Abstract
Within a time span of only a few months, the SARS-CoV-2 virus has managed to spread across the world. This virus can spread by close contact, which includes large droplet spray and inhalation of microscopic droplets, and by indirect contact via contaminated objects. While in most countries, supermarkets have remained open, due to the COVID-19 pandemic, authorities have ordered many other shops, restaurants, bars, music theaters and indoor sports centers to be closed. As part of COVID-19 (semi)lock-down exit strategies, many government authorities are now (May-June 2020) allowing a gradual re-opening, where sometimes indoor sport centers are last in line to be permitted to re-open. This technical note discusses the challenges in safely re-opening these facilities and the measures already suggested by others to partly tackle these challenges. It also elaborates three potential additional measures and based on these additional measures, it suggests the concept of a certificate of equivalence that could allow indoor sports centers with such a certificate to re-open safely and more rapidly. It also attempts to stimulate increased preparedness of indoor sports centers that should allow them to remain open safely during potential next waves of SARS-CoV-2 as well as future pandemics. It is concluded that fighting situations such as the COVID-19 pandemic and limiting economic damage requires increased collaboration and research by virologists, epidemiologists, microbiologists, aerosol scientists, building physicists, building services engineers and sports scientists.
Keywords: Corona virus, Sports club, Gym, Fitness, Aerodynamics, Building ventilation, Filters, Face masks
1. Introduction
Within a time span of only a few months, the SARS-CoV-2 virus has managed to spread to many countries in the world and to generate a world-wide crisis. Many countries have closed their borders and some have imposed long lockdowns or semi-lockdowns on their inhabitants. International, national and local sports and cultural events have been canceled or at least postponed. Restaurants, bars, music and movie theaters and indoor sports centers had to close their doors. In spite of these measures, on 31 May 2020, the European Centre for Disease Prevention and Control reported nearly 5.9 million cases of SARS-CoV-2 including 364,891 deaths world-wide [1]. SARS-CoV-2 is not only a highly transmissible but also a deadly virus. Several sources have suggested that the COVID-19 virus is transmitted by respiratory droplets and by contact routes [[2], [3], [4], [5], [6], [7]]. Direct transmission by droplets can occur between people when infective droplets produced by sneezing, coughing, talking, singing or simply exhaling reach the mucosae (mouth and nose) or conjunctiva (eyes) of another person. That is why during the COVID-19 pandemic, many countries world-wide have declared – sometimes by law – a so-called “social distance” of about 1.5 m, 2 m or 6 ft (actual value dependent on the country) to be kept between individuals. While this is not really a social distance but rather a physical distance, this distance is considered not only feasible but by many also effective because it is sometimes assumed that the largest respiratory droplets will settle by gravity and/or evaporate before having traveled this distance to impact the other person. However, recent studies have demonstrated that droplets from coughing and sneezing can sometimes travel 4 m or even 6 m and more, co-propelled by the turbulent air jet by the coughing or sneezing person [[8], [9], [10]]. Indirect or contact route transmission can occur via fomites such as skin cells, hair, clothes, handrails, keyboard buttons and other objects, where virus is deposited after contact with an infected person. There is mounting evidence that the virus can also be transmitted by inhalation of microscopic droplets (i.e. aerosols) at short-to-medium range because the virus has been found in small aerosols that can remain in the air for hours, and it has been shown to maintain viability in such aerosols [[11], [12], [13], [14], [15]]. Thus, it would be judicious to apply precautionary measures also for the airborne route.
Respiratory droplets are generated from the fluid lining of the respiratory tract during the expiratory activities breathing, talking, coughing and sneezing [16,17] and the size of these droplets can range from about 0.1 μm to 1 mm [18]. While a sneeze can generate 10,000 droplets or more, a cough can produce about 100–1000 droplets and talking can produce about 50 droplets per second [19,20]. Sneezing and coughing can generate a substantial fraction of larger droplets and breathing mainly generates the smaller range of droplets or aerosols. However, as stated by Mittal et al. [21], previous studies have noted that “even though breathing generates droplets at a much lower rate, it probably accounts for more expired bioaerosols over the course of a day than intermittent events such as coughing and sneezing”.
Indoor sports centers are environments that house equipment and services for the purpose of physical exercise. The equipment and services can cover a very wide range of physical activities: (i) cardio equipment with stationary exercise bicycles, treadmills, rowing machines and elliptical trainers, (ii) workout equipment with free weights and weight-based exercise machines, (iii) group exercise services where trainers or instructors provide classes in aerobics, cycling/spinning, step yoga, pilates, stretching, etc. and (iv) additional facilities such as indoor running tracks, basketball courts, squash courts, boxing areas, ice rinks and swimming pools. In the present technical note, we focus on the categories (i), (ii) and (iii), where the people exercising are not moving throughout the room while performing a particular exercise but instead remain confined at a rather fixed position in the room.
