Abstract
As the backbone for the treatment of patients with coronavirus disease 2019 (COVID-19), nurses have been playing key roles in cabin hospitals, isolation wards, and intensive care units for critical cases. Anesthesia nurses have their own professional specialties, such as airway management, the use and maintenance of life support equipment, including ventilators, and the use of high-flow oxygen equipment. With rich experience in emergency responses and nursing, anesthesia nurses, along with emergency nurses and critical care nurses, play important roles during the treatment of patients with COVID-19. In our hospital, 27 of 34 anesthesia nurses participated in the front-line fight against COVID-19 and did an excellent job. Anesthesia care by nurses is relatively new in China, and the role of anesthesia nurses during a disaster response has not been fully appreciated. Given their specialty, anesthesia nurses have played important roles in the treatment of patients with COVID-19. We hope that authorities will consider including anesthesia nurses in national disaster response medical rescue teams.
Keywords: anesthesia nurse, coronavirus disease 2019, medical rescue team
In the month before New Year's Day 2020, the coronavirus disease 2019 (COVID-19) outbreak began in Wuhan, Hubei Province, China, and quickly spread throughout China. COVID-19 is an acute respiratory infection that is mainly transmitted via respiratory droplets and contact. All age groups are susceptible. The disease is highly contagious with a short onset period and a long incubation period.1 COVID-19 poses severe challenges to the public health emergency response system in China, and is a serious threat to public health and life. In the wake of the epidemic, the Chinese government responded quickly by sending medical rescue teams across China to Hubei. Most of the team members were from respiratory medicine, infectious disease medicine, critical care medicine, and emergency medicine. In particular, anesthesia nurses played an important role in the treatment of patients with COVID-19, thanks to their specialties in airway management. In this article, we discuss the specialties and roles of anesthesia nurses in this front-line work.
Background
Role and Responsibility of Nurses in the Treatment of Patients With COVID-19
Nurses are the backbone of the medical emergency response system. They work with other health care professionals on the front lines and play key roles during emergency responses.2 On February 29, 2020 Yanhong Guo, Ombudsman of the National Health Commission's Medical Administration Bureau, mentioned at the Press Conference of the Joint Prevention and Control Mechanism of the State Council that more than 42,000 health care professionals around China had been dispatched to Hubei, of whom 28,600 (68%) were nurses (Table 1 ). During the treatment of patients with COVID-19, nurses provided meticulous care, treatment, monitoring, and mental support, thereby playing key roles in COVID-19 prevention and control. Nurses worked closely with doctors to promote patient recovery and improve treatment outcomes.3
Table 1.
Composition of the Medical Team Members Dispatched to Hubei During the COVID-19 Outbreak
| Medical Team Members | Nurses | Doctors and Other Professionals | |
|---|---|---|---|
| n | 42,000 | 28,600 | 13,400 |
| % | 68 | 32 |
COVID-19, coronavirus disease 2019.
Severe COVID-19 is associated with a critical and rapidly evolving condition and includes multiple organ failure and multiple complications. The treatments are often complex, involving a very high workload for nurses and high requirements for technical skills. During treatment, careful monitoring, close cooperation between doctors and nurses, and attention to the holistic care of patients with critical disease are essential for improving patient outcomes. Patients with COVID-19 face severe mental challenges. In addition to nursing and treatment, nurses are able to promptly ease a patient's psychological concerns while enhancing the courage to overcome COVID-19.
