Abstract
The COVID-19 (Coronavirus disease 2019) pandemic has caused an unprecedented strain on healthcare systems across the globe. Apart from being a major hurdle to delivery of basic healthcare services, this may be associated with potential harm for cancer patients. Usually being immunocompromised, cancer patients are at a higher risk of contracting the disease and with hospitals being a potential source of the infection, an urgent need to reorganise the structure of delivery of cancer care is essential. Cancer departments must balance patient care whilst also minimising transmission among patients and healthcare professionals. The Oxford Sarcoma Service was re-structured based on the guidelines issued by the National Health Service (NHS) and the British Orthopaedic Oncology Society (BOOS) to deliver unhindered care to patients. Prioritising patients who needed urgent surgery, weighing the risk-benefit ratio while delivering adjuvant treatments and conducting regular virtual multi-disciplinary team (MDT) meetings combined with personal protection equipment (PPE) usage by all involved healthcare workers were salient features in terms of ensuring the delivery of effective care during the COVID-19 pandemic. Our new model of modus operandi during this global crisis was effective in delivering high standard of care to patients and might serve as a guide to similar units managing bone and soft tissue tumours.
Keywords: COVID-19, Cancer care delivery, Bone tumour, Sarcoma, Virtual MDT
Abbreviations: NHS, National Health Service; BOOS, British Orthopaedic Oncology Society; PPE, Personal Protective Equipment; MDT, Multi-disciplinary team; GP, General Practitioner
1. Introduction
The COVID-19 virus which originated in Wuhan, China in December 2019, rapidly progressed to a global pandemic by March 2020 and caused a massive shock to all healthcare systems around the world.1 Elective surgeries and non-urgent patient appointments were cancelled to mitigate disease transmission but emergency services including trauma and essential services like cancer needed to continue to prevent disease progression and reduce mortality.2,3 Healthcare professionals managing these patients are also at higher risk of contracting the disease as hospitals are a potential source of infection. It follows therefore that, an adequate balance is essential where patient care is delivered appropriately, healthcare workers are protected and most importantly the healthcare system is not overwhelmed.4,5 On March 23rd, 2020 the National Health Service (NHS) issued guidelines for managing cancer patients who needed acute care.6 Based on these guidelines and the guidelines issued by the British Orthopaedic Oncology Society (BOOS),7 the Oxford sarcoma service re-structured its day-to-day functioning which was aimed at delivering treatment to patients who would benefit most. We largely moved to virtual platforms with for MDT meetings and clinics. The Oxford Bone and Soft Tissue Tumour Service - at the Nuffield Orthopaedic Centre is one of five nationally approved centres in England) for the treatment of rare primary bone tumours and sarcomas – is a tertiary referral centre for catering to nearly 2500 patients each year. Reorganisation of the main arms of the service – triages, MDTs, clinics, surgery, adjuvant therapies - was vital to deliver effective cancer care continuously throughout the peak of the pandemic in the UK without overwhelming the local healthcare system. In this article, we discuss the organisational changes we undertook in the service to manage patients during the COVID-19 pandemic. (see Table 1)
Table 1.
Key changes implemented at the Oxford bone tumour and soft tissue sarcoma service during the COVID-19 pandemic.
|
|
|
|
|
|
MDT: Multidisciplinary team.
2. Patient referral triages
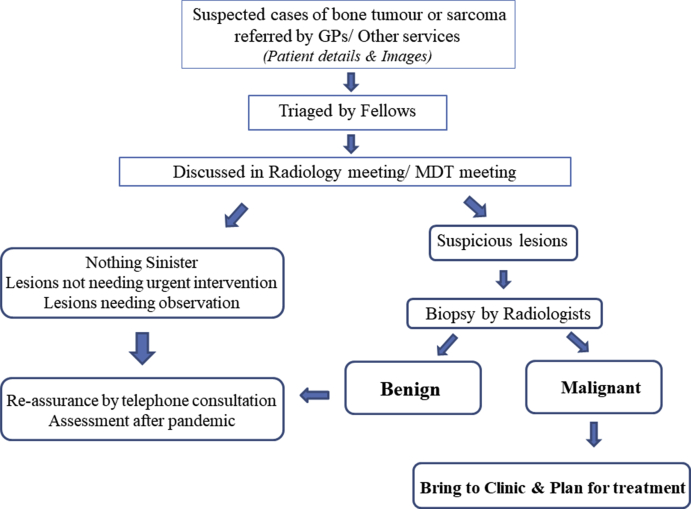
Triaging referred patients from General Practitioners (GP) and accurately determining the severity of presenting disease is one of the key pillars of any cancer service in the UK. An appropriate referral pathway was implemented whereby patients needing biopsies, urgent treatments and urgent discussion in MDT to narrow down on diagnosis and plan further treatment were brought forward (Fig. 1). Benign conditions and conditions which were not deemed life-threatening were contacted over the telephone and re-assured about their prognosis to be seen at a later date. The main aim of this exercise was to reduce the unnecessary patient attendance at hospital. Suspicious lesions needing a tissue diagnosis were brought forward and biopsied by radiologists following all protective measures. Patients with suspicious new lesions, biopsy proven cancer diagnoses and those needing urgent/emergency surgery were the only patients who were brought to a face-to-face clinic in the hospital.
