Abstract
Background
As a result of the COVID-19 pandemic, there has been a significant disruption of the practice of pharmacy. Importantly, in many parts of the world, this disruption occurred literally overnight, requiring pharmacists to demonstrate significant adaptability and resiliency in order to manage continuing and in some cases expanding needs of patients.
Objectives
The objective of this research was to characterize how community pharmacy in Ontario (Canada) responded to the COVID-19 pandemic of winter/spring 2020, in particular in understanding what factors may influence or predict resiliency of individual practitioners and their workplaces.
Methods
One-on-one interviews mediated through technology (Microsoft Teams) were used, following a semi-structured interview protocol. Verbatim transcripts were produced and analyzed by two independent researchers, using an inductive coding process to identify and characterize themes.
Results
A total of 21 pharmacists participated in this study. Six themes were identified: a) use of and comfort with technology; b) early adoption of corporate and professional guidance; c) workplaces that emphasized task-focus rather than multi-tasking were more resilient; d) scheduling methods and practices in the workplace are important for personal resilience; e) dedicated specialty staff allowed pharmacists to focus on their work; and f) provision of personal protective equipment was essential.
Conclusions
Traditionally, resilience in professional practice has been characterized as a personal, not a workplace, issue. This study suggests that personal resiliency for pharmacists requires substantial workplace support; further work in this area is required to better understand how pharmacists adapt to complex and difficult situations such as pandemics.
Context
In 2007, we published a paper describing the experiences of community pharmacists in Ontario, Canada during two “unprecedented” times of civil crisis: the Sudden Acute Respiratory Syndrome (SARS) outbreak of 2003 and the disruption of the electrical transmission grid across the eastern part of North America in 2005.1 This paper described how community pharmacists managed to maintain services and provide care despite the extraordinary circumstances confronting them. This paper noted that such a study was necessary because “… (e)mergencies and civil crises will continue to occur”. We also noted that “… (t)he need for pharmacists and pharmacy services continues and likely increases during times of civic disaster, yet the basic infrastructure necessary to support these services may be severely compromised or nonexistent. The reality of emergencies and disasters, however, is that they are frequently unpredictable and of a scale and magnitude that defies imagination or preplanning.“1
In late 2019, in Wuhan, China, a novel coronavirus infection triggered what would eventually become one of the most impactful, global disruptions in living memory. Within four months this infection had travelled across the globe, resulting in millions of infections, hundreds of thousands of deaths, and triggering one of the sharpest declines in economic productivity ever experienced.2 On March 11, 2020, the World Health Organization (WHO) declared a global pandemic.3 Local and national responses to this crisis varied significantly, but in many cases wholesale population-wide lockdowns and targeted quarantines were mandated affecting literally billions of people world-wide simultaneously.4 The scale and magnitude of this event truly did defy imagination or pre-planning … yet health care professionals like pharmacists were required to continue to provide service and care to patients5 – and in many cases, expand their repertoire of clinical skills to assume new and even more challenging responsibilities.6 , 7
At the time of writing of this paper, the full story of the novel coronavirus is still being written, and in many places around the world there is great uncertainty as to what – if anything – will come next. While many parts of the world have now loosened lockdown restrictions and attempted some semblance of a return to pre-pandemic normalcy, there are significant concerns that follow-up waves of infection may continue indefinitely and that traditional activities of human life will be forever altered.8 At this particular juncture – the pause between what may become several successive waves of outbreak and lockdown – there is a unique opportunity to capture the experiences of community pharmacists in managing their practices and providing care and service to patients during the first unexpected wave of coronavirus, in order to potentially enhance resilience (responsiveness, adaptability, and confidence) in managing whatever may come next.
Background
Pandemic planning and readiness has been discussed across health systems for many years. In 2003, Cox, Tamblyn, and Tam (who eventually went on to become Canada's Chief Public Health Officer) described principles for effective pandemic planning in the context of influenza.9 This paper served as an important point of reference for subsequent influenza outbreaks including H1N1, Middle Eastern Respiratory Syndrome (MERS) and Avian Flu in the years following SARS.10 This paper described the foundations of pandemic preparedness in terms of public health principles related to coordination of activities across diverse agencies (locally, nationally, and globally), the importance of measurement and monitoring, and the value of population-wide preventative initiatives such as vaccination. Shearer et all presciently published on the topic of incorporation of decision analysis into infectious disease pandemic planning and response in early 2020, highlighting the importance of system planning and policy flexibility required to ensure all aspects of the health care system – but particularly primary care – coordinate effectively to keep populations safe and healthy and reduce strain on tertiary care during emergencies.11
Fitzgerald et al. highlighted the significant potential role of community pharmacies within a system-wide public-health led planning program focused on influenza pandemic.12 They noted that – in 2016 – there were discussions and formal commitment to including community pharmacies in pandemic readiness protocols but there were few effective examples of successful integration. Traynor – in 2008 – noted that “pharmacists matter in pandemic response”, and highlighted the ways in which pharmacies and pharmacists could and should serve a more useful role in society-wide pandemic preparedness: beyond simply being a place where vaccinations can be administered, community pharmacies could become decentralized primary care service hubs, triaging patients prior to accessing family doctors or emergency rooms, and providing more direct hands-on support for medication therapy management at the patient and community level.13 Her comments reflected our own findings regarding the experience of community pharmacy in Ontario during the SARS outbreak of 2003: at a time when emergency rooms are overwhelmed and doctors’ offices were beyond capacity, community pharmacies rapidly emerged as the first point of primary care contact for many patients uncertain of where to go or what to do – and community pharmacists ended up providing a level of care, service, and triage well above what they were accustomed to providing in the past.1
The importance of psychological resilience is a particularly important issue during times of significant social upheaval, particularly for health professionals.14 , 15 Resilience is traditionally described as the ability to adapt to and maintain psychological equilibrium during times of high stress16 - such as the unexpected workload surge that occurs during pandemic, or the situational ambiguity that arises when public health guidance appears to be constantly in flux. Resilience has been described as a way of mitigating or preventing burnout17 or ensuring that routine occupational stress does not lead to more severe psychological consequences.18 Recently, there has been significant interest in the topic of resilience in pharmacy practice,19 independent of issues associated with pandemic. A variety of proactive individual/personal strategies – including mindfulness, meditation, and psychotherapy – have been proposed to enhance resilience, better manage burnout, and prevent the worst effects of occupational stress,20, 21, 22 but there has been little formal research into this issue in the context of community pharmacy practice. Importantly, there has been scant attention paid to organizational/workplace strategies that can enhance resiliency of the individuals working within community pharmacies,23 instead putting the onus on individual pharmacists to manage their own mental health and wellness albeit with the support of (in some cases) employer assistance programs.
