To the Editor
1. Introduction
Epilepsy is a chronic neurological disorder that causes recurrent, unprovoked seizures. It is known that 20–30% of patients with epilepsy experience symptoms of depression [1]. Compared with healthy people, patients with epilepsy have a 40–50% higher suicide rate [2].
Coronavirus disease 2019 (COVID-19) initially occurred in Wuhan, China in late 2019 before its global outbreak [3]. It is a novel infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The COVID-19 crisis has been stressful for people across the world, with everyone having to adapt to the changes involved.
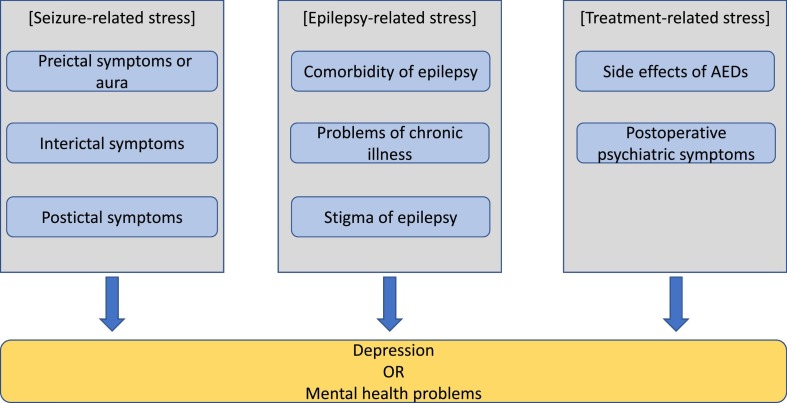
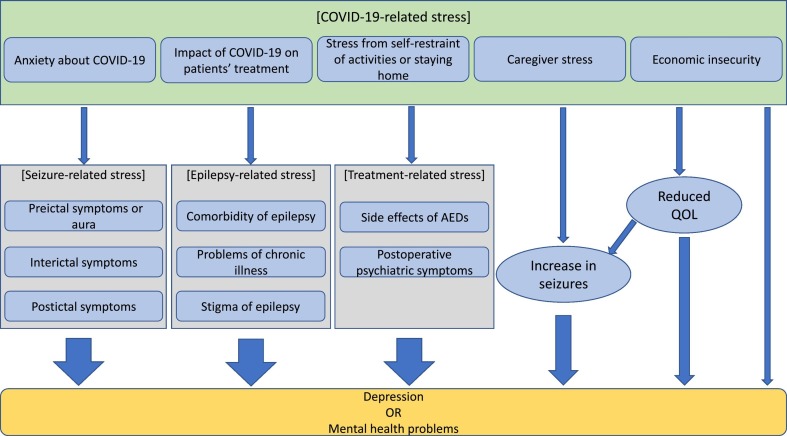
It is important for clinicians to consider the psychological impact of this crisis while treating patients with epilepsy. Firstly, we have discussed how epilepsy causes mental stress in patients (Fig. 1 ). We have also considered how the COVID-19 crisis affects the mental health of patients with epilepsy (Fig. 2 ).
Fig. 1.
Impact of each factor on the mental health of patients with epilepsy. AEDs: antiepileptic drugs.
Fig. 2.
Effects of COVID-19-related stress on each factor and the direct impact on the mental health of patients. AEDs: antiepileptic drugs, COVID-19: coronavirus disease 2019, QOL: quality of life.
2. Mental changes associated with seizures
Preictal psychiatric symptoms often occur about a few days or hours before the seizure and end with the onset of the seizure [4]. According to a previous report, about one-third of the patients with partial seizures experience premonitory symptoms, usually before secondarily generalized tonic–clonic seizures [5]. Therefore, in addition to the information on seizures, physicians treating epilepsy need to be aware of the patient's original mental state and premorbid personality. The patient also needs to be evaluated for any changes.
Psychiatric symptoms may occur as a symptom of the seizure itself and are known to be more common in temporal lobe epilepsy [4]. As these are seizure symptoms that occur during the duration of the seizure, the quality of life of the patient may be affected because of the fear of the onset of the mood symptoms.
The psychiatric symptoms that accompany the end of a seizure are known as postictal psychiatric disturbances or postictal mood disorders and commonly occur after frequent seizures and generalized seizures. There is typically an asymptomatic period spanning hours or days after the seizure, followed by a rapid hallucinatory delirium along with aggression and exaggeration [4]. Basically, it improves within a week with self-remitting. In contrast, postictal depression is less recognized in psychiatric practice as compared with postictal psychoses. However, these are frequently reported by patients and relatives [4]. Its symptoms, including dysphoria and crying bout, are characteristics of depression complicated by epilepsy. In addition, it is believed that as many as 45% of the total population complains of anxiety after a seizure, even if it might not reach the stage of depression [4].