Current Status of Anesthesia Care by Nurses in China
Anesthesia care by nurses is relatively new in China and was established to align with the development of modern anesthesiology.4 The title “anesthesia nurse” was officially proposed internationally in 1861 to adapt to the rapid development of anesthesiology.5 Anesthesia care by nurses is relatively new in China, and the education program is only 20 years old and still in its infancy.6
In December 2017, the General Office of the National Health and Family Planning Commission of People's Republic of China issued Management of the Outpatient and Nursing Unit Setup for the Anesthesiology Department in Medical Institutions, and proposed that medical centers set up anesthesia care units when possible to improve anesthesia care.7 In August 2018, seven ministries, including the National Health Commission, jointly issued Opinions on Strengthening and Improving Anesthesia Care. Thus, the central government executed a strategy for the development of anesthesia care, with a focus on the overall framework of anesthesia care and the responsibilities of anesthesia nurses.8
At present, anesthesia nurses in China mainly include anesthesia monitoring nurses, general care nurses, and postanesthesia care unit (PACU) nurses. They participate in preoperative visits, the assessment of patients, and the development of anesthesia plans under the supervision of a licensed anesthesiologist. Moreover, they prepare patients for anesthesia and monitor patients during the operation based on each patient's condition and anesthesia plan; they are also responsible for postanesthesia care, patient transfer, and postoperative follow-up. Currently, about 10 universities or colleges have an anesthesia nursing education program. Graduates who get nurse practitioner certificates are trained as anesthesia monitoring nurses, general care nurses, or PACU nurses according to the hospitals' need.
Key Considerations for COVID-19 Care
Patients with COVID-19 should be isolated in designated hospitals with effective isolation and protection measures. Patients with suspected cases and confirmed cases should be admitted to separate areas. No visitors are allowed during isolation. During hospitalization, patients should wear surgical masks and receive appropriate medical care based on their condition and physician orders.9
Common Cases
The following measures are recommended for patients with common cases of COVID-19: absolute bed rest, good nutrition, vital sign monitoring based on each patient's condition, medical care based on physician orders, maintain an unobstructed respiratory tract, timely and effective oxygen therapy, mental support, and effective communication.
Severe Cases
The following measures are recommended for patients with severe cases of COVID-19: the aforementioned measures, oxygen therapy, life care, monitoring temperature, respiratory rhythm, frequency, and depth, blood oxygen saturation, monitor level of consciousness and systemic symptoms, and life support as needed.
Patients Receiving Noninvasive Ventilator-Assisted Ventilation
These patients should be monitored for blood oxygen saturation and receive humidification, skin care, and mental support. Noninvasive ventilator-assisted ventilation is mechanical ventilation without as artificial airway, such as tracheal intubation or tracheotomy.
Patients Requiring Tracheal Intubation or Tracheotomy and an Artificial Airway
For these patients, closed sputum aspiration should be performed, along with airway management under the level III personal protective equipment (PPE) (Figure 1 ). The level III PPE includes positive pressure air breathing apparatuses, multilayer protective clothing, N95 masks, goggles, gloves, and foot covers and is mainly used to protect staff with high-risk exposure positions in the infectious disease department, intensive care units, and isolation wards where patients with COVID-19 were treated.
Figure 1.
The level III personal protective equipment. This figure is available in color online at www.jopan.org
Mental Assessment and Support
Patients in isolation are prone to fear, anxiety, anger, loneliness, and sleep disorders, thereby requiring proper assessment of their mental status and needs. Nurses should carefully evaluate changes in patients' cognition, emotional responses, and behaviors; intervene and help patients adapt; provide proper emotional support; encourage patients to exhibit confidence in overcoming the disease; provide ongoing information support; and alleviate uncertainty and anxiety.
Skin Care
Skin care should be performed, and stress injuries should be prevented.
Anesthesia Nurses in the Front-Line Fight
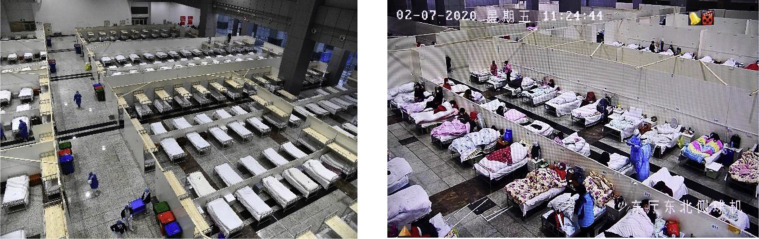
As medical centers strive to treat as many patients with COVID-19 as possible in China, front-line nurses in respiratory medicine and infectious disease medicine faced high workload and stress levels. Proper shifts and support from nurses from other departments have helped alleviate the stress experienced by front-line nurses. Of the 34 anesthesia nurses at our hospital, 27 experienced nurses supported front-line work at some point and worked at fever clinics, isolation wards, intensive care units, and cabin hospitals to provide medical treatment and care and mental support for patients with COVID-19 (Table 2 ). The few nurses who did not participate were responsible for the normal operation of the anesthesiology department. Cabin hospitals (Figure 2 ), also called makeshift hospitals (Fangcang in Chinese), are large, temporary hospitals built by converting public venues, such as stadiums and exhibition centers, into health care facilities to isolate patients with mild to moderate symptoms of an infectious disease from their families and communities, while providing medical care, disease monitoring, food, shelter, and social activities.10
Table 2.