In the 2020 coronavirus pandemic, pharmacists in China were amongst the first to experience the full brunt of the outbreak. Liu et al. recently published their commentary reflecting upon how the experiences of Chinese pharmacists on the front lines may be an important lesson for the rest of the world, as the infection spread globally.24 They identified a broad swathe of issues, including management of drug shortages/hoarding, the provision of public health education, management of medication-related issues at times when prescribers were not available for consultation, etc. They highlight the importance of rapid adaptability and resiliency of individual practitioners, municipal public health authorities, and regional and national governance to respond to rapidly changing circumstances of this pandemic.
Globally and nationally, many pharmacy organizations have drafted guidance documents to support pharmacists during times of pandemic. The International Pharmaceutical Federation (FIP) has published Guidelines for Pharmacists and the Pharmacy Workforce to manage COVID-19.25 This document highlights several core responsibilities for pharmacists, including stewardship of the medication supply chain, patient education, appropriate triaging to other health care providers, and provision of public health measures including vaccinations. Initially produced in 2009, the Canadian Pharmacists' Association “Pharmacists' Guide to Pandemic Preparedness” focused on practical strategies to support community pharmacy, including methods to safeguard personal health, how to manage supply chain problems and backlogs of patients flocking to pharmacies, and how to initiate infection control programs within a retail environment.26 Similarly, the Royal Pharmaceutical Society (UK) recently published its “Guidance on ethical, professional decision-making in the COVID-19 pandemic, highlighting the importance of cognitive/clinical services provision and providing support for decision making related to rationing, managing when policy is ambiguous or absent, and interprofessional collaboration.27 The American Pharmacists' Association (in conjunction with the American Society of Health-System Pharmacists) and the National Association of Chain Drug Stores) first produced “A Pharmacist's Guide to Pandemic Preparedness” in 2007, providing similar guidance to that of their Canadian and British counterparts.28 During the first months of the 2020 pandemic, APhA provided significant daily updates and briefing to pharmacists across the country, dealing with topical issues such as the role of hydroxychloroquine or bleach disinfectant,29 in response to widely-publicized claims of efficacy. Despite more than a decade of reasonable assurance regarding the eventual emergence of a pandemic similar to COVID-19, it is unclear whether pandemic preparedness guidance documents such as these truly mattered or supported front-line practitioners, particularly given the ferocity and speed with which the virus spread and the society-wide lockdown that resulted. Further, given the magnitude of the pandemic and its expected long-standing impact on daily life, society, the economy, and health care there are unique opportunities to study – in real-time – how community pharmacies have responded to COVID-19.
Research question
The objective of this research was to characterize how community pharmacy in Ontario responded to the COVID-19 pandemic of winter/spring 2020. In particular, we were interested in understanding what factors may influence or predict resiliency and adaptability of individual practitioners and their workplaces, in light of the extraordinary circumstances of the time.
Method
Despite having undertaken similar research following the 2003 SARS outbreak, the context of this research was unique and as a result required significant flexibility and adaptability on the part of the researchers themselves. In order to gather contextually rich data and provide research participants in this research with the opportunity to fully co-create the data set for analysis through discussion, reflection, and articulation of their lived experiences during the pandemic, it was clear that a qualitative, interview-based data gathering method was essential. However, given the society-wide need for social distancing, traditional face-to-face interviews with audiotaping were simply not an option during this time. Alternative methods (e.g. reflective writing using logbooks or diaries) were rejected for data gathering as these were deemed both intrusive and time-consuming, and unlikely to yield the same depth as an interactive conversation between researcher and participant.
Ultimately, technologically enabled face-to-face interviewing using the Microsoft Teams© application was identified as the optimal data gathering strategy at this time, mindful of the reality that this method would mean certain pharmacists who either lacked access or were uncomfortable with video-based teleconferencing methods might be excluded. To provide alternative access to these individuals, traditional phone-based interviewing was also made available for participants who preferred this alternative, mindful of the fact that these participants would not be visible to the researcher and as a result, non-verbal responses transmitted by facial or gestural cues may be missed, thereby creating an asymmetry in data collection within the participant pool.30
A combination of convenience and snowball sampling methods were used to recruit potential participants in this study. Inclusion criteria for this study were: a) licensed pharmacist in Ontario for a minimum of 3 years; b) working minimum of 24 h/week on average over last three years; c) practiced for a minimum of 2 years in community pharmacy; d) practicing in community pharmacy from January 1, 2020 to present time (so as to have experienced first-hand COVID-19 related issues in practice); and e) English language fluency sufficient to provide informed consent. An initial invitation to participate in an interview-based study examining pharmacists’ responses to COVID-19 was posted on social media sites (including Facebook and via email). In addition, those who had participated in previous interview-based research (on different topics) were also contacted by email and invited to participate in this study. Those who responded were provided with additional information regarding the study remit and logistics, asked to complete informed consent, and then offered different time slots for interview via Teams or telephone. During this process, these individuals were invited to also share study recruitment information with friends or colleagues who they thought might be interested in participating in this study. No compensation was available for participation in this study.
