Abstract
Background
Portal vein embolization (PVE) is performed to reduce the risk of liver failure and subsequent mortality after major liver resection. Although a cut‐off value of 2·7 per cent per min per m2 has been used with hepatobiliary scintigraphy (HBS) for future remnant liver function (FRLF), patients with perihilar cholangiocarcinoma (PHC) potentially benefit from an additional cut‐off of 8·5 per cent/min (not corrected for body surface area). Since January 2016 a more liberal approach to PVE has been adopted, including this additional cut‐off for HBS of 8·5 per cent/min. The aim of this study was to assess the effect of this approach on liver failure and mortality.
Methods
This was a single‐centre retrospective study in which consecutive patients undergoing liver resection under suspicion of PHC in 2000–2015 were compared with patients treated in 2016–2019, after implementation of the more liberal approach. Primary outcomes were postoperative liver failure (International Study Group of Liver Surgery grade B/C) and 90‐day mortality.
Results
Some 191 patients with PHC underwent liver resection. PVE was performed in 6·4 per cent (9 of 141) of the patients treated in 2000–2015 and in 32 per cent (16 of 50) of those treated in 2016–2019. The 90‐day mortality rate decreased from 16·3 per cent (23 of 141) to 2 per cent (1 of 50) (P = 0·009), together with a decrease in the rate of liver failure from 19·9 per cent (28 of 141) to 4 per cent (2 of 50) (P = 0·008). In 2016–2019, 24 patients had a FRLF greater than 8·5 per cent/min and no liver failure or death occurred, suggesting that 8·5 per cent/min is a reliable cut‐off for patients with suspected PHC.
Conclusion
The major decrease in liver failure and mortality rates in recent years and the simultaneous increased use of PVE suggests an important role for PVE in reducing adverse outcomes after surgery for PHC.
The use of portal vein embolization (PVE) in patients undergoing major liver resection for perihilar cholangiocarcinoma at the authors' centre increased from 6·4 per cent in 2000–2015 to 32 per cent in 2016–2019. This increased use of PVE coincided with a major decrease in the postoperative liver failure rate, from 19·9 to 4 per cent, and a decrease in the 90‐day mortality rate, from 16·3 to 2 per cent. Using hepatobiliary scintigraphy, an additional cut‐off for future remnant liver function of 8·5 per cent/min (not corrected for body surface area) correlated with safe liver resection in patients with suspected perihilar cholangiocarcinoma.
Portal vein embolization decreases rates of liver failure and mortality
Antecedentes
La embolización de la vena porta (portal vein embolization, PVE) se realiza para reducir el riesgo de insuficiencia hepática y de mortalidad asociada después de una resección hepática mayor. Aunque con la gammagrafía hepato‐biliar (hepato‐biliary scintigraphy, HBS) se ha utilizado un punto de corte de 2,7%/min/m2 para la función hepática remanente futura (future remnant liver function, FRLF), los pacientes con colangiocarcinoma perihilar (perihilar cholangiocarcinoma, PHC) se beneficiarían potencialmente de un punto de corte adicional de 8,5%/min (no corregido para el área de superficie corporal). Desde enero de 2016, se adoptó un enfoque más liberal para la PVE, incluyendo este punto de corte adicional para la HBS de 8,5%/min. El objetivo de este estudio fue evaluar el efecto de este enfoque sobre la insuficiencia hepática y la mortalidad.
Métodos
Se trata de un estudio retrospectivo de un solo centro, en el que los pacientes consecutivos sometidos a resección hepática por sospecha de PHC entre 2000‐2016 se compararon con los pacientes tratados entre 2016‐2019, después de la implementación de un enfoque más liberal. Los objetivos primarios fueron la insuficiencia hepática postoperatoria (ISGLS grado B/C) y la mortalidad a los 90 días.
