahara K, Nakagawa Y, Shinohara M. Angiosarcoma of the oral cavity: a clinicopathological study and a review of the literature. Int J Oral Maxillofac Surg. 2014;43(8):917–923. doi: 10.1016/j.ijom.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Henny FA. Angiosarcoma of the maxilla in a 3-month-old infant; report of case. J Oral Surg (Chic) 1949;7(3):250–252. [PubMed] [Google Scholar]
- 5.Blake H, Blake FS. Angiosarcoma; report of a case. Oral Surg Oral Med Oral Pathol. 1956;9(8):821–825. doi: 10.1016/0030-4220(56)90346-2. [DOI] [PubMed] [Google Scholar]
- 6.Quinn JH, McConnell HA, Jr, Leonard GL. Multifocal angiosarcoma of the gingiva: report of case. J Oral Surg. 1970;28(3):215–217. [PubMed] [Google Scholar]
- 7.Albright CR, Shelton DW, Vatral JJ, Hobin FC. Angiosarcoma of the gingiva: report of case. J Oral Surg. 1970;28(12):913–917. [PubMed] [Google Scholar]
- 8.Wesley RK, Mintz SM, Wertheimer FW. Primary malignant hemangioendothelioma of the gingiva: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol. 1975;39(1):103–112. doi: 10.1016/0030-4220(75)90400-4. [DOI] [PubMed] [Google Scholar]
- 9.Piscioli F, Leonardi E, Scappini P, Cristofolini M. Primary angiosarcoma of the gingiva. Case report with immunohistochemical study. Am J Dermatopathol. 1986;8(5):430–435. doi: 10.1097/00000372-198610000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Carr RJ, Green DM. Oral presentation of disseminated angiosarcoma. Br J Oral Maxillofac Surg. 1986;24(4):277–285. doi: 10.1016/0266-4356(86)90094-x. [DOI] [PubMed] [Google Scholar]
- 11.Kashima K, Igakura Y, Komura M, Hamada M, Arima R, Sakoda S. Three gingival tumors derived from vascular endothelial cells: a case of hemangioendothelioma and two cases of angiosarcoma. Nihon Koku Shuyo Gakkaishi. 1994;6:251–261. [Google Scholar]
- 12.Margiotta V, Florena AM, Giuliana G. Primary angiosarcoma of the alveolar mucosa in a haemodialysis patient: case report and discussion. J Oral Pathol Med. 1994;23(9):429–431. doi: 10.1111/j.1600-0714.1994.tb00090.x. [DOI] [PubMed] [Google Scholar]
- 13.Muñoz M, Monje F, del Hoyo JA, Martín-Granizo R. Oral angiosarcoma misdiagnosed as a pyogenic granuloma. J Oral Maxillofac Surg. 1998;56(4):488–491. doi: 10.1016/s0278-2391(98)90719-4. [DOI] [PubMed] [Google Scholar]
- 14.Abdullah BH, Yahya HI, Talabani NA, Alash NI, Mirza KB. Gingival and cutaneous angiosarcoma. J Oral Pathol Med. 2000;29(8):410–412. doi: 10.1034/j.1600-0714.2000.290807.x. [DOI] [PubMed] [Google Scholar]
- 15.Loudon JA, Billy ML, DeYoung BR, Allen CM. Angiosarcoma of the mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2000;89(4):471–476. doi: 10.1016/s1079-2104(00)70127-2. [DOI] [PubMed] [Google Scholar]
- 16.Favia G, Muzio LL, Serpico R, Maiorano E. Angiosarcoma of the head and neck with intra-oral presentation. A clinico-pathological study of four cases. Oral Oncol. 2002;38(8):757–762. doi: 10.1016/s1368-8375(02)00045-3. [DOI] [PubMed] [Google Scholar]
- 17.Penner C, Grist W, Müller S. Epithelioid angiosarcoma presenting in the gingiva of an adolescent. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2002;94(2):205–216. [Google Scholar]
- 18.Florescu M, Simionescu C, Margaritescu C, Georgescu CV. Gingival angiosarcoma: histopathologic and immunohistochemical study. Romanian J Morphol Embryol. 2005;46(1):57–61. [PubMed] [Google Scholar]
- 19.Driemel O, Müller-Richter UD, Hakim SG, Bauer R, Berndt A, Kleinheinz J, Reichert TE, Kosmehl H. Oral acantholytic squamous cell carcinoma shares clinical and histological features with angiosarcoma. Head Face Med. 2008;4(1):17. doi: 10.1186/1746-160X-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mücke T, Deppe H, Wolff KD, Kesting MR. Gingival angiosarcoma mimicking necrotizing gingivitis. Int J Oral Maxillofac Surg. 2010;39(8):827–830. doi: 10.1016/j.ijom.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 21.Gordon-Nunez MA, Lopes MF, Maia AP, Galvão HC. Intraoral epithelioid hemangioendothelioma: a case report and review of the literature. Med Oral Patolog Oral Cir Bucal. 2010;15(2):e340–e346. [PubMed] [Google Scholar]
- 22.Terada T. Angiosarcoma of the oral cavity. Head Neck Pathol. 2011;5(1):67–70. doi: 10.1007/s12105-010-0211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suzuki G, Ogo E, Tanoue R, Tanaka N, Watanabe Y, Abe T, Iwamoto O, Kusukawa J, Hayabuchi N. Primary gingival angiosarcoma successfully treated by radiotherapy with concurrent intra-arterial chemotherapy. Int J Clin Oncol. 2011;16(4):439–443. doi: 10.1007/s10147-010-0145-7. [DOI] [PubMed] [Google Scholar]
- 24.Sumida T, Murase R, Fujita Y, Ishikawa A, Hamakawa H. Epulis-like gingival angiosarcoma of the mandible: a case report. Int J Clin Exp Pathol. 2012;5(8):830–833. [PMC free article] [PubMed] [Google Scholar]
- 25.Aditya A, Lele S. A nodular growth on maxillary gingiva. Indian J Dent Res. 2012;23(1):116–119. doi: 10.4103/0970-9290.99054. [DOI] [PubMed] [Google Scholar]
- 26.Sachdeva SK, Dutta S, Rout P. Angiosarcoma of mandible: An uncommon clinical entity. Int J Appl Basic Med Res. 2015;5(2):142. doi: 10.4103/2229-516X.157172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hunasgi S, Koneru A, Vanishree M, Manvikar V. Angiosarcoma of anterior mandibular gingiva showing recurrence–a case report with immunohistochemistry. J Clin Diagn Res. 2016;10(7):ZD01–ZD04. doi: 10.7860/JCDR/2016/18497.8080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chamberland F, Maurina T, Degano-Valmary S, Spicarolen T, Chaigneau L. Angiosarcoma: a case report of gingival disease with both palatine tonsils localization. Rare Tumors. 2016;8(3):113–117. doi: 10.4081/rt.2016.5907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aljadeff L, Fisher CA, Wolf SL, Byrd KM, Curtis W, Ward BB, Munz SM, Fullen DR, McHugh JB, Danciu TE. Red exophytic mass of the maxillary anterior gingiva. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(4):379–384. doi: 10.1016/j.oooo.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartanto FK, Lau SH. A case report of Angiosarcoma of maxillary gingiva: histopathology aspects. Sci Dent J. 2018;2(2):77–83. [Google Scholar]