Fig. 1.
Flowchart depicting the workflow of patient triages planned during the COVID-19 pandemic.
3. MDT functioning – moving the virtual way
Bone tumours and soft tissue sarcomas are unique. They have a very low incidence and amount to less than 1% of all cancers.8 These rare cancers are managed only in specialised centres. Their complexity is compounded by the fact that they are not site specific, sex specific nor age specific like other cancers. Hence, to manage this important group of tumours, a comprehensive and well attended MDT comprising of multiple specialists across specialities including pathology, paediatrics, radiology, spinal surgery, cardiothoracic surgery and orthopaedic oncology is vital. A routine MDT of the Oxford sarcoma service would typically involve around 40 specialists in an auditorium gathering on a weekly basis. In 2019, on an average 48 cases(37-69) were discussed every week in the MDT over a time period of 2 hours. The number of participants in these meetings is a necessity to plan treatments but however meeting in person increases the risk of disease transmission amongst healthcare providers and contravenes the government policy of social distancing and spacing. In an effort to reduce this risk a virtual MDT was established. Key enablers – radiologist, pathologist, orthopaedic oncologist andadministrative co-ordinator - still attend the meeting in person with increased interpersonal spacing. Other specialists dial into the meeting via software platforms and have access all relevant information and relevant images. This measure is found to be effective and the past seven MDT meetings have been held via a virtual platform with only 8 key members attending in person and the rest dialling in whenever their input is required.
4. Out-patient clinics
Prior to the pandemic, 43 patients (27–55) were seen face-to-face in sarcoma clinics every week. Following the implementation of social distancing measures and the need to minimise unnecessary patient visits to hospital, only patients with active disease which warranted urgent surgery were brought to clinics. Triages and MDT discussions helped in identifying patients who needed urgent intervention. All follow-up patients and patients with benign disease which were not life-threatening had telephonic/video consultations. In the first month after implementation of these measures, only 8 patients (6-11) were seen face-to-face every week in clinic. Compulsory use of face masks, use of hand sanitizers and social distancing of 2 m were measures implemented strictly in the waiting area and in the consultation cubicle.
5. Surgery
Surgery is an essential part of sarcoma treatment and in some cases, the only modality of treatment to the patient. The need to keep regular theatre lists functioning is a necessity in cancer treatment as delaying surgery would compromise the efficacy of the multidisciplinary treatment, outcomes and potential life expectancy. The risk of cancer patients contracting the virus and the risk of postponing cancer care are key factors which need to be analysed and decisions need to be taken on a case-to-case basis. Patients who warranted surgery were classified as per guidelines issued by the NHS.6 Patients were categorised as follows:
-
-
Priority level 1a: Emergency operation needed within 24 h to save life
-
-
Priority level 1b: Urgent surgery needed within 72 h
-
-
Priority level 2: Elective surgery to save life/prevent disease progression beyond operability
-
-
Priority level 3: Elective surgery which can be delayed for 10–12 weeks and will have no predicted negative outcome
Surgery for priority level 3 patients was postponed to a suitable time after the pandemic. All patients were informed of this plan and the necessity to follow such a rigorous triage system was vital. Patients in priority levels 1a, 1b and 2 were assessed on a case-to-case basis. Aggressiveness of the disease, timing from neo-adjuvant treatment and general condition of patient were taken into account for each patient. Based on the urgency of surgery required, surgical lists were planned.
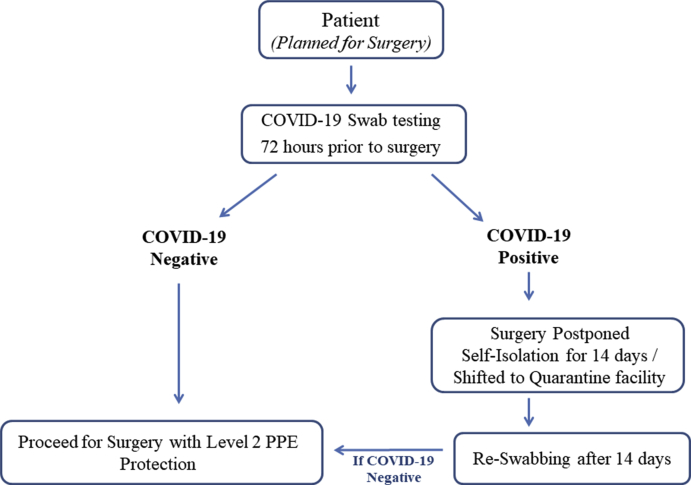
6. Use of COVID-free hospital for surgery
The need for COVID-free hospitals to manage cancer care was recommended following initial reports from Lombardy, Italy to mitigate transmission.9 A non-public hospital in Oxford (which was effectively nationalised by the NHS at the start of the pandemic) was used to manage COVID-negative cases which needed surgery on urgent basis. COVID-free hospitals managing cancer patients serve as an essential step to mitigate disease transmission and protect patients from disease contraction. All patients planned for surgery followed a definitive pathway which included pre-operative screening for COVID 72 h prior to surgery (Fig. 2). Only COVID-negative patients were admitted in the hospital. No attenders were allowed inside the hospital. Level 2 PPE was employed by the entire surgical team during the procedure. All measures were aimed at protecting both the patient and also healthcare professionals from contracting and transmitting the disease.