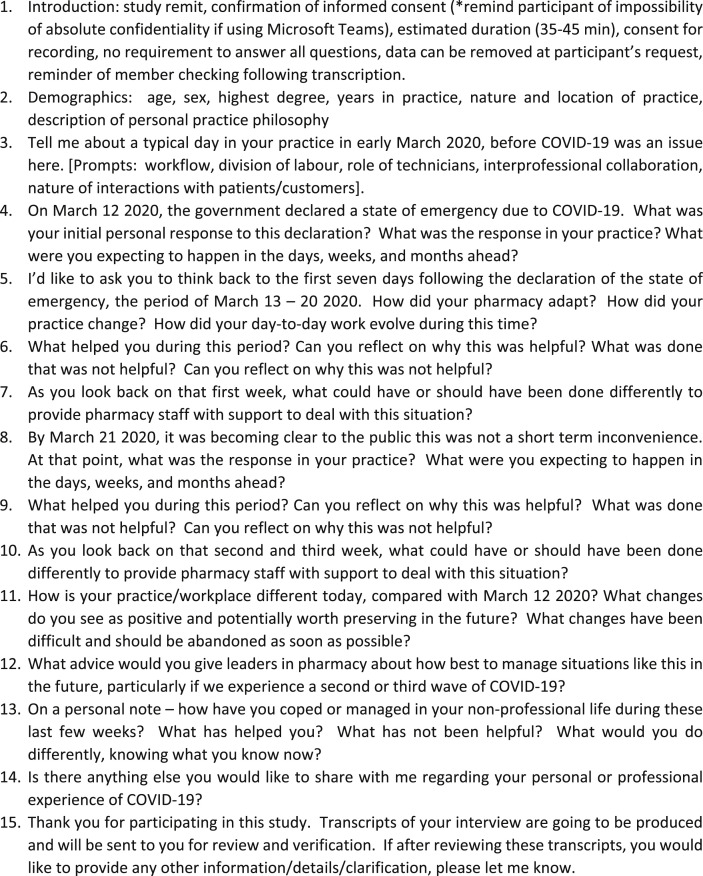
A semi-structured interview protocol was developed and used to guide data gathering. In an effort to expedite data collection to capture real-time experiences, no pilot testing of the protocol was undertaken, and data collection began immediately upon expedited approval of this research by the Research Ethics Board. Initially, questions for the interview protocol were derived from our original 2007 study focused on SARS and the blackout.1 This protocol focused on pragmatic adaptation strategies undertaken by pharmacists during times of civil crisis, and used demarcated time frames during the evolution of the crisis as a tool for stimulating participants to recall and report. Adaptations to the original protocol evolved during the course of the study based on responses from participants and how effectively these addressed research objectives. The final version of the interview protocol is provided at Fig. 1 . The emphasis of this research was on specific personal and professional responses by pharmacists to an acute and evolving crisis. As a result, a pragmatic (rather than theoretically- oriented) approach to protocol development was undertaken emphasizing techniques designed to prompt reflection and enable clear reporting in a chronological manner, corresponding to specific phases of the evolving COVID-10 pandemic. Microsoft Teams provides the capacity to produce verbatim transcripts of recorded “meetings” (interviews); while the quality of these transcripts varied considerably, they provided a starting point for transcription and for those individuals who agreed to meet using this technology, all interviews were recorded and initially transcribed using Teams, but subsequently reviewed and transcripts “cleaned” immediately following the interview by the interviewer to minimize recall bias. In addition, the interviewer maintained field notes during all interviews (by phone or by Teams) to facilitate transcript cleaning and to support data triangulation and confirmation of understanding. In addition, all participants were provided the opportunity to review transcripts of their own interviews to confirm accuracy, intention, and to provide contextualization and clarification.
Fig. 1.
Semi structured interview protocol
1. Introduction: study remit, confirmation of informed consent (*remind participant of impossibility of absolute confidentiality if using Microsoft Teams), estimated duration (35–45 min), consent for recording, no requirement to answer all questions, data can be removed at participant's request, reminder of member checking following transcription.
2. Demographics: age, sex, highest degree, years in practice, nature and location of practice, description of personal practice philosophy
3. Tell me about a typical day in your practice in early March 2020, before COVID-19 was an issue here. [Prompts: workflow, division of labour, role of technicians, interprofessional collaboration, nature of interactions with patients/customers].
4. On March 12,2020, the government declared a state of emergency due to COVID-19. What was your initial personal response to this declaration? What was the response in your practice? What were you expecting to happen in the days, weeks, and months ahead?
5. I'd like to ask you to think back to the first seven days following the declaration of the state of emergency, the period of March 13–20 2020. How did your pharmacy adapt? How did your practice change? How did your day-to-day work evolve during this time?
6. What helped you during this period? Can you reflect on why this was helpful? What was done that was not helpful? Can you reflect on why this was not helpful?
7. As you look back on that first week, what could have or should have been done differently to provide pharmacy staff with support to deal with this situation?
8. By March 21,2020, it was becoming clear to the public this was not a short term inconvenience. At that point, what was the response in your practice? What were you expecting to happen in the days, weeks, and months ahead?
9. What helped you during this period? Can you reflect on why this was helpful? What was done that was not helpful? Can you reflect on why this was not helpful?
10. As you look back on that second and third week, what could have or should have been done differently to provide pharmacy staff with support to deal with this situation?
11. How is your practice/workplace different today, compared with March 12,
2020? What changes do you see as positive and potentially worth preserving in the future? What changes have been difficult and should be abandoned as soon as possible?
12. What advice would you give leaders in pharmacy about how best to manage situations like this in the future, particularly if we experience a second or third wave of COVID-19?
13. On a personal note – how have you coped or managed in your non-professional life during these last few weeks? What has helped you? What has not been helpful? What would you do differently, knowing what you know now?
14. Is there anything else you would like to share with me regarding your personal or professional experience of COVID-19?
15. Thank you for participating in this study. Transcripts of your interview are going to be produced and will be sent to you for review and verification. If after reviewing these transcripts, you would like to provide any other information/details/clarification, please let me know.
The nature of Microsoft Teams as an application means an electronic log of interviews and transcripts was maintained, captured, and stored on a server that was not (and could not be) controlled by the research team. As a result, absolute confidentiality was not possible, though this was deemed “low risk” by the ethics review board. Participants were informed of this; for those who expressed concern regarding confidentiality, a telephone-based interview could be arranged as this was more confidential than using Teams.
