Abstract
Cuff erosion at the bladder neck of an implanted artificial urinary sphincter (AUS) needs complete explantation of the device. The subsequent scar tissues predispose to repeated cuff erosion, when another AUS is implanted with the cuff at a similar location. We describe a paraplegic patient with exstrophy-epispadias complex that suffered from an AUS cuff erosion at the bladder neck. We use a novel perineal-retropubic route for cuff placement, with preparation similar to a retropubic male sling. At 12 years follow-up the AUS is still functional and the patient continent.
Keywords: Cuff erosion, Artificial urinary sphincter, Perineal retropubic approach, Salvage AMS 800
Introduction
The artificial urinary sphincter (AUS) with a bladder neck cuff is the treatment of choice for neurogenic urinary incontinence. Patients with exstrophy-epispadias complex (EEC) and urinary incontinence may also be treated with an AUS.1 A real dilemma arises when a paraplegic patient with EEC and an AUS suffers from cuff erosion at the bladder outlet. We describe a novel alternative of cuff placement via a perineal-retropubic route to avoid the fibrosis and scar tissues at the bladder outlet. Three years after removal of the AUS and bladder outlet reconstruction, a new AUS implantation followed, with the cuff in a diagonal position across the membranous urethra (Fig. 1). At 12 years follow-up the AUS is still functional and the patient fully continent. A Brindley stimulator accomplishes residual-free voiding and regular defecation.2
Fig. 1.

Image of a lateral voiding cystourethrography of the patient after AUS removal. a
) Blue arrow indicates the classical route for AUS cuff placement at the bladder neck.
b) Yellow arrow indicates perineal-retropubic route for AUS cuff placement diagonal across the membranous urethra. Appreciate the difference of a) and b) in the possible strain onto the bladder neck/
bladder outlet and membranous urethra.
Note the sacral nerve electrodes of the Brindley stimulator. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Case Presentation
In the year 2000, a 32-year-old male paraplegic patient presented to the neurourology outpatient clinic with his main problem of neurogenic urinary incontinence. Furthermore, he has an uncorrected proximal epispadias with diastasis of the symphysis. The bladder neck is incompetent. A Brindley procedure followed with rhizotomy of the dorsal sacral roots, bilateral electrodes at S2, 3, 4, and a stimulator implant for sacral anterior-root stimulation. Use of the Brindley stimulator enabled micturition with complete bladder emptying, defecation, and erections. The proximal epispadias was surgically corrected (Fig. 2). In 2001, an AUS implantation with a 9cm bladder neck cuff dramatically improved his continence. The patient wished for total continence that resulted in downsizing of the cuff to 8cm in 2003. In 2005, the cuff eroded into the left lateral bladder neck and urethra, which necessitated AUS explantation. At this stage, further options included incontinent or continent urinary diversions that the patient did not want. In 2008, another AUS implant followed using a combined suprapubic and perineal approach (Fig. 2). Dissection followed a path lateral to the urethral bulb and wide from the bladder neck alongside the inferior pubic rami, staying away from the reconstructed bladder neck and urethra. Placing a measuring tape all around enabled railroading of an 11cm cuff around the anterior bladder wall above, and the urethral bulb below. A 61–70 cmH2O pressure-regulating balloon filled with 25 ml isosmotic radio contrast solution was put intraperitoneal. The pump was placed deep into the right hemiscrotum. Post-surgery bladder drainage was by transurethral catheter for 2 weeks. As the patient was still incontinent, AUS activation followed at 8 weeks post-surgery. At 12 years follow-up, the patient is still fully continent and voids by Brindley stimulator. His original Brindley stimulator still functions 20 years after implantation.
Fig. 2.
Overview of surgery:
A). Operative result after proximal epispadias repair.
B) Measuring tape on the right side (of the patient) lateral to the bladder neck and urethra alongside the inferior pubic rami. Note the perineal and suprapubic incisions. C and D) Measuring tape with both ends in the suprapubic wound, measuring 11cm circumference.
Discussion
This patient was born with EEC with proximal epispadias and diastasis of the symphysis. His bladder neck was competent, but he was not completely continent. As a young man, he suffered from spinal trauma and became a complete paraplegic below D7, with the development of neurogenic bladder and bowel dysfunction. He was incontinent of urine and needed to do clean intermittent self-catheterization (CISC) to empty bladder residual. At first, the Brindley procedure was done with good success that enabled complete voiding. The epispadias repair then followed. His bladder capacity was ~500ml, and to gain continence an AUS was implanted with a bladder neck cuff. After downsizing of the cuff, it eventually eroded through the bladder neck and the urethra on the left side. In exstrophy patients, bladder neck reconstruction or bladder neck closure with continent diversion is treatment of choice.3 This patient had proximal epispadias right up to the level of the wide bladder neck. The use of an AUS after proximal epispadias repair is controversial. Even after AUS cuff erosion, our patient was determined to try another AUS once more. Repeat cuff placements in the same position are problematic.4 We decided on a different approach similar to the male remeex system.5 Cuff placement via suprapubic and perineal incisions, staying wide of the bladder neck alongside the inferior pubic rami around the urethral bulb was a viable alternative. (Fig. 1, Fig. 2). Fig. 3 shows the difference in cuff location.