Resultados
Un total de 191 pacientes con PHC se sometieron a resección hepática. Se realizó PVE en el 6% (9/141) de los pacientes antes de 2016 y en el 32% (16/50) de los pacientes después de 2016. La mortalidad disminuyó del 16% (23/141) al 2% (1/50) (P = 0,009), junto con una disminución de la insuficiencia hepática del 20% (28/141) al 4% (2/50) (P = 0,008). Después de 2016, 20 pacientes tuvieron un FRLF > 8,5%/min y no se produjo insuficiencia hepática o mortalidad, lo que sugiere que el 8,5%/min es un punto de corte fiable para los pacientes con sospecha de PHC.
Conclusión
La disminución marcada de la insuficiencia hepática y de la mortalidad en los últimos años y el aumento simultáneo del uso de la PVE, sugiere que la PVE ha jugado un importante papel en el descenso de los resultados adversos después de la cirugía para el PHC.
Introduction
Radical resection of perihilar cholangiocarcinoma (PHC) is the only treatment that offers a chance of long‐term survival1. Extended procedures, consisting of combined liver and extrahepatic bile duct resection, are often required, and are associated with high morbidity and mortality rates2.
Mortality rates in Western series range from 6 to 18 per cent3, 4, 5, whereas rates in Eastern series are lower, ranging from 1 to 4 per cent6, 7. Several studies have addressed the particular differences in outcomes between these parts of the world; along with several differences in treatment strategy, the more frequent use of portal vein embolization (PVE) in Eastern series was considered to be the most striking difference2, 8, 9. Differences in the indication for PVE appear to exist, as a recent study8 comparing the present authors' results with those of a large centre in Japan showed that, although preoperative future remnant liver volume shares were comparable between the two cohorts, PVE was done in 55 per cent of the Eastern and 7 per cent of the Western patients. Of note, the indocyanine green retention rate at 15 min was used to assess liver function in Japan, whereas in the present authors' centre liver function was assessed using hepatobiliary scintigraphy (HBS).
In recent years, strategies to select patients for PVE have been developed that include other risk factors besides future remnant liver volume and function using HBS10, 11. Although the cut‐off value for future liver function was set at 2·7 per cent per min per m2 in the general population of patients undergoing major liver resection, this cut‐off may not be the same for all patients undergoing major liver resection. The work‐up of patients with PHC for resection is known to be complex, specifically related to preoperative biliary drainage, and postoperative outcomes are generally worse compared with those following other indications for major liver resection. Therefore, this subgroup of patients requires a different approach compared with that used for patients who undergo resection for colorectal liver metastases, for example. Based on previously published receiver operating characteristic (ROC) curve analysis of the 2000–2015 cohort, a cut‐off of 8·5 per cent/min resulted in the best predictive value for patients with PHC11. In that study, the correction for body surface area (BSA) seemed not to increase the predictive value of future liver remnant function (FLRF) for liver failure, leading to an uncorrected cut‐off with regard to BSA. Therefore, an additional cut‐off for FLRF of 8·5 per cent/min in patients with PHC was added to the authors' strategy11. These studies have resulted in an altered treatment strategy, using a more liberal approach to PVE in an attempt to improve postoperative outcomes by reducing the risk of liver failure. However, the preoperative work‐up of patients with PHC can be challenging and, although PVE is considered a safe and effective procedure, surgical resection is not attained in all patients undergoing PVE12.
This study aimed to assess the effect of the more liberal approach to PVE on postoperative outcomes, in particular postoperative liver failure and mortality.
Methods
All consecutive patients who had surgical resection with suspected PHC between January 2000 and October 2019 at the Academic Medical Centre of Amsterdam UMC were included in the study. Data were obtained retrospectively from a maintained database. Patient management and work‐up have been described in detail previously11, 13, 14. HBS is the current modality of choice for remnant liver assessment, and liver volumes are determined only when there is a discrepancy in the results obtained by HBS or at the surgeon's request. Since the report on the effect of preoperative liver function on postoperative outcomes comprising the 2000–2015 cohort, the policy for application of PVE was changed. From 2016 the new cut‐off without correction for BSA for liver function of 8·5 per cent/min was adopted for patients with PHC based on the ROC curves of the previously published study11. In the present study, the latter cut‐off value was therefore used.
All patients with PHC undergoing PVE between 2000 and 2019 were identified, regardless of whether or not they underwent resection. The need for ethical approval and individual informed consent was waived by the Institutional Medical Ethics Committee (W19_114).