Regardless of data collection method (Teams or telephone), all interview data was transcribed, reviewed, cleaned, and ultimately stored and managed through nVivo 11.1. Using an inductive coding and thematic analysis method described by Yin, all transcripts were reviewed by two independent coders who initially categorized and generated themes for analysis.31 This method involves reading and preliminary coding by each coder independently and separately. Each coder produced a preliminary coding structure with specific transcript excerpts as supportive evidence (minimum of 3 excerpts per identified code, in the form of a coding dictionary). As the coding dictionary and structure grew and evolved, each individual coder would identify opportunities for refinements but maintain parallel dictionary/structures as a way of documenting evolution of the analytical process, and for cross-comparison purposes with the other coder. Coders met (virtually, using Microsoft Teams) to discuss their independent analyses and reconcile discrepancies on five separate occasions. After each meeting, a common coding structure and dictionary was then carried forward to the next round of analysis by both coders, who then independently carried on with their analysis as outlined above, before reconvening to establish the next iteration of the common coding structure and dictionary. Through this iterative process, modifications to the interview protocol were also incorporated to address inconsistencies or unclear questions/items. While interviewing was meant to proceed until saturation (the point at which no additional new themes or sub-themes were identified by either coder), the inevitable lag time between interview, transcription, coding, and reconciliation meant that interviews proceeded beyond the point of saturation, and these additional interviews were used for triangulation and confirmation purposes, providing the researchers with an opportunity to test their themes and explanatory model as a primary filter for data analysis, rather than using the transcript data itself to generate themes and build the explanatory model.32 As recommended by Lincoln and Guba, trustworthiness of data interpretation and analysis was built into the method by: a) member checking of transcripts; b) independent coding by two reviewers who met (virtually) to reconcile discrepancies; c) interviewing beyond the point of saturation; and d) using interviews beyond this point of saturation to test and confirm the final themes and the explanatory model generated.33
Findings and discussion
A total of 21 pharmacists from diverse geographical regions representing different practice types participated in this research. A demographic profile of participants is provided at Table 1 . An overarching issue that all pharmacists agreed upon – but which was not the focus of this study – was the almost complete collapse in provision of any paid/remunerated non-dispensing clinical services such as vaccinations or medication reviews during the pandemic. This collapse was mainly due to public health guidance related to social distancing and the impractical logistics associated with continuing to provide services such as these given an unprecedented increase in dispensing workload that was occurring at the same time. The notion that such clinical services and care are “luxuries” that must be abandoned during times of acute crisis warrants further examination but was not the focus of this study.
Table 1.
Demographic profile of participants.
| Participant | Agea | Sexa | Highest Degree | Years in Practice | Nature of Practice | Location of Practice |
|---|---|---|---|---|---|---|
| F48BCS | 48 | Female | BScPharm | 26 | Chain | Suburban |
| M55BGS | 55 | Male | BScPharm | 33 | Grocery | Suburban |
| F40PIR | 40 | Female | Pharm D | 11 | Independent | Rural |
| F49PCU | 49 | Female | Pharm D | 27 | Chain | Urban |
| F31PCU | 31 | Female | Pharm D | 4 | Chain | Urban |
| M66PIU | 66 | Male | Pharm D | 42 | Independent | Urban |
| F40MIS | 40 | Female | MPharm | 14 | Independent | Suburban |
| F31MCU | 31 | Female | MSc | 3 | Chain | Urban |
| M30PCR | 30 | Male | Pharm D | 4 | Chain | Rural |
| M58BGU | 58 | Male | BScPharm | 36 | Grocery | Urban |
| F60BIS | 60 | Female | BScPharm | 38 | Independent | Suburban |
| F27PGR | 27 | Female | Pharm D | 3 | Grocery | Rural |
| F39PCS | 39 | Female | Pharm D | 14 | Chain | Suburban |
| F31PGS | 31 | Female | Pharm D | 5 | Grocery | Suburban |
| F41MIS | 41 | Female | MSc | 15 | Independent | Suburban |
| M28PGU | 28 | Male | Pharm D | 4 | Grocery | Urban |
| M48PGS | 48 | Male | Pharm D | 20 | Grocery | Suburban |
| M49BCR | 49 | Male | BScPharm | 27 | Chain | Rural |
| F52BIU | 52 | Female | BScPharm | 30 | Independent | Urban |
| F32PCU | 32 | Female | Pharm D | 9 | Chain | Urban |
| FaBCS | No response | Female | BScPharm | 38 | Chain | Suburban |
= if declared by participant.
An abundance of data was collected from participants highlighting a diverse array of experiences, adaptive strategies and responses to the COVID crisis, some of which may have been linked to demographic characteristics. Across the participant pool, several common themes with respect to practice resilience emerged:
-
a)
Use of and comfort with technology
-
b)
Early adoption of corporate and professional guidance
-
c)
Workplaces that emphasized task-focus rather than multitasking were more resilient
-
d)
Scheduling methods and practices in the workplace are important for personal resiliency
-
e)
Dedicated specialty staff allowed pharmacists to focus on their work
-
f)
Provision of personal protective equipment and supports was essential
Use of and comfort with technology
An important finding from our 2007 study regarding pharmacy practice in times of civil crisis was the ways in which reliance upon technology actually hindered practice adaptability.1 That study noted that – during the “blackout” of Northeastern North America – pharmacists who had experience with manual dispensing systems and the capacity to do therapeutic assessments without accessing electronic resources (including medication profiles) were better able to cope with the immediate needs of patients. By 2020, this study suggested this finding had been completely upended. A strong and consistent theme across all participants related to the central importance of computer skills and comfort with technology in supporting practice resilience. Central to this finding was the significant increase in prescription volumes (particularly for refill medications) that occurred during the early weeks of quarantine and lockdown. Whether this was driven by consumers’ hoarding behaviours, concerns regarding security of the supply chain, or simply the recognition that getting out to the pharmacy to get medications would become difficult, dispensing workloads increased quickly and substantially. Pharmacy organizations that had previously invested in technology (eg. online or automated telephone-based refill services, or central fill systems) were much better able to manage the surge in workload than those without such systems. Similarly, pharmacy organizations and pharmacists who had comfort and confidence in managing electronic communication reported feeling greater control over workflow and the ability to triage and queue patients more effectively based on priority and need. Using virtual consultation methods in conjunction with appointment bookings helped pharmacists better manage workloads and feel in control of their tasks. In contrast, pharmacy organizations without such technologies were quickly overwhelmed by demand surges, and pharmacists without skills, confidence, or access to such technologies reported feeling heightened occupational stress. The early experience of COVID-19 suggests that rapid evolution of virtual care/clinical consultation models and supports, coupled with technologically enabled digital dispensing supports (particularly around refill medication management) are integral to effectively managing pandemic-related workload surges, and mitigating risk of burnout – provided pharmacists and other staff are trained and confident in effectively using these technologies.