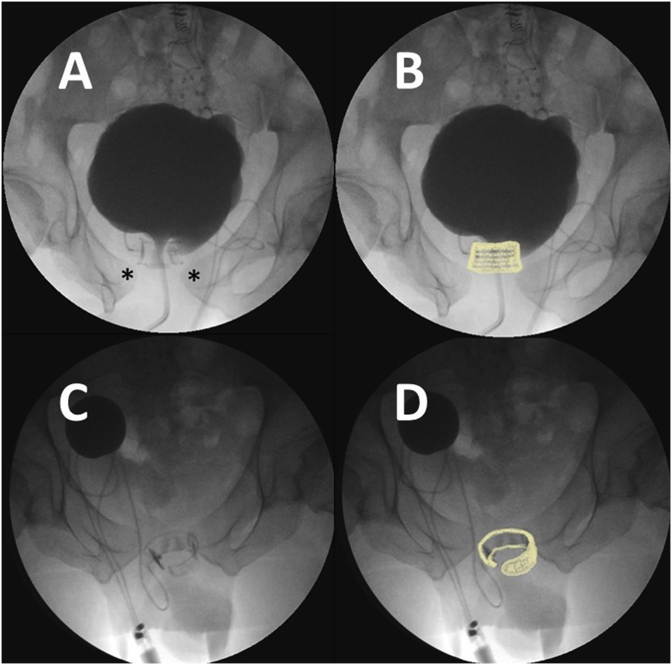
Fig. 3.
Comparison of cuff position at bladder neck (A, B), and after perineal-retropubic placement (C, D) on anterior-posterior X-ray view. Cuff highlighted in light yellow in B and D.
A and B).
Asterisks show diastasis of pubic symphysis in exstrophy-epispadias complex. The cuff is located around the bladder neck. It eroded on the left hand side into the bladder neck and reconstructed urethra.
C and D) The cuff is diagonally across the membranous urethra around the anterior bladder outlet above and the urethral bulb below.
Note the sacral nerve electrodes of the Brindley stimulator in A through D.
Conclusion
The perineal-retropubic cuff placement is a novel alternative in comparison to the bulbar or bladder neck locations. In this complex case of a young paraplegic patient after proximal epispadias repair with diastasis of the pubic symphysis and previous AUS cuff erosion at the bladder neck, this technique resulted in complete urinary continence with a follow-up of 12 years.
Declarations of competing interest
PR: Speaker for Boston Scientific.
MB, AR, AO, HM: no conflicts of interest.
JS: Speaker for Boston Scientific.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient data anonymized and patient's consent obtained for publication.
Acknowledgements
A great “Thank You” to all staff members of the Neurourology Team in the Department of Urology at the Tirol Kliniken, Innsbruck, Austria, dedicated to neurourology patients.
References
- 1.Light J.K., Scott F.B. Treatment of the epispadias-exstrophy complex with the AS792 artificial urinary sphincter. J Urol. 1983;129(4):738–740. doi: 10.1016/s0022-5347(17)52336-8. [DOI] [PubMed] [Google Scholar]
- 2.Brindley G.S., Rushton D.N. Long-term follow-up of patients with sacral anterior root stimulator implants. Paraplegia. 1990;28(8):469–475. doi: 10.1038/sc.1990.63. [DOI] [PubMed] [Google Scholar]
- 3.Snodgrass W., Barber T. Comparison of bladder outlet procedures without augmentation in children with neurogenic incontinence. J Urol. 2010;184(4 Suppl):1775–1780. doi: 10.1016/j.juro.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 4.Motley R.C., Barrett D.M. Artificial urinary sphincter cuff erosion. Experience with reimplantation in 38 patients. Urology. 1990;35(3):215–218. doi: 10.1016/0090-4295(90)80034-k. [DOI] [PubMed] [Google Scholar]
- 5.Sousa-Escandon A., Cabrera J., Mantovani F. Adjustable suburethral sling (male remeex system) in the treatment of male stress urinary incontinence: a multicentric European study. Eur Urol. 2007;52(5):1473–1479. doi: 10.1016/j.eururo.2007.05.017. [DOI] [PubMed] [Google Scholar]