Primary outcomes
The primary outcomes of the present study were postoperative liver failure and mortality. Liver failure was defined and graded according to the International Study Group of Liver Surgery (ISGLS) criteria15, with only grades B and C considered as clinically relevant. Postoperative mortality was defined as death within 90 days of surgery.
Variables
Major liver resection was defined as the resection of at least three Couinaud liver segments (with or without segment I). All postoperative complications within 30 days of surgery were scored and graded according to the Clavien–Dindo classification16. Biliary leakage and postoperative haemorrhage were scored and graded according to the respective ISGLS criteria, and only grades B and C were considered clinically relevant15, 17. Patients undergoing PVE who did not reach surgical resection were identified, and the reasons for not undergoing resection were recorded. Preoperative cholangitis was defined as an episode of fever, leucocytosis or raised C‐reactive protein level, and malaise requiring additional biliary drainage before resection18.
Statistical analysis
Categorical variables are presented as numbers with percentages and tested using either the χ2 or Fisher's exact test. Continuous variables that followed a normal distribution are presented as mean(s.d.) values and compared with Student's t test. Continuous variables that did not follow a normal distribution are presented as median (i.q.r.) values and tested using the Mann–Whitney U test. Two‐tailed P < 0·050 was considered statistically significant. All statistical analyses were performed with SPSS® version 25 (IBM, Armonk, New York USA) and figures were generated using GraphPad Prism® version 7 (GraphPad, La Jolla, California, USA).
Results
A total of 215 patients were included in the study; 164 (76·3 per cent) were operated on in 2000–2015 and the remaining 51 (23·7 per cent) between January 2016 and October 2019. Twenty‐four patients who underwent external bile duct resection without liver resection were excluded from the analysis regarding PVE and liver volume and function. Baseline patient and operative characteristics of the 191 patients who had concomitant liver resection are shown in Table 1. The characteristics of the two cohorts from 2000–2015 (141 patients) and 2016–2019 (50) were similar, although a higher proportion of patients in the later cohort had no biliary drainage: 14 of 50 (28 per cent) versus 18 of 141 patients in the earlier cohort (P = 0·013). Type of biliary drainage (endoscopic, percutaneous, or both) did not differ significantly between the groups (P = 0·242). Preoperative cholangitis appeared to occur more often in the 2016–2019 cohort: 23 of 50 (46 per cent) versus 47 of 141 (33·3 per cent) in the 2000–2015 cohort (P = 0·101).
Table 1.
Baseline patient and disease characteristics
| 2016–2019 (n = 50) | 2000–2015 (n = 141) | P ‡ | |
|---|---|---|---|
| Age (years) * | 65(11) | 63(10) | 0·231§ |
| Sex ratio (F : M) | 21 : 29 | 53 : 88 | 0·582 |
| BMI (kg/m 2 ) † | 23 (22–26) | 22 (20–26) | 0·974¶ |
| ECOG performance status | 0·285 | ||
| 0 | 30 (60) | 98 (69·5) | |
| 1 | 13 (26) | 35 (24·8) | |
| 2 | 6 (12) | 7 (5·0) | |
| 3 | 1 (2) | 1 (0·7) | |
| ASA grade | 0·190 | ||
| I | 5 (10) | 30 (21·3) | |
| II | 37 (74) | 88 (62·4) | |
| III | 8 (16) | 23 (16·3) | |
| Jaundice at presentation | 33 (66) | 104 (73·8) | 0·295 |
| Biliary drainage | 36 (72) | 123 (87·2) | 0·013 |
| Type of biliary drainage | 0·242 | ||
| Percutaneous transhepatic | 5 (14) | 11 (8·9) | |
| Endoscopic | 23 (64) | 67 (54·5) | |
| Both | 8 (22) | 45 (36·6) | |
| Preoperative cholangitis | 23 (46) | 47 (33·3) | 0·101 |
| Bismuth type | 0·134 | ||
| I | 0 (0) | 0 (0) | |
| II | 0 (0) | 4 (2·8) | |
| IIIA | 33 (66) | 70 (49·6) | |
| IIIB | 9 (18) | 44 (31·2) | |
| IV | 8 (16) | 23 (16·3) | |
| Portal vein embolization | 16 (32) | 9 (6·4) | < 0·001 |
| Resection type | 0·432 | ||
| Left hemihepatectomy | 17 (34) | 57 (40·4) | |
| Extended left hemihepatectomy | 2 (4) | 6 (4·3) | |
| Right hemihepatectomy | 16 (32) | 33 (23·4) | |
| Extended right hemihepatectomy | 15 (30) | 40 (28·4) | |
| Central/minor liver resection | 0 (0) | 5 (3·5) | |
| Portal vein reconstruction | 8 (16) | 38 (27·0) | 0·120 |
Values in parentheses are percentages unless indicated otherwise; values are
mean(s.d.) and
median (i.q.r.). ECOG, Eastern Cooperative Oncology Group.