“I'm so glad I'm the kind of person who, you know, likes technology and computers. We were one of the first stores to sign up with the digital renewals and online prescriptions request system and I was the first pharmacist here to get the training so I'm really comfortable with it. Honestly right now with COVID, I don't know what we would have done without it. The volume of work has gone through the roof but being able to manage and control the workflow these technologies is amazing, especially with the email and other options to communicate with the patients.” F49PCU
Early adoption of corporate and professional guidance
All participants in this study described the early weeks of the pandemic as a time of information overload and confusion. The rapid proliferation of every-changing guidance and recommendations, coupled with an overwhelming amount of “fake news” perpetuated on social media meant it was difficult for pharmacists to uphold their traditional commitments to evidence-based scientific practice. Finding trustworthy sources of information was facilitated by computer skills and confidence (see (a) above), but beyond information, facts, or evidence, what pharmacists reported they needed was actual how-to guidance on managing rapidly evolving problems. Most participants in the study reported increasing reliance upon regulatory bodies and professional associations websites and emails as their primary source of information, but simultaneously noted that the way in which these organizations communicated was ambiguous and not focused on actual guidance but simply provision of information or links to other websites. Pharmacists working in large corporate settings noted that corporate employers appeared more pragmatic in the way they communicated with front-line employees, and the clarity, specificity and practical orientation of this guidance was in contrast to (and more helpful in enhancing resilience than) that provided by regulatory bodies. Participants in this study also noted that being “sent” guidance was different than actually reading, understanding, internalizing, and applying it. Once again, the way in which guidance was communicated was seen as pivotally important to the way it was on-boarded by pharmacists: unreasonably theoretical or abstract ideals framed as “principles” which required pharmacists’ interpretation and application to their specific situation/context was seen as less readable and valuable than clear directives telling pharmacists how to behave, what to do, and what to say in specific situations. This style or mode of guidance facilitated early adoption by pharmacy staff and proved helpful in most cases in managing practical workplace issues contributing to occupational stress and burnout.
“I've actually been really impressed with whoever has been writing all these memos and emails about how to handle things during COVID. It's like the person – well they must have been, or maybe still are a pharmacist. It's practical, to the point, and really explains things well, and takes into account real world issues we face all the time. It does wonders for my mental health when I see these memos because I know, phew, they have my back, they understand, they will tell me what I need to know and I can trust it.” F60BIS
Workplaces that emphasized task-focus rather than multitasking were more resilient
There is increasing recognition within the organizational behaviour literature that multitasking – the process of simultaneously undertaking multiple different activities – contributes adversely to cognitive and emotional load,34 and may actually enhance likelihood of errors35 and diminish the quality of outcomes.36 The traditional community pharmacy dispensary has historically been built upon a foundation of multitasking – educating patients, checking prescriptions, answering phone calls, entering inventory etc. The importance of each task may be subsumed in the need to get many tasks done quickly in such an environment, and in such a context, quality is most likely to suffer. An important finding from this study was the connection between resilience and task-focus. Practices that had – pre-COVID – developed workplace routines that provided for physical separation between dispensing and clinical activities, or that used scheduling to provide pharmacists with opportunities to focus on the same activity in isolation for a dedicated period of time – reported greater capacity to manage work surges and challenges associated with the pandemic. More traditional practices that relied upon an undifferentiated (rather than specialized) workforce model reported much more difficulty adapting to the rapid changes induced by pandemic conditions. Further, these practices – even when they recognized the potential value of reorganizing multi-tasking to facilitate task-focus – reported difficulties in doing so given the concomitant surge in workload they were already struggling to deal with. One of the most important findings of this study relates to roles, responsibilities, and opportunities for regulated pharmacy technicians. Ontario, Canada is one of a relatively few jurisdictions that has fully regulated and defined a scope of practice for pharmacy technicians.37 Practices that had hired regulated pharmacy technicians but had not actually established the most appropriate role for them found themselves in a highly advantageous position to pivot rapidly away from multitasking towards a differentiated labour practice model, thereby enhancing resilience and improving workplace conditions for all staff. Further study of this particular finding is important in helping practices develop and implement sustainable workflow models that more fully leverage what regulated pharmacy technicians can do.
“Let's face it you only have so much capacity to give. My last job, the pharmacist was doing everything, running around like a chicken with its head cut off. Here, I get to focus more. We have a system for clinical verification outside the dispensary, so I can sit down at a computer, review, approve and not be disturbed or interrupted so I can really concentrate. It makes me feel so much more confident that I'm doing a good job, doing the right thing, otherwise I would take my work home with me at night and always be worried if I'd made a mistake because I was distracted or interrupted.” F39PCS
Scheduling methods and practices in the workplace are important for personal resiliency
Three scheduling practices in particular were identified by participants as being important for supporting resiliency during times of heightened occupational stress: i) 8 h vs 12 h shifts; ii) established and enforced mandatory ‘break times’ for staff, reinforced by managers; and iii) scheduling of an entire team to work together consistently, rather than scheduling different individuals to work with one another on a seemingly random basis. All three of these practices were identified as practical and important managerial tools to support better quality professional practice as well as enhance personal resiliency. These practices further reinforce the importance of managing the cognitive and emotional load that are characteristic of day-to-day pharmacy practice. Shorter workdays (even if these may not initially be preferred by some individuals for personal scheduling reasons) provide greater opportunities for post-work recharging which can support better quality care. The sheer physical exhaustion associated with longer shifts does not allow for the additional capacity to deal with pandemic related stressors. Similarly, workplaces that actually enforce mandatory break times for staff were described by participants as simply “healthier”. Many participants noted that even workplaces that “allow” for breaks (and importantly – not all workplaces do so) do not necessarily provide the practical or cultural support needed for pharmacists to feel comfortable and confident to actually take scheduled breaks, particularly when in pandemic times workload has increased so significantly. Managerial direction – not simply permission – to take breaks appears to be an important way to address the mixed-messages some pharmacists reported receiving from employers/supervisors. Finally, participants in this research who described workplace scheduling practices focused on entire teams as a unit – rather than individuals – noted that the consistency associated with working with the same individuals over time produced certain efficiencies and communication patterns that increased the practice's capacity to deal with pandemic-related work surges.