Fig. 2.
Pre-operative swab testing procedure and implemented surgical pathway.
7. Adjuvant therapy
Chemotherapy and radiation therapy are key aspects in bone tumour and soft tissue sarcoma management. Initial reports from a nationwide analysis in China showed that patients with cancer had a higher risk of COVID-19 infection and a poorer outcome.10 The authors also recommended an intentional postponing of adjuvant chemotherapy or elective surgery for stable cancer. The level of immunosuppression associated with individual therapies also needs to be taken into consideration. Patients requiring neo-adjuvant therapies were discussed in the MDT and decision making was made on a case-to-case basis. Multiple trips to hospitals to receive adjuvant therapies could increase risk of disease contraction. Categorising patients by treatment intent and risk-benefit ratio associated with treatment is essential. Patients who required adjuvant treatment with curative intent with a high chance (>50%) of success were prioritised and managed with respective therapies.
8. Conclusion
Balancing the risks of the COVID-19 pandemic with measures to mitigate transmission against the undeniable risk of increased morbidity and mortality for cancer patients is a challenge. For many patients, the benefit of ensuring a well-delivered cancer treatment pathway outweighs the risk of COVID-19 infection. Treatment tailored for each patient is of utmost importance during such a pandemic as the risk of exposure varies from patient to patient. Virtual MDTs and telephonic consultations are new activities which could we be the way forward to manage sarcoma patients until the pandemic settles down. Triaging patients who need urgent surgery, avoiding unproductive hospital attendances, following social distancing measures, use of level 2 PPE and shifting of operative work to COVID-free hospitals are important organisational changes we employed in our sarcoma service to deliver continued cancer care during the pandemic. The COVID-19 virus and the resultant pandemic needs to be effectively managed and normal delivery of service is essential but not at the expense of increased morbidity and mortality of cancer patients.
Funding statement
No funding granted or received.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Zhu H., Wei L., Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020 Mar 2;5:6. doi: 10.1186/s41256-020-00135-6. PMID: 32226823; PMCID: PMC7050114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saini K.S., de Las Heras B., de Castro J. Effect of the COVID-19 pandemic on cancer treatment and research [published online ahead of print, 2020 Apr 24] Lancet Haematol. 2020 doi: 10.1016/S2352-3026(20)30123-X. S2352-3026(20)30123-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vrdoljak E., Sullivan R., Lawler M. Cancer and coronavirus disease 2019; how do we manage cancer optimally through a public health crisis? [published online ahead of print, 2020 Apr 18] Eur J Canc. 2020;132:98–99. doi: 10.1016/j.ejca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Indini A., Aschele C., Cavanna L. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey [published online ahead of print, 2020 Apr 6] Eur J Canc. 2020;132:17–23. doi: 10.1016/j.ejca.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Public Health England COVID-19: infection prevention and control (IPC) 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infectionprevention-and-control (accessed 10May 2020)
- 6.Guidance for trusts on the management of non-coronavirus patients requiring acute treatment: cancer – NHS. https://covid19.aischannel.com/guidelines-nhs/files/clinical-guide-for-the-management-of-non-coronavirus-patients-requiring-acute-treatment-cancer
- 7.Joint statement from the British sarcoma group, British orthopaedic oncology society and the chairs of the regional sarcoma advisory groups relating to COVID-19. https://wmcanceralliance.nhs.uk/images/Documents/Covidwww.boos.org.uk
- 8.Franchi A. Epidemiology and classification of bone tumors. Clin Cases Miner Bone Metab. 2012 May;9(2):92–95. Epub 2012 Sep 30. PMID: 23087718; PMCID: PMC3476517. [PMC free article] [PubMed] [Google Scholar]
- 9.Restivo A., De Luca R., Spolverato G., Italian Society of Surgical Oncology (SICO) The need of COVID19 free hospitals to maintain cancer care. Eur J Surg Oncol. 2020 Apr 22 doi: 10.1016/j.ejso.2020.04.003. S0748-7983(20)30400-5. Epub ahead of print. PMID: 32336627; PMCID: PMC7175900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335-337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]