χ2 or Fisher's exact test, except
Student's t test and
Mann–Whitney U test.
Portal vein embolization
Of the 191 patients who underwent liver resection, 25 (13·1 per cent) had preoperative PVE. PVE was done in nine (6·4 per cent) of the 141 patients treated before 2016 and in 16 (32 per cent) of the 50 treated later (P < 0·001). Postoperative outcomes for patients undergoing liver resection in both time frames are shown in Table 2. There was a reduction in the rate of liver failure, from 19·9 per cent (28 of 141) in 2000–2015 to 4 per cent (2 of 50) in 2016–2019 (P = 0·008). The reduction in liver failure was accompanied by a decreased 90‐day mortality rate, from 16·3 per cent (23 of 141) to 2 per cent (1 of 50) (P = 0·009).
Table 2.
Postoperative outcomes after liver resection
| 2016–2019 (n = 50) | 2000–2015 (n = 141) | P * | |
|---|---|---|---|
| Major morbidity (Clavien–Dindo grade ≥ IIIA) | 26 (52) | 82 (58·2) | 0·451 |
| Liver failure (grade B/C) | 2 (4) | 28 (19·9) | 0·008 |
| Biliary leakage (grade B/C) | 16 (32) | 45 (31·9) | 0·991 |
| Bleeding (grade B/C) | 2 (4) | 12 (8·5) | 0·293 |
| Drainage of intra‐abdominal abscess | 17 (35) | 56 (39·7) | 0·534 |
| 90‐day mortality | 1 (2) | 23 (16·3) | 0·009 |
Values in parentheses are percentages.
χ2 or Fisher's exact test.
The largest liver resections associated with the highest risk of liver failure are generally right liver resections and, as expected, the use of PVE in patients undergoing either a right or extended right hepatectomy increased from nine of 73 (12 per cent) in the earlier cohort to 16 of 31 (52 per cent) in the later cohort (P < 0·001). Liver failure and mortality had not generally decreased over time, but markedly dropped from 2016 (Fig. 1), coinciding with the more liberal policy in the use of PVE.
Figure 1.
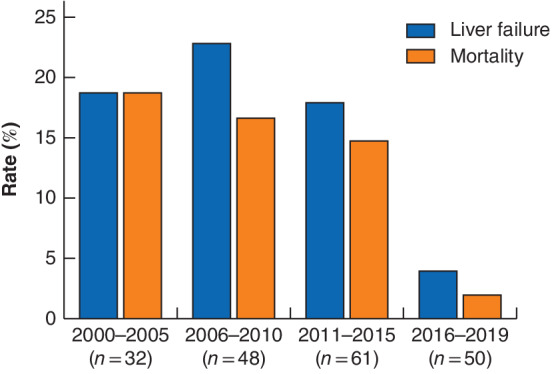
Evolution of liver failure and mortality rates over time
Liver function
Based on a study performed in the authors' department11, a specific cut‐off of 8·5 per cent/min appeared safer for patients with PHC with a negative predictive value of 94% compared to the general cut‐off of 2·7 per cent per min per m2 with a negative predictive value of 82% in the 2000–2015 cohort. In the 2016–2019 cohort, future remnant liver function (FRLF) data were available for 49 of the 50 patients. Twenty‐four of these 49 patients had a baseline FRLF of 8·5 per cent/min or higher (3 after PVE), and none had postoperative liver failure or died. Among the 25 patients with FRLF below 8·5 per cent/min, two developed liver failure (Fig. 2).