“It's not rocket science – human beings can't function at 110% capacity all the time, we burn out. We need to have sustainable shifts, things that allow us a break, a rest so we can recharge a bit. I've worked before with 12, sometimes even 14 hour shifts and that's just nuts. You can't do it more than a day and be safe and stay sane. Right now [with COVID] what everyone needs is the ability to take on more complexity, and if you're already at 110%, you just don't have that to give.” M28PGU
Dedicated specialty staff allowed pharmacists to focus on their work
Throughout the interviews, participants described in great detail the upending of normal workflow and activities caused by the pandemic. Managing crowding in pharmacies – including requiring individuals to take turns and await outside until crowding dissipates, deep cleaning protocols, managing of deliveries and stocking of shelves etc - were described as significantly stressful during the early weeks of the pandemic. Traditionally, pharmacies have often operated as “all hands on board” businesses in which any member of the pharmacy team does whatever needs to be done at any point in time to simply keep things operational; as a result, this means that at times pharmacists are cleaners, security officers and inventory clerks. The dramatic workload increases associated with the pandemic, coupled with the amplified emotional responses demonstrated by many patients made this traditional model difficult to sustain. Pharmacy operations that had (prior to the pandemic) restructured activities to protect pharmacists’ time from these non-clinical activities – or those which were able to do so quickly after the pandemic erupted – were described as being safer, more efficient, and more resilient workplaces. In particular, virtually all participants noted that security-related incidents and issues increased significantly in the early days of the pandemic: patients refusing to queue or wait outside to facilitate social distancing requirements, or individuals demonstrating inappropriate and sometimes violent responses to pharmacists or other staff caused significant stress and concern, particularly when no dedicated security staff were available to manage these issues. Similarly, specific professional cleaning staff with the correct tools and training to ensure effective practices were highlighted as essential during the pandemic: pharmacy organizations that required staff themselves to clean, or used less-than-professional individuals to do so heightened workplace stress considerably, due to concerns of disease transmission. Further, requiring pharmacists to engage in non-clinical work after (or during) exhausting patient-care work was not simply a problem of multitasking (see (d) above); it was physically draining and reduced psychological capacity for resiliency.
“The hardest thing for me right now – it's the customers. They're bananas honestly. I get everyone is concerned and stressed but then they take it out on me. There was a customer, and well, you know about the [salbutamol] and the shortages and then they get freaked out they won't get an inhaler and honestly I start to worry they're going to assault me or the staff. I know some pharmacies have actual real security guards who will intervene and can keep everyone calm and safe and that would be so important right now for me. How can I do my job and think about clinical issues if I'm worried someone is going to punch me in the face? I can't be a police officer and a pharmacist at the same time.” M49BCR
Provision of personal protective equipment and supports was essential
The earliest days of the pandemic were characterized by participants as “chaotic”; beyond issues of guidance, technology, and staffing, all participants in the study highlighted concerns regarding access to correct personal protective equipment (PPE), coronavirus testing, quarantining should coworkers or patients become infected etc. While issues of PPE and testing were society-wide issues at this time,38 most participants in this study resented the notion that they – as front line health care providers during time of pandemic – should be deprived of these most necessary tools of the trade. More than most other factors, lack of ready access to PPE and testing created significant psychological stress that impaired clinical performance and demonstrably changed the nature, time, duration, and extent of contact with patients. Workplaces that found ways to accommodate – either by shifting to virtual care to prevent the need for PPE, or securing appropriate PPE quickly and keeping it replenished, were lauded for both being able to support clinical activities and for demonstrating commitment to the care of their staff. PPE and test access became important psychological proxies, or a litmus test, for organizational commitment to staff, which in turn enhanced individual and organizational resilience and willingness to go the extra mile. Beyond the basic physical safety/security issues associated with PPE and testing, the symbolic importance of these items to pharmacists’ morale and professional commitment were significant.
“It's pretty basic … if I'm worried I'm going to get sick, there's no way I can do my job well, and there's no way I'm going to do the million extra things pharmacists do to help patients. All my energy is being diverted to simply keeping me and my family safe and disease free. That's no way to run a business though and you'd think the [corporation] would figure that out and give us the [PPE] we need and deserve. But if they don't – well then they live with the consequences in terms of what my priorities have to be.” F52BIU
During the course of the interviews, many other ideas and experiences were shared that did not reach the threshold of saturation for reporting in this manuscript; clearly, further longitudinal work in this area is needed to continue to build our understanding of how to prepare pharmacists for the next wave of pandemic.
One of the most important insights from this research has been its practical orientation. Traditionally, the literature has framed “resilience” or psychological attribute residing within the professional him/herself.23 As a result, much of the resilience literature has promoted individual “solutions” such as meditation, mindfulness, or psychotherapy. This study suggests organizations and employers have a much more important role to play in supporting individual resilience than has traditionally been acknowledged in the literature. Seemingly small managerial strategies – for example, moving to 8 h shifts rather than 12 h shifts – that are completely within the control of employers can have meaningful impacts on individual's quality of life and resilience. Across all themes described in this study, a common perspective evolved: the importance of capacity or “bandwidth” within individuals and organizations to manage workload surges induced by the pandemic. Managerial practices related to scheduling, technology, PPE, etc were consistently highlighted by participants as central to whether individuals had the capacity to manage the additional stress and strain brought on by COVID-19. Rather than focus on individual pharmacist's deficiencies with respect to resilience, perhaps a new approach that looks to organization's and employer's responsibilities to provide workplace conditions conducive to resilience is a future line of research. This research was not framed in an open way, and did not seek or avoid discussion related to personal psychology and resilience. Importantly, across all 21 interviews, all participants naturally gravitated to conversations related to organizational, rather than personal psychological issues, despite specific prompts in the interview protocol inviting them to reflect and comment upon personal psychological themes. In enumerating organizational resilience-building tactics and describing how these supported individual, personal efforts, there are perhaps enhanced opportunities for greater conversations between employers and employees - front-line pharmacists and managers – around issues of workplace conditions, cognitive and emotional load, capacity/bandwidth building, and ultimately, resilience.