Participation in Front-Line Work by Anesthesia Nurses From Our Hospital
| Isolation Ward | Intensive Care Unit | Fever Clinic | Cabin Hospital | Total | |
|---|---|---|---|---|---|
| Anesthesia nurses participating in front-line work | 14 | 7 | 5 | 1 | 27 |
| Total number of anesthesia nurses | 34 | ||||
Figure 2.
The largest cabin hospital in Wuhan managed by Union Hospital. (Left) Before patient admission; (Right) after patient admission. This figure is available in color online at www.jopan.org
In general, anesthesia nurses primarily work in the PACU for postoperative care. They monitor patient breathing, circulation, consciousness, muscle strength, and blood oxygen saturation; prevent common complications; manage respiratory emergencies; and transfer patients to his or her ward after the patient is fully awake. They have extensive clinical experience in airway management, monitoring patient conditions, emergency response, mental care, and safe transfer, all of which give them unique advantages in the treatment and management of patients with COVID-19.
Anesthesia nurses are experienced in patient transport. The transport of critically ill patients is a high-risk procedure. It is challenging to ensure the safety of critically ill patients during transport. Studies have shown that up to 71% of patients endure mild to severe complications during transport or examination.11 However, the transport of critically ill patients during a crisis is an important task. In particular, life support and monitoring during transport requires senior medical staff with transport experience; notably, the transport of critically ill patients is a daily task in the PACU. Anesthesia nurses are better equipped than other nurses to handle this task.
Anesthesia nurses have more experience in personal protection. They routinely work in an operating room and are familiar with surgical gowns, gloves, eye protection, surgical caps, masks, and even barrier gowns. They are superior to other nurses with respect to the acceptance of and adaptability to PPE. During the severe acute respiratory syndrome epidemic in 2003, personal protection was the main source of stress for nurses. COVID-19 is more contagious than severe acute respiratory syndrome. Nurses must wear multilayer PPE, including multilayer protective clothing, masks, gloves, foot covers, and eye protection, which can cause breathing problems and hypoxia. Eye protection and caps block vision and hearing; gloves reduce the hand's tactile sensation and increase the difficulty of nursing procedures. As a result, the difficulty of completing work tasks is greatly increased, with high stress and workload levels. Moreover, nurses unfamiliar with isolation and protection and intensive care are prone to mental stress, physical burnout, and even other complications.
Anesthesia nurses have extensive experience in emergency response. COVID-19 mainly targets the lungs. Symptoms include dry cough, fever, acute respiratory distress syndrome, and even respiratory failure, multiple organ failure, and cardiac arrest. As a result, nurses face high levels of stress. During the postanesthesia stage, postoperative patients are prone to hypoxemia because of respiratory tract obstruction and respiratory depression and subsequently hypoxic agitation,12 blood pressure fluctuations and insufficient perfusion of major organs, delayed recovery of consciousness, and cardiac arrest because of massive postoperative bleeding and other reasons. Anesthesia nurses have unique advantages over other nurses in the management of hypoxemia, cardiac arrest, and cardiopulmonary resuscitation of patients with COVID-19. In general, anesthesia nurses are more experienced or more skilled than are other nurses during an emergency airway and respiratory emergency.