Figure 2.
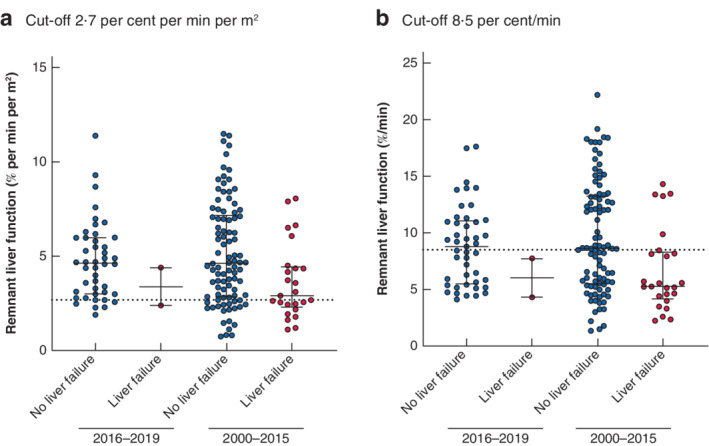
Remnant liver function in patients with and without liver failure in the 2000–2015 and 2016–2019 cohorts a Cut‐off 2·7 per cent per min per m2; b cut‐off 8·5 per cent/min. Bars represent median (i.q.r.).
In the 2016–2019 cohort, 43 of the 49 patients had preoperative remnant liver function above the general cut‐off of 2·7 per cent per min per m2. Ten of these 43 patients underwent PVE to reach this cut‐off value for liver function; one of them experienced fulminant postoperative liver failure leading to death within 90 days of surgery. Although the outcome was fatal in only one of these 43 patients, these findings suggest that the 2·7 per cent per min per m2 cut‐off was insufficient in this group of high‐risk patients with PHC (Fig. 2).
Six patients underwent resection with a remnant liver function below 2·7 per cent per min per m2, of whom three had undergone PVE. The other three patients, without PVE, all had a favourable postoperative course. Although considered in these patients, PVE was not performed owing to their expected low risk; none had experienced preoperative cholangitis and two patients did not need biliary drainage. Of the three patients who did have PVE, one recovered from grade B liver failure. In the other two patients PVE did not result in a remnant liver function above 2·7 per cent per min per m2 or 8·5 per cent/min, but they had a resection despite the higher risk as no curative alternative was available after already having undergone PVE.
There were ten patients who underwent PVE, but with no subsequent surgical resection. In seven of these patients unresectability was determined during explorative laparotomy, owing to positive distant (N2) lymph nodes (3 patients), distant metastases (1), extensive vascular involvement (2) and severe main portal vein thrombosis (1). In two patients follow‐up CT performed after PVE showed liver metastases, and in one patient resection was cancelled due to an insufficient hypertrophy response after PVE.
Discussion
In this single‐centre study of a large cohort of patients undergoing resection for suspected PHC, the rates of liver failure and 90‐day mortality decreased from 19·9 and 16·3 per cent in 2000–2015 to 4 and 2 per cent respectively in 2016–2019. This major drop in adverse events coincided with the increased use of PVE in the later cohort of up to 32 per cent, compared with only 6·4 per cent in 2000–2015.
PVE was first reported19 about 30 years ago, and has since evolved into the standard procedure for preoperative enhancement of the future remnant liver, reducing the risk of liver failure and mortality12. PVE is most effective in combination with compromised liver parenchyma20. As most patients with PHC suffer from longstanding cholestasis and usually require extensive liver resection, high rates of PVE may be expected. Many Eastern series21, 22 indeed report frequent use of PVE of up to 60 per cent, in contrast to most Western series10, 23, 24 that use PVE in only 4–24 per cent of patients.