As the COVID-19 situation has evolved rapidly, researchers around the world have been examining impacts and implications for community pharmacy practice. Aruru et al. have proposed a novel framework for expansion of pharmacists' roles and contributions to evolving pandemic situations, highlighting important operations management issues related to key findings of this study (such as PPE, scheduling, and use of technology to support practice).39 Cadogan and Hughes have recently published work examining community pharmacists’ contributions on the front line during COVID-19, highlighting ways in which primary care services and responsibilities shift towards community pharmacy as a way of reducing pressure on other primary care providers (notably physicians).40 They also note several similar issues related to increased reliance on technology to support pharmacists, and the need to structure workplaces in ways that support provision of clinical care activities rather than traditional operational/business activities. Carioco et al. have written about the unique importance of community pharmacists and their communication skills during the COVID-19 pandemic, highlighting the application of the health belief model. Their work again signposts the importance of workplace design and organizational support for pharmacists providing clinical consultative services.41 While the topic of practice resilience was not explicitly addressed in any of these recently published papers, they do point to the central importance of workplace design and organizational support in providing the tools pharmacists need in order to provide care to patients. In this way, they similarly echo findings of this study which highlight the central importance of managers backing-up pharmacists in ways that demonstrate commitment to personal care and resilience, and to high quality professional practice.
Limitations
While this research has identified important potential future directions for research, there are limitations to consider. The interview protocol used for this study was pragmatic, rather than theoretically derived, and was oriented towards chronological recall and reporting by participants, rather than built upon a pre-existing model or framework. It was neither validated nor pilot tested, in an effort to jump-start data collection for this real-time, real-world study. As a result, it is not connected to an established theoretical framework examining resilience during times of crisis; given the highly unusual circumstances of the COVID-19 situation and the need to expedite research to capture real-time experiences this pragmatic approach had logistical advantages but does mean the findings of this research does not fully connect to extant literature, theory, or models. The recruitment strategy used for this study limits generalizability beyond the study context, particularly to other jurisdictions or pharmacy practice models. While the data collected was both thick and rich, it is based upon the experiences of an unrepresentative group of pharmacists in one geographical context. This study applied several core principles described by Lincoln and Guba to enhance trustworthiness of analysis and interpretation33; however, additional principles (e.g. multiple interviews at different times with individual participants, use of other data gathering techniques for triangulation etc) were not possible given time, resource, and logistics constraints. Many more individual experiences were described by participants during this research, but never reached the saturation threshold to be framed as “themes” for this study; further exploration involving a larger number of research participants may be useful to help determine how best to understand and frame these experiences so they are not lost. Further work in better understanding the intersection of personal psychology and organizational/workplace practices is needed to help the profession of pharmacy equip itself for the next wave of pandemic – and other crises that may occur in the future.
Lincoln and Guba's recommendations for establishing credibility and trustworthiness were used to help guide data collection, analysis, and reporting.33 However, it was not possible to follow all their recommendations, and as a result this may limit the generalizability of the study to other contexts. While certain strategies described in the Methods section above (e.g. use of dual independent coders, thick description, and data collection beyond saturation) enhance credibility and dependability of this research, other techniques were simply not feasible or not used (e.g. prolonged engagement, persistent observation, triangulation, or inquiry audits). As described by Lincoln and Guba, the more of these techniques that are used, the greater the confidence that is generated in the robustness and trustworthiness of the research. Our inability to use more than four of these techniques was due to our desire to undertake rapid-response, pragmatic real-world research of an evolving phenomenon in real time; as a result, generalizability and credibility may not be as strong as possible had additional techniques been incorporated into the study design.
Conclusions
Whether multiple waves of COVID-19 infections persist for months or years to come, or whether a new pandemic, infection, or civic crisis erupts, there will be sharp, acute emergencies that will continue to fundamentally disrupt pharmacy practice in the years to come. Ensuring resilience of the workplace and the workforce is essential to ensure continuing provision of service and care. This study has highlighted important opportunities for workplaces to contribute meaningfully to individual/personal resilience through a diverse array of managerial practices. Conceptualizing resilience as a shared responsibility between workers and management, rather than as an individual deficit, is essential, particularly during times of pandemic and emergency.
CRediT authorship contribution statement
Zubin Austin: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Validation, Writing - original draft. Paul Gregory: Data curation, Formal analysis, Investigation, Project administration, Software, Writing - review & editing.
Acknowledgements
Funding for this study was provided through an unrestricted educational grant from the Ontario College of Pharmacists, the regulatory body for pharmacy in Ontario, Canada.
References
- 1.Austin Z., Martin J.C., Gregory P.A. Pharmacy practice in times of civil crisis: the experience of SARS and the blackout in Ontario, Canada. Res Soc Adm Pharm. 2007;3(3):320–335. doi: 10.1016/j.sapharm.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruan S. Likelihood of survival of coronavirus disease 2019. Lancet. 2020 doi: 10.1016/S1473-3099(20)30257-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Director-general media briefing. March 11 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Accessed May 12 2020 at.
