The coronavirus disease 2019 (COVID-19) pandemic has altered endoscopic practice significantly because severe acute respiratory syndrome–coronavirus 2 is present in the gastrointestinal tract and may be aerosolized during upper and lower endoscopy.1 Societal recommendations have been published to guide screening processes, personal protective equipment (PPE) use, and procedure prioritization2 , 3; however, their uptake remains unclear. Additionally, pediatric endoscopy has unique considerations, including a higher proportion of mild or asymptomatic COVID-19, preferential usage of anesthesiologist-administered deep sedation or general anesthesia, and more frequent gastrointestinal symptoms at the time of endoscopy.4 This is the first study to explore the impact of COVID-19 on pediatric endoscopic practice worldwide and to compare differences across regions and between areas with differing COVID-19 case burdens.
Methods
An online Research Electronic Data Capture survey was distributed to pediatric gastroenterologists in April 2020 using an e-mail listserve targeting pediatric gastroenterologists affiliated with the European and North American Societies for Pediatric Gastroenterology, Hepatology, and Nutrition. The pretested survey anonymously recorded information regarding institutional demographics, current pediatric endoscopic practice patterns, and changes in endoscopic practice, including COVID-19 screening processes and PPE use. Detailed methodology is provided in Appendix 1.
Results
Respondent Characteristics
There were 145 responses from distinct institutions worldwide, representing 27 different countries, with 24.1% (n = 35) from Europe, 57.9% (n = 84) from North America, and 17.9% (n = 26) from countries in other continents. Most were free-standing children’s hospitals (59.3%, n = 86) and in regions regulated by a stay-at-home/quarantine order (90.3%, n = 131) for a mean duration of 26 ± 12 days before survey completion. Eighty-nine institutions (61.4%) were from regions with ≥10,000 cases at time of survey completion, and 70 (48.3%) were from regions with ≥100/100,000 after normalization by population.
Changes in Endoscopic Practice
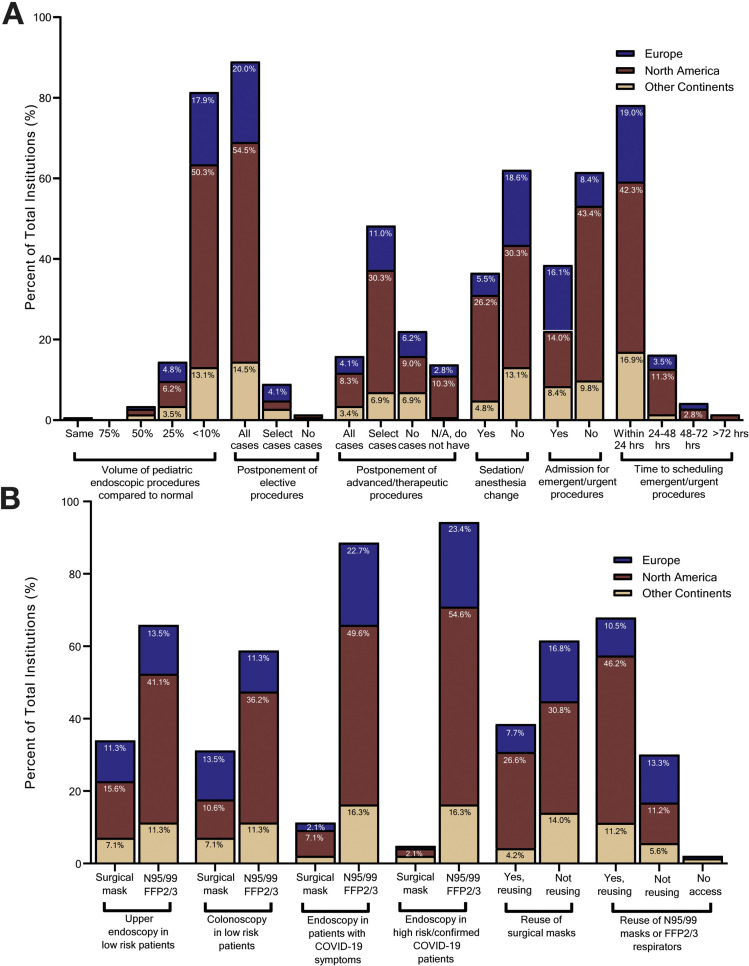
Pediatric endoscopy volumes decreased to <10% of normal at most institutions (81.4%, n = 118), and 89.6% (129/144) postponed all elective cases (Figure 1 A). Most were not rescheduling postponed procedures (53.1%, n = 77), and 69.7% (n = 101) had no defined plan to address the backlog. Emergent/urgent cases were not delayed at 88.3% of institutions (n = 128). One hundred twelve institutions (78.3%) continued emergent/urgent procedures for patients with suspected or confirmed COVID-19. Notably, triage criteria for procedures were lacking; only half (n = 69) reported using guidelines to classify procedural urgency.