In a recent direct comparison8 of the present cohort with a large series from Japan, the differential use of PVE across the globe was demonstrated, with a rate of 7 per cent (14 of 210) in the West compared with 54·9 per cent (90 of 164) in the East. This coincided with a halved mortality in the East, although outcomes were similar after propensity score matching, suggesting that use of PVE relates directly to favourable outcomes8. These findings may explain the higher operative mortality rate of 6–18 per cent in Western series4, 5, compared with 1–4 per cent in the East2, 6, 7.
Preoperative cholangitis is a significant risk factor for postoperative mortality5, 24, and has been associated with operative mortality rates of up to 25 per cent25. Generally, in patients undergoing PVE, unilateral biliary drainage of only the future remnant liver is undertaken. Preoperative biliary drainage was increasingly omitted in patients with a sufficient future remnant liver volume (above 40–50 per cent) or FRLF greater than 3·5 per cent per min per m2, resulting in a lower percentage of biliary drainage after 2015. In contrast, the rate of preoperative cholangitis increased from 33·3 per cent before 2016 to 46 per cent in patients operated on after 1 January 2016. PVE prolongs the duration of biliary drainage and thus negatively influences the risk of cholangitis. However, although cholangitis occurred in 46 per cent of the 2016–2019 cohort, the rates of liver failure and 90‐day mortality were low. This suggests that the benefits of PVE greatly outweigh the risks of the longer time to surgery, along with the risk of developing cholangitis. The high incidence of cholangitis is likely to be explained by the liberal definition, which differs from other definitions that may require a positive bile culture for example, as bile samples are not always obtained (for instance with endoscopic drainage)24.
Based on findings in the 2000–2015 cohort, the suggested remnant liver function for safe liver resection in patients with PHC was adjusted from 2·7 per cent per min per m2 to 8·5 per cent/min11. The previous analysis11 showed that use of the 2·7 per cent per min per m2 cut‐off still frequently resulted in liver failure in patients with a function above the cut‐off value. Therefore, a 8·5 per cent/min cut‐off (uncorrected for BSA) was devised, with a high negative predictive value (94 per cent), meaning that the risk of liver failure is very low when liver function is measured above this value. The zero postoperative liver failure and mortality rates in patients in the 2016–2019 cohort with a FRLF above 8·5 per cent/min confirmed that resection can be undertaken safely in these patients. This can therefore be considered a validation of this cut‐off value. Although not all patients below the 8·5 per cent/min cut‐off underwent PVE, it was considered for all these patients, and the associated, more liberal, approach to PVE resulted in improved outcomes. PVE can be omitted safely in patients with a function above 8·5 per cent/min, whereas PVE should be considered carefully in every patient with a function below 8·5 per cent/min.
In the three patients who did not reach the 2·7 per cent per min per m2 or 8·5 per cent/min cut‐off after PVE, the increased surgical risk was accepted and they did undergo resection, as the alternative would have been palliation with a dismal prognosis; other alternatives, such as ALPPS (associated liver partition and portal vein ligation for staged hepatectomy), are currently associated with unacceptable outcomes26. A preliminary study27 examining dual embolization of both the portal and hepatic vein has shown promising results, and may help to induce a large hypertrophic response in patients with a very small remnant liver. Of the ten patients in the present study who had PVE not followed by resection, the reason for not proceeding to resection was the lack of a sufficient hypertrophic response in only one patient, whereas in the other patients the finding of advanced disease precluded resection. In the later cohort a strict policy was applied that precluded patients with a bilirubin level above 50 μmol/l from undergoing HBS because of the competitive uptake of mebrofenin with bilirubin, leading to potentially false low assessments of functional capacity. This also enforced the policy of achieving complete biliary drainage of the future liver remnant in patients with resectable PHC. Using these changes in the work‐up of patients, functional assessment is now used mainly to guide preoperative management, and volume assessment is no longer part of standard practice in the authors' institution.