- 4.Gates B. Responding to COVID-19 – a once in a century pandemic? N Engl J Med. 2020;382:1677–1679. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 5.Ives J., Greenfield S., Parry J. Healthcare workers' attitudes to working during pandemic influenza: a qualitative study. BMC Publ Health. 2009;9 doi: 10.1186/1471-2458-9-56. Article 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) J Hosp Infect. 2020;105(1):100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. J Am Med Assoc. 2020;323(15):1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 8.Taubenberger J.K., Morens D.M. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12(1):15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cox N.J., Tamblyn S.E., Tam T. Influenza pandemic planning. Vaccine. 2003;21(16):1801–1803. doi: 10.1016/s0264-410x(03)00076-8. [DOI] [PubMed] [Google Scholar]
- 10.Tam T., Sciberras J., Tamblyn S.E., King A., Robert Y. The Canadian Pandemic Influenza Plan: an evolution to the approach for national communicable disease emergencies. Int Congr Ser. 2004;1263:239–242. doi: 10.1016/j.ics.2004.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shearer F.M., Moss R., McVernon J., Ross J.V., McCaw J.M. Infectious disease pandemic planning and response: incorporating decision analysis. PLoS Med. 2020;17(1) doi: 10.1371/journal.pmed.1003018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzgerald T.J., Kang Y., Bridges C.B. Integrating pharmacies into public health program planning for pandemic influenza vaccine response. Vaccine. 2016;34(46):5643–5648. doi: 10.1016/j.vaccine.2016.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Traynor K. Pharmacists matter in pandemic response. Am J Health Syst Pharm. 2008;65(19):1792–1793. doi: 10.2146/news080080. [DOI] [PubMed] [Google Scholar]
- 14.McCann C., Beddoe E., McCormick K. Resilience in the health professions: a review of recent literature. Int J Wellbeing. 2013;3(1):60–81. [Google Scholar]
- 15.Robertson H., Elliott A., Burton C. Resilience of primary health care professionals: a systematic review. Br J Gen Pract. 2016;66(647):e423–e433. doi: 10.3399/bjgp16X685261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rakesh G., Pier K., Costales T. A call for action: cultivating resilience in healthcare providers. Am J Psychiatr. 2017 doi: 10.1176/appi.ajp-rj.2017.120402. [DOI] [Google Scholar]
- 17.O'Dowd E., O'Connor P., Lydon S. Stress, coping, and psychological resilience among physicians. BMC Health Serv Res. 2018;18 doi: 10.1186/s12913-018-3541-8. Article 730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee Y., Lee J., Kim J., Shin I., Yoon J., Kim S. A comparative study of burnout, stress, and resilience among emotional workers. Psychiatry Investig. 2019;16(9):686–694. doi: 10.30773/pi.2019.07.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Austin Z. Cultivating resilience in the health professions. J Am Pharmaceut Assoc. 2020;26(2):41–53. [Google Scholar]
- 20.Iflaifel M., Lim R.H., Ryan K., Crowley C. Resilient health care: a systematic review of conceptualisations, study methods, and factors that develop resilience. BMC Health Serv Res. 2020;20 doi: 10.1186/s12913-020-05208-3. Article 324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kahn W.A. Brunner-Routledge; Hove: 2004. Holding Fast: The Struggle to Create Resilient, Caregiving Organizations. [Google Scholar]
- 22.Glasberg A.L., Eriksson S., Norberg A. Burnout and stress of conscience among healthcare personnel. J Adv Nurs. 2007;57(4):392–403. doi: 10.1111/j.1365-2648.2007.04111.x. [DOI] [PubMed] [Google Scholar]
- 23.Lengnick-Hall C., Beck T., Lengnick-Hall M. Developing a capacity for organizational resilience through strategic human resource management. Hum Resour Manag Rev. 2011;21:243–255. [Google Scholar]
- 24.Liu S., Luo P., Tang M. Providing pharmacy services during the coronavirus pandemic. Int J Clin Pharm. 2020;42(2):299–304. doi: 10.1007/s11096-020-01017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.International Pharmacy Federation (FIP) Covid-19 information hub. https://www.fip.org/coronavirus Accessed May 12 2020 at.
- 26.Canadian Pharmacists’ Association Pandemic influenza: a pharmacist's guide to pandemic preparedness. 2009. http://www.pharmacists.ca/cpha-ca/assets/File/education-practice-resources/PandemicGuideEN.pdf Accessed May 12 2020 at:
- 27.Royal Pharmaceutical Society of Great Britain Guidance on ethical, professional decision-making in the COVID-19 pandemic. 2020. https://www.rpharms.com/about-us/news/details/Guidance-on-ethical-professional-decision-making-in-the-COVID-19-pandemic Accessed May 12 2020 at.
- 28.American Pharmacists’ Association A pharmacist's guide to pandemic preparedness. 2007. https://cdn.ymaws.com/www.aparx.org/resource/resmgr/imported/Pandemic_Preparedness_Guide.pdf Accessed May 12 2020 at.
- 29.American Pharmacists’ Association APhA issues preparedness and prevention guidance during coronavirus pandemic. https://www.pharmacist.com/press-release/apha-issues-preparedness-and-prevention-guidance-during-coronavirus-pandemic Accessed May 12 2020 at.
- 30.Novick G. Is there a bias against telephone interviews in qualitative research? Res Nurs Health. 2008;31:391–398. doi: 10.1002/nur.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yin R. second ed. Guildford Press; London: 2007. Qualitative Research from Start to Finish. [Google Scholar]
- 32.Saunders B., Sim J., Kingstone T. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quantity. 2018;52:1893–1907. doi: 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lincoln Y., Guba E. Sage Publications; Newbury Park CA: 1985. Naturalistic Inquiry. [Google Scholar]
- 34.Gopher D., Armony L., Greenspan Y. Switching tasks and attention policies. J Exp Psychol. 2000;129:208–229. doi: 10.1037//0096-3445.129.3.308. [DOI] [PubMed] [Google Scholar]
- 35.Monsell S., Yeung N., Azuma R. Reconfiguration of task-set: is it easier to switch to the weaker task? Psychol Res. 2000;63:250–264. doi: 10.1007/s004269900005. [DOI] [PubMed] [Google Scholar]
- 36.Raban M., Walter S., Douglas H., Strumpman D., Mackenzie J., Westbrook J. Measuring the relationship between interruptions, multitasking and prescribing errors in an emergency department. BMJ Open. 2015;5(10) doi: 10.1136/bmjopen-2015-009076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gregory P., Austin Z. Professional identity formation: the experience of regulated pharmacy technicians in Ontario. Can Pharm J. 2019;153(1):46–51. doi: 10.1177/1715163519882466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herron J. Personal protective equipment and COVID-19 – a risk to healthcare staff? Br J Oral Maxillofac Surg. 2020 doi: 10.1016/j.bjoms.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aruru M., Truong H., Clark S. Pharmacy emergency preparedness and responses (PEPR): a proposed framework for expanding pharmacy professionals' roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.002. https://reader.elsevier.com/reader/sd/pii/S1551741120303235?token=4AFA9192CC281CECAD890B9F576B857789144EC6AFF7D37CFCE2FD4ACE254C2AC1DABA76E9C2BB413BD713F911B06D90 Accessed May 25 2020 at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cadogan C., Hughes C. On the frontline against COVID-19: community pharmacists' contribution during a public health crisis. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.015. https://reader.elsevier.com/reader/sd/pii/S1551741120302928?token=6F763476E76578C9AD6B12EF36FFBB0C6971CB109D4F3A25F2681755CE8B24D93A92D6284C4B746074D63AE2C18F8128 Accessed May 25 2020 at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carico R., Sheppard J., Borden Thomas C. Community pharmacists and communication in the time of COVID-19: applying the health belief model. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.017. https://reader.elsevier.com/reader/sd/pii/S155174112030293X?token=A83A95F2288A560708D69AE7BD923D97580B96A8B0E7BDE7BFAA2B46F3F725D2FC5B07E514B322E432FD01EE20E77203 Accessed on May 25 2020 at. [DOI] [PMC free article] [PubMed] [Google Scholar]