Figure 1.
Pediatric endoscopic practice changes during the COVID-19 pandemic. (A) Survey responses divided by geographic region, including Europe, North America, and countries in other continents. Questions reflect common changes in pediatric endoscopic practice since the onset of the COVID-19 pandemic. (B) Survey responses divided by geographic region, including Europe, North America, and countries in other continents. Questions reflect mask usage during various endoscopic procedures and mask reuse. FFP, filtering face piece.
Modified staffing for endoscopy was reported by 53.5% of institutions (77/144), and 60.1% (86/143) restricted the number of personnel permitted in the endoscopy suite. Only 17.2% (n = 25) continued to allow unrestricted fellow participation in procedures; 33.1% (n = 48) barred trainee participation completely.
Endoscopy-related COVID-19 Screening and Testing
COVID-19 screening practices varied, with 78.5% of institutions (113/144) screening patients before and on the endoscopy day and 6.25% (9/144) not performing any screening. Only 53.1% (n = 77) screened for gastrointestinal symptoms. Five institutions (3.4%) inquired about loss of smell or taste. Most (95.1%, 136/143) measured body temperature. Nearly 80% (110/141) had protocols to address a positive screen. After endoscopy, only 18.4% of institutions (n = 26/141) followed-up about new COVID-19 diagnoses and/or symptoms.
Thirty-one percent of institutions (44/143) tested for COVID-19 before all endoscopies, 24.5% (35/143) tested select cases, and 44.8% (64/143) did not test. Of those testing, most used nasopharyngeal swabs (96.2%, 76/79) and had a turnaround time of <24 hours (93.7%, 74/79). Over 90% of institutions had no known COVID-19 exposures from patients (129/143) or caregivers (130/143); however, 71.6%, (101/141) had protocols in place if such exposure did occur.
Changes in Personal Protective Practices
The location of endoscopy did not change at 67.4% of institutions (97/144). Only 44.8% (64/143) had negative pressure rooms in their endoscopy unit. Thirty-three institutions (23.1%) used them for all procedures, whereas 21.7% (31/143) used them for select cases. Anesthesia practices changed for 37.1% (53/143), with more institutions uniformly performing endotracheal intubation for all procedures.
There was variation in use of full airborne, contact, and droplet PPE precautions compared with contact and droplet precautions alone (Supplementary Table 1). Reuse of surgical masks was reported by 38.5% of institutions (55/143), and 67.8% (97/143) reused N95/N99 masks or filtering face piece 2/3 respirators (Figure 1 B).
Survey Responses Stratified by Region
Fewer North American institutions admitted patients for emergent/urgent cases compared with Europe (P = .00001) or other countries (P = .0171). Compared with North America, countries on other continents were less likely to classify procedural urgency using guidelines (P = .0065) and to postpone emergent/urgent cases (P = .0129) and advanced endoscopic procedures (P = .0059). North American institutions rescheduled fewer postponed cases compared with Europe (P = .0060). Fellows were less likely to be involved in endoscopic procedures in Europe compared with North America (P = .0037) and other countries (P = .0005).
Screening questions differed across regions, with European centers asking significantly more gastrointestinal symptom questions (P < .001). PPE use also varied, with European countries using fewer N95/N99 masks in high-risk or confirmed COVID-19 patients (P = .002) compared with North America.
Survey Responses Stratified by COVID-19 Cases
Regions with ≥10,000 COVID-19 cases were more likely to use full PPE precautions for all upper (P = .039) and lower endoscopies (P = .0418), less likely to postpone emergent/urgent cases (P = .0094), and more likely to have established protocols pertaining to endoscopy-related COVID-19 exposure (P = .0461) (Supplementary Table 2). Institutions with ≥100/100,000 COVID-19 cases more frequently inquired about gastrointestinal symptoms (diarrhea, P = .0385; vomiting, P = .0091).
Institutions in regions with ≥10,000 COVID-19 cases were also more likely to diagnose celiac disease using European Society of Paediatric Gastroenterology, Hepatology, and Nutrition nonendoscopic diagnostic criteria (P = .0327) and inflammatory bowel disease without endoscopy (P = .00362). Most institutions reported still using endoscopy to guide management of eosinophilic esophagitis.