This study has several limitations, mostly due to its retrospective nature. Although the study protocol was designed prospectively following the analysis of the 2000–2015 cohort11, it was still subject to selection bias. The decrease in liver failure coincided with the liberal implementation of PVE, but it is possible that other unmeasured factors, such as improved intraoperative or patient‐specific factors, influenced this association. However, no gradual decline in liver failure and mortality was observed over time, as would be expected with improved perioperative management, but there was a sudden drop in liver failure and mortality starting in 2016. In addition, the 141 patients operated on between 2000 and 2015 were compared with a smaller group of 50 patients treated between 2016 and 2019, within a much shorter time frame. In the future, a comparison of two more equal groups is needed to confirm these findings. The inclusion of multiple centres would potentially enhance the validity of the analyses; however, there is much improvement needed in the implementation of HBS among centres treating these complex patients. Notwithstanding these facts, the present study findings can be considered a preliminary prospective validation of the previous HBS analyses performed11. The structural application of PVE in patients planned for extensive liver resection with low FRLF, and perhaps also in patients who had preoperative cholangitis, potentially reduces adverse outcomes and ultimately offers more patients the chance of long‐term survival.
Acknowledgements
T.M.v.G. and P.B.O. have shared last authorship.
Disclosure: The authors declare no conflict of interest.
Funding information
No funding
References
- 1. Cillo U, Fondevila C, Donadon M, Gringeri E, Mocchegiani F, Schlitt HJ et al Surgery for cholangiocarcinoma. Liver Int 2019; 39: 143–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Franken LC, Schreuder AM, Roos E, van Dieren S, Busch OR, Besselink MG et al Morbidity and mortality after major liver resection in patients with perihilar cholangiocarcinoma: a systematic review and meta‐analysis. Surgery 2019; 165: 918–928. [DOI] [PubMed] [Google Scholar]
- 3. Popescu I, Dumitrascu T. Curative‐intent surgery for hilar cholangiocarcinoma: prognostic factors for clinical decision making. Langenbecks Arch Surg 2014; 399: 693–705. [DOI] [PubMed] [Google Scholar]
- 4. Hemming AW, Mekeel K, Khanna A, Baquerizo A, Kim RD. Portal vein resection in management of hilar cholangiocarcinoma. J Am Coll Surg 2011; 212: 604–613. [DOI] [PubMed] [Google Scholar]
- 5. Olthof PB, Coelen RJ, Wiggers JK, Besselink MG, Busch OR, van Gulik TM. External biliary drainage following major liver resection for perihilar cholangiocarcinoma: impact on development of liver failure and biliary leakage. HPB (Oxford) 2016; 18: 348–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Furusawa N, Kobayashi A, Yokoyama T, Shimizu A, Motoyama H, Miyagawa S. Surgical treatment of 144 cases of hilar cholangiocarcinoma without liver‐related mortality. World J Surg 2014; 38: 1164–1176. [DOI] [PubMed] [Google Scholar]
- 7. Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y et al Evolution of surgical treatment for perihilar cholangiocarcinoma: a single‐center 34‐year review of 574 consecutive resections. Ann Surg 2013; 258: 129–140. [DOI] [PubMed] [Google Scholar]
- 8. Olthof PB, Miyasaka M, Koerkamp BG, Wiggers JK, Jarnagin WR, Noji T et al A comparison of treatment and outcomes of perihilar cholangiocarcinoma between Eastern and Western centers. HPB (Oxford) 2019; 21: 345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kimura N, Young AL, Toyoki Y, Wyatt JI, Toogood GJ, Hidalgo E et al Radical operation for hilar cholangiocarcinoma in comparable Eastern and Western centers: outcome analysis and prognostic factors. Surgery 2017; 162: 500–514. [DOI] [PubMed] [Google Scholar]
- 10. Olthof PB, Wiggers JK, Groot Koerkamp B, Coelen RJ, Allen PJ, Besselink MG et al Postoperative liver failure risk score: identifying patients with resectable perihilar cholangiocarcinoma who can benefit from portal vein embolization. J Am Coll Surg 2017; 225: 387–394. [DOI] [PubMed] [Google Scholar]