3. Mental stress associated with epilepsy as a neurological chronic disorder
A certain percentage of people with epilepsy are known to have complications with mood disorders and psychiatric symptoms [1]. This is attributed to the possibility that organic lesions in epilepsy may also cause depression and psychiatric symptoms. The impact of comorbid depression on the quality of life of patients is thought to be comparable with the impact of severity and frequency of seizures.
In addition, having epilepsy can lead to a new onset of depression. Apart from the stress associated with chronic illnesses in general, patients with epilepsy experience a great deal of anxiety and tension about the onset of seizures and a sense of helplessness of being unable to control them on their own. Seizures also have a significant impact on normal day-to-day activities, such as bathing and exercise, as well as important aspects of social life, such as working, driving, and marriage. These effects of seizures on daily life often constrain patients with epilepsy to limit their day-to-day activities, leading to depressive symptoms.
The social stigma associated with epilepsy also majorly impacts the mental state of patients with epilepsy in addition to their personal problems. The stigma of having epilepsy can lead to depression in patients [6]. Thus, it is necessary for the society as a whole to create a better environment for patients to live in, through conducting activities to increase awareness and being sensitive to the feelings of people around them [7]. While there may be restrictions on driving and working, patients with epilepsy should not be subjected to social discrimination on the basis of their condition.
4. Mental changes caused by treatments for epilepsy
Since some antiepileptic drugs (AEDs) can affect the patient's mental state and mood, the possibility of adverse effects from AEDs should be considered when a patient presents with symptoms of a mood disorder [8]. Typical drugs that cause such adverse effects are ethosuximide, clonazepam, zonisamide, topiramate, and levetiracetam. Most of the adverse effects caused by these AEDs improve with discontinuation of the drugs. Physicians should pay close attention to patients who report adverse effects associated with AEDs, as some reports have stated an association between suicide and adverse effects of AEDs [9].
It is known that new psychiatric symptoms can occur after epilepsy surgery. The incidence of postoperative depression is 4–18%, often occurring between 3 and 12 months postoperatively and lasting for several months [10]. Therefore, clinicians need to follow-up with patients within a year of epilepsy surgery, paying attention to the presence of psychiatric symptoms.
5. Impact of COVID-19 on the mental health of patients with epilepsy
5.1. Anxiety about COVID-19
Although information about COVID-19 is regularly updated, no specific treatment has been identified yet. Vaccines are also being researched and developed, but it will take some time before they can be put to practical use. For these reasons, the existence of COVID-19 has been a threat to humanity for several months. Although the risk of COVID-19 in patients with epilepsy is not thought to be higher than in healthy people, psychological stress from COVID-19 has been reported to be greater in the former [11]. This mental stress might increase the frequency of seizures in patients with epilepsy. The increase of seizures can itself be a cause of depression in patients. In addition, more seizures may increase the likelihood of seizure-related depression, which is described in Section 2.
5.2. Stress from self-restraint of activities or staying home
In order to prevent the spread of COVID-19, several countries and regions are taking measures such as social distancing and are refraining from certain activities [12]. The stress on people from having to maintain a social distance and not being able to engage in free activities is pronounced. It is believed that a majority of the people have depression due to this stress [13]. People with epilepsy may be affected not only by this stress but also by disruptions in lifestyle and changes in medication compliance from staying at home, which may influence seizure frequency.
5.3. Impact of COVID-19 on patients' treatment
Patients with epilepsy may need their doctors to prescribe AEDs on a regular schedule; they may be concerned about the access to medication or may fear about being exposed to the virus by going to a healthcare provider. Patients from regions where telemedicine services are not available could face a shortage of AEDs [14,15]. In addition, some patients on a diet therapy may find it difficult to obtain low-carb foods due to the hoarding behavior of people, which may lead to increased seizures and stress [16].
5.4. Economic insecurity
Because of the need to maintain a social distance, remote working has been recommended worldwide. In addition, restaurants and recreational facilities have been restricted from operating. Thus, the impact of COVID-19 on economies around the world has been significant, leading to huge job losses [13]. Concerns about salary and job are also reasons for depression in the general population [17]. These concerns can also lead to a decline in the quality of life and result in secondary symptoms of depression.