Discussion
Our study demonstrates significant pediatric endoscopic practice variation across institutions worldwide and highlights relevant differences in practice across geographic regions and differential COVID-19 case burdens. European institutions were more likely to inquire about gastrointestinal symptoms and recent travel compared with North America, likely reflecting earlier experience with COVID-19. Additionally, areas with a higher case burden were more likely to use full PPE precautions. Only 59.2% of institutions reported using full precautions for all procedures, demonstrating continued variation among institutions despite societal guidelines.2 , 3 Reuse of masks was high, and most institutions reported concerns about PPE supply, underscoring the implications of PPE scarcity.5
Pediatric endoscopy volumes have been impacted significantly in line with adult practice,6, 7, 8 with over 80% of pediatric institutions operating at <10% of normal procedural volumes and 98.6% of institutions postponing elective procedures. Most institutions had no defined plans for rescheduling, highlighting the need for guidance as regions start to reopen. Future study of rebooking processes and outcomes of patients affected by these cancellations will be important to re-evaluate which indications for pediatric endoscopy are pertinent.
This study provides real-world data highlighting the drastic impact COVID-19 has had on pediatric endoscopic practice worldwide. As the pandemic evolves, this information will be useful to help inform practices and streamline guidelines in a manner that balances safety issues and practicability and to inform strategies for resumption of endoscopic services.
Acknowledgment
The following members of the International Pediatric Endoscopy COVID-19 Alliance also contributed to this study: Raoul I Furlano, MD, PhD, Paediatric Gastroenterology and Nutrition, University Children's Hospital Basel, Basel, Switzerland; and Mike Thomson, MBChB, DCH, MD, International Academy of Paediatric Endoscopy Training, Sheffield Children’s Hospital NHS Foundation Trust, Sheffield, United Kingdom.
CRediT Authorship Contributions
Wenly Ruan, MD (Conceptualization: Equal; Data curation: Equal; Formal analysis: Lead; Investigation: Equal; Methodology: Equal; Project administration: Equal; Writing – original draft: Lead; Writing – review and editing: Equal). Douglas S Fishman, MD (Conceptualization: Supporting; Data curation: Supporting; Formal analysis: Supporting; Investigation: Supporting; Methodology: Supporting; Project administration: Supporting; Resources: Supporting; Supervision: Supporting; Writing – original draft: Supporting; Writing – review and editing: Supporting). Diana G Lerner, MD (Conceptualization: Supporting; Formal analysis: Supporting; Investigation: Supporting; Methodology: Supporting; Writing – review and editing: Supporting). Melinda A Engevik, PhD (Data curation: Supporting; Formal analysis: Supporting; Writing – review and editing: Supporting). B. Joseph Elmunzer, MD, MSc (Conceptualization: Supporting; Formal analysis: Supporting; Investigation: Supporting; Methodology: Supporting; Writing – review and editing: Supporting). Catharine M Walsh, MD, MEd, PhD (Conceptualization: Lead; Data curation: Lead; Formal analysis: Equal; Investigation: Lead; Methodology: Lead; Project administration: Lead; Resources: Lead; Supervision: Lead; Writing – original draft: Equal; Writing – review and editing: Lead).
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding Wenly Ruan is supported by grant 5T32DK007664-28 from the National Institutes of Health. Catharine M. Walsh holds a Career Development Award from the Canadian Child Health Clinician Scientist Program and an Early Researcher Award from the Ontario Ministry of Research and Innovation. The funders had no role in the design and conduct of the review, decision to publish and preparation, review, or approval of the manuscript.
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at https://doi.org/10.1053/j.gastro.2020.05.068.
Contributor Information
International Pediatric Endoscopy COVID-19 Alliance:
Supplementary Material
References
- 1.Repici A. Gastrointest Endosc. 2020;92:192–197. doi: 10.1016/j.gie.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sultan S. Gastroenterology. 2020;159:739–758. doi: 10.1053/j.gastro.2020.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walsh C.M. J Pediatr Gastroenterol Nutr. 2020;70:741–750. doi: 10.1097/MPG.0000000000002750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong Y. Pediatrics. 2020;145:e20200702. [Google Scholar]
- 5.Rex D.K. Gastroenterology. 2020;159:1167–1169. doi: 10.1053/j.gastro.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forbes N. Gastroenterology. 2020;159:772–774. doi: 10.1053/j.gastro.2020.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahadev S. Gastrointest Endosc. 2020;92:788–789. doi: 10.1016/j.gie.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garbe J. Gastroenterology. 2020;159:778–780. doi: 10.1053/j.gastro.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.