Anesthesia nurses are experienced in respiratory and life support. Patients with severe COVID-19 require respiratory support, and the use of a ventilator has become routine in the treatment of patients with COVID-19. Anesthesia nurses routinely use ventilators during the postanesthesia care of patients undergoing general anesthesia, including setting up respiratory support and respiratory parameters, adjusting respiratory modes and respiratory parameters based on patient recovery, and assisting the anesthesiologist when removing the tracheal tube for general anesthesia and sputum aspiration. Therefore, anesthesia nurses have unparalleled experience in respiratory and life support, which are critical skills in the emergency response to COVID-19.
Conclusions
Anesthesia nurses have unique airway and respiratory management skills and experience, and can quickly adapt to the treatment and management of patients with COVID-19. However, anesthesia nurses lack experience in the prevention and control of infectious diseases, which is also the case for most nurses from noninfectious disease departments. Anesthesia nurses routinely work in operating rooms and, thus, may lack experience in the nursing procedures in regular wards and in patient communication, which are two shortcomings. Therefore, anesthesia nurses require training in emotional management and communication.
Footnotes
Conflict of interest: none to report.
Q.C., X.L., and Z.Z. are co-first authors. P.G. and S.Y. are co-senior authors.
References
- 1.National Health Commission of the PRC Diagnosis and Treatment Protocol for COVID-19 (Trial Version 7) 2020. https://www.chinadaily.com.cn/pdf/2020/1.Clinical.Protocols.for.the.Diagnosis.and.Treatment.of.COVID-19.V7.pdf Available at: Accessed March 3, 2020.
- 2.Li Z., Li X. Development and new mission of disaster relief care. Chin J Nurs. 2016;08:901–902. [Google Scholar]
- 3.Press Conference of the Joint Prevention and Control Mechanism of the State Council on February 29, 2020. 2020. http://www.nhc.gov.cn/xcs/fkdt/202002/f6557445863a447f87014e514263dd91.shtml Available at: Accessed February 29, 2020.
- 4.Chen Q., Zhao Z., Hu S., Xing L. Research on current status of anesthesia care in secondary and tertiary hospitals in Hubei province. J Nurs Sci. 2018;08:33–35. [Google Scholar]
- 5.Stewart M.W. Research news: Nurse anesthesia. J Perianesth Nurs. 2011;26:176–178. doi: 10.1016/j.jopan.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Jiang L., Ruan H., Wang J. Development and the research status quo of anesthesia nursing. Chin Nurs Res. 2009;23:2829–2831. [Google Scholar]
- 7.National Health Commission of the PRC Management of the Outpatient and Nursing Unit Setup for the Anesthesiology Department in Medical Institutions. 2017. Available at: http://www.nhc.gov.cn/yzygj/s3593/201712/251fb61008bc487797ed18a3a15c1337.shtml. Accessed December 12, 2017.
- 8.National Health Commission of the PRC National Development and Reform Commission of the PRC, Ministry of Education of the PRC, Ministry of Finance of the PRC, Ministry of Human Resources and Social Security of the PRC, National Administration of Traditional Chinese Medicine of the PRC, National Healthcare Security Administration of the PRC. Opinions on strengthening and improving anesthesia care. 2018. Available at: http://www.nhc.gov.cn/yzygj/s3594q/201808/4479a1dbac7f43dcba54e6dce873a533.shtml. Accessed August 17, 2018.
- 9.National Health Commission of the PRC Standardardized Nursing Management of Severe and Critical Patient with COVID-19. 2020. Available at: http://www.nhc.gov.cn/yzygj/s7653p/202003/8235a35f35574ea79cdb7c261b1e666e/files/f4269c33b5a94135a124609252595613.pdf. Accessed February 29, 2020.
- 10.Chen S., Zhang Z., Yang J. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet. 2020;395:1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Day M.W. Transport of the critically ill: The Northwest MedStar experience. Crit Care Nurs Clin North Am. 2005;17:183–190. doi: 10.1016/j.ccell.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Wang S., Zhang L., Han W. Risk assessment and preventive nursing on respiratory complication after general anesthesia in post-anesthesia care unit. Int J Anesthesiol Resuscitation. 2018;19:148–152. [Google Scholar]