5.5. Consideration for caregiver stress
In the case of patients with epilepsy who require care, the stress of the caregiver should also be considered. It has been reported that caregiver stress and anxiety can affect the quality of life of the patient [18], and hence, attempts to reduce caregiver stress and anxiety can help prevent a decline in the quality of life of the patients.
6. Conclusion
This article discusses the mental health of people with epilepsy and the associated impact of COVID-19. Even prior to the COVID-19 crisis, patients with epilepsy were prone to depression for a variety of reasons. Despite the introduction of telemedicine, there is a need to pay more attention to the psychiatric symptoms in patients than prior to the COVID-19 crisis.
Financial disclosures
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
Acknowledgments
None.
References
- 1.Fiest K.M., Dykeman J., Patten S.B., Wiebe S., Kaplan G.G., Maxwell C.J. Depression in epilepsy: a systematic review and meta-analysis. Neurology. 2013;80:590–599. doi: 10.1212/WNL.0b013e31827b1ae0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell G.S., Sander J.W. Suicide and epilepsy. Curr Opin Neurol. 2009;22:174–178. doi: 10.1097/WCO.0b013e328328f8c3. [DOI] [PubMed] [Google Scholar]
- 3.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mula M., Monaco F. Ictal and peri-ictal psychopathology. Behav Neurol. 2011;24:21–25. doi: 10.3233/BEN-2011-0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaitatzis A., Trimble M.R., Sander J.W. The psychiatric comorbidity of epilepsy. Acta Neurol Scand. 2004;110:207–220. doi: 10.1111/j.1600-0404.2004.00324.x. [DOI] [PubMed] [Google Scholar]
- 6.Yeni K., Tulek Z., Simsek OF, Bebek N. Relationships between knowledge, attitudes, stigma, anxiety and depression, and quality of life in epilepsy: a structural equation modeling. Epilepsy Behav. 2018;85:212–217. doi: 10.1016/j.yebeh.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Tedrus G., Pereira R.B., Zoppi M. Epilepsy, stigma, and family. Epilepsy Behav. 2018;78:265–268. doi: 10.1016/j.yebeh.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Perucca P., Mula M. Antiepileptic drug effects on mood and behavior: molecular targets. Epilepsy Behav. 2013;26:440–449. doi: 10.1016/j.yebeh.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 9.Mula M., Kanner A.M., Schmitz B., Schachter S. Antiepileptic drugs and suicidality: an expert consensus statement from the Task Force on Therapeutic Strategies of the ILAE Commission on Neuropsychobiology. Epilepsia. 2013;54:199–203. doi: 10.1111/j.1528-1167.2012.03688.x. [DOI] [PubMed] [Google Scholar]
- 10.Cleary R.A., Baxendale S.A., Thompson P.J., Foong J. Predicting and preventing psychopathology following temporal lobe epilepsy surgery. Epilepsy Behav. 2013;26:322–334. doi: 10.1016/j.yebeh.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 11.Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E. Severe psychological distress among epilepsy patients during the COVID-19 outbreak in southwest China. Epilepsia. 2020 doi: 10.1111/epi.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shader R.I. COVID-19 and depression. Clin Ther. 2020 doi: 10.1016/j.clinthera.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leenen L.A.M., Wijnen B.F.M., de Kinderen R.J.A., van Heugten C.M., Evers S., Majoie M. Are people with epilepsy using eHealth-tools? Epilepsy Behav. 2016;64:268–272. doi: 10.1016/j.yebeh.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Brigo F., Bonavita S., Leocani L., Tedeschi G., Lavorgna L. Telemedicine and the challenge of epilepsy management at the time of COVID-19 pandemic. Epilepsy Behav. 2020 doi: 10.1016/j.yebeh.2020.107164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.KetoDiet 10 tips to help you stay low-carb during COVID-19 isolation. 2020. https://ketodietapp.com/Blog/lchf/10-tips-to-help-you-stay-low-carb-during-covid-19-isolation
- 17.Zhu S., Tse S., Goodyear-Smith F., Yuen W., Wong P.W. Health-related behaviours and mental health in Hong Kong employees. Occup Med (Lond) 2017;67:26–32. doi: 10.1093/occmed/kqw137. [DOI] [PubMed] [Google Scholar]
- 18.Zhu X.R., Zhao T., Gu H., Gao Y.J., Wang N., Zhao P. High risk of anxiety and depression in caregivers of adult patients with epilepsy and its negative impact on patients' quality of life. Epilepsy Behav. 2019;90:132–136. doi: 10.1016/j.yebeh.2018.11.015. [DOI] [PubMed] [Google Scholar]