- 11. Olthof PB, Coelen RJS, Bennink RJ, Heger M, Lam MF, Besselink MG et al 99mTc‐mebrofenin hepatobiliary scintigraphy predicts liver failure following major liver resection for perihilar cholangiocarcinoma. HPB (Oxford) 2017; 19: 850–858. [DOI] [PubMed] [Google Scholar]
- 12. van Lienden KP, van den Esschert JW, de Graaf W, Bipat S, Lameris JS, van Gulik TM et al Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol 2013; 36: 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rassam F, Roos E, van Lienden KP, van Hooft JE, Klümpen HJ, van Tienhoven G et al Modern work‐up and extended resection in perihilar cholangiocarcinoma: the AMC experience. Langenbecks Arch Surg 2018; 403: 289–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coelen RJ, Olthof PB, van Dieren S, Besselink MG, Busch OR, van Gulik TM. External validation of the estimation of physiologic ability and surgical stress (E‐PASS) risk model to predict operative risk in perihilar cholangiocarcinoma. JAMA Surg 2016; 151: 1132–1138. [DOI] [PubMed] [Google Scholar]
- 15. Rahbari NN, Garden OJ, Padbury R, Brooke‐Smith M, Crawford M, Adam R et al Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011; 149: 713–724. [DOI] [PubMed] [Google Scholar]
- 16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 2011; 149: 680–688. [DOI] [PubMed] [Google Scholar]
- 18. van der Gaag NA, de Castro SM, Rauws EA, Bruno MJ, van Eijck CH, Kuipers EJ et al Preoperative biliary drainage for periampullary tumors causing obstructive jaundice; DRainage vs. (direct) OPeration (DROP‐trial). BMC Surg 2007; 7: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P et al Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery 1990; 107: 521–527. [PubMed] [Google Scholar]
- 20. Farges O, Belghiti J, Kianmanesh R, Regimbeau JM, Santoro R, Vilgrain V et al Portal vein embolization before right hepatectomy: prospective clinical trial. Ann Surg 2003; 237: 208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yokoyama Y, Ebata T, Igami T, Sugawara G, Mizuno T, Yamaguchi J et al The predictive value of indocyanine green clearance in future liver remnant for posthepatectomy liver failure following hepatectomy with extrahepatic bile duct resection. World J Surg 2016; 40: 1440–1447. [DOI] [PubMed] [Google Scholar]
- 22. Sano T, Shimada K, Sakamoto Y, Esaki M, Kosuge T. Changing trends in surgical outcomes after major hepatobiliary resection for hilar cholangiocarcinoma: a single‐center experience over 25 years. J Hepatobiliary Pancreat Surg 2007; 14: 455–462. [DOI] [PubMed] [Google Scholar]
- 23. Nuzzo G, Giuliante F, Ardito F, Giovannini I, Aldrighetti L, Belli G et al Improvement in perioperative and long‐term outcome after surgical treatment of hilar cholangiocarcinoma: results of an Italian multicenter analysis of 440 patients. Arch Surg 2012; 147: 26–34. [DOI] [PubMed] [Google Scholar]
- 24. Ribero D, Zimmitti G, Aloia TA, Shindoh J, Fabio F, Amisano M et al Preoperative cholangitis and future liver remnant volume determine the risk of liver failure in patients undergoing resection for hilar cholangiocarcinoma. J Am Coll Surg 2016; 223: 87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wiggers JK, Groot Koerkamp B, Cieslak KP, Doussot A, van Klaveren D, Allen PJ et al Postoperative mortality after liver resection for perihilar cholangiocarcinoma: development of a risk score and importance of biliary drainage of the future liver remnant. J Am Coll Surg 2016; 223: 321–331.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Olthof PB, Coelen RJS, Wiggers JK, Groot Koerkamp B, Malago M, Hernandez‐Alejandro R et al High mortality after ALPPS for perihilar cholangiocarcinoma: case–control analysis including the first series from the international ALPPS registry. HPB (Oxford) 2017; 19: 381–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hwang S, Ha TY, Ko GY, Kwon DI, Song GW, Jung DH et al Preoperative sequential portal and hepatic vein embolization in patients with hepatobiliary malignancy. World J Surg 2015; 39: 2990–2998. [DOI] [PubMed] [Google Scholar]