Sports have an important role in the society. They contribute to several of the United Nations Sustainable Development Goals [22] (Fig. 1 ). For centuries, sports have succeeded in bringing people together. Even in the darkest of times, sports have been practiced to maintain at least a semblance of normality and to build and sustain morale. During war, soldiers would exercise some sports in the trenches to pass time and enjoy themselves [23,24]. Also during the COVID-19 pandemic, sports have been and still are undoubtedly important [25,26]. However, the fact that in many countries indoor sports centers have been closed has equally undoubtedly made it more difficult for people to cope with this pandemic and the associated (semi-)lockdown [27]. A long closure of indoor sports centers could also lead to detrimental economic consequences, with bankruptcies and the associated negative consequences throughout the whole supply chain.
Fig. 1.
Sports contributes to several of the Sustainable Development Goals of the United Nations [22].
During the COVID-19 pandemic, in most countries, supermarkets have remained open, but many other shops, restaurants, bars, music theaters and indoor sports centers have been closed. As part of a COVID-19 (semi)lock-down exit strategy, many government authorities are allowing a gradual re-opening, where sometimes indoor sport centers are last in line to be permitted to re-open. This technical note discusses the challenges in re-opening these facilities and the measures already suggested by others to partly tackle these challenges. It also elaborates three additional measures and based on the implementation of some of these additional measures, it suggests the concept of a certificate of equivalence that could allow indoor sports centers with such a certificate to re-open safely and more rapidly. It also attempts to stimulate increased preparedness of indoor sports centers that should allow them to remain open safely during potential next waves of this virus as well as future pandemics. As an example, the situation of the Netherlands is taken, but similar situations are undoubtedly present in many countries around the world.
This document does not attempt to be complete. Given the urgency of the situation and the historical lack of research on infectious diseases and sports, it attempts to provide a first overview of challenges, current measures and additional measures supplemented with a potential practical framework.
2. Challenges and current measures for indoor sports centers
In indoor sports centers, typically the facilities such as exercise equipment, lockers, showers and all means to access them such as keyboard buttons, handlebars, railings and doorknobs are used by many visitors, which could result in many opportunities of infection transmission, either directly (by expired droplets at short range) or indirectly (by fomites). Therefore, a wide range of precautionary measures can and should be taken. The NOC*NSF (Dutch Olympic Committee * Dutch Sports Federation) is the overarching organization for all sports activities, professional and recreational, in the Netherlands. This organization has issued a “Protocol for Responsible Physical Exercise” [28]. Based on this document, the Dutch organization “NL Actief” has published a similar document but especially focused on indoor sports centers: “Protocol for Responsible Physical Exercise – Branche: Fitness” [29]. This protocol contains a comprehensive list of precautionary measures and is intended to supplement the already imposed measures by the Dutch National Institute of Public Health and the Environment (RIVM) and the protocol by the NOC*NSF. It explicitly focuses on those physical activities that do not involve physical contact between persons. The precautionary measures are provided in four categories: for (i) operators, (ii) visitors, (iii) employees and (iv) suppliers. The measures should be applied on top of the basic measures that hold for all people in the Netherlands such as keeping the 1.5 m physical distance at all times, sneezing and coughing in one's elbow cavity and using paper towels, staying at home after you have tested positive for the virus, staying at home when showing at least one of the typical symptoms, staying at home when one of your housemates has tested positive for the virus and staying at home when one of your housemates has a fever (38°C and above) or a tightness feeling. The additional measures include [28,29]:
-
•
For operators: controlling the maximum number of visitors and routing inside the buildings, providing masks, gloves, glasses and regular disinfection of payment terminal keyboards, door handles and other surfaces, appointing a COVID-19 supervisor and instructions for employees including pointing visitors to unsafe behavior;
-
•
For visitors: required reservation of a time slot, only visiting with members from the same household, avoiding public transport, using the sanitary facilities at home instead of in the center, only starting exercise after having washed the hands and leaving the center immediately after having finalized your physical activity;
-
•
For employees: working at home as much as possible, regular washing of the hands before every meal, after use of the sanitary facilities, after having traveled with public transport, and after cleaning, not sharing tools with other employees, keeping personal tools clean and disinfected;
-
•
For suppliers: announcing arrival 15 min in advance, wearing gloves, announcing where the goods will be placed, giving preference to delivery at the doorstep.
The protocol also advises a gradual re-opening in three phases, from a first and limited opening that should have started on 15 March 2020 to a full regular opening including catering facilities afterwards.
In spite of this document, the Dutch government decided on 6 May 2020 that indoor sports centers would have to remain closed until 1 September 2020. The main argument provided for this decision by the Ministry of Health, Welfare and Sports pointed to the issue that was not addressed in the Protocol document: concern about the increased amount of aerosols expired during physical exercise that can remain in the air for a long duration [30]. They also raised the concern that it was yet insufficiently clear whether asymptomatic SARS-CoV-2 carriers also expire such aerosols. Given the current status of knowledge on aerosol expiration and on SARS-CoV-2, both concerns seem justified. Indeed, there is evidence that deep exhalation (as with physical exercise) produces more aerosols [17,31], there are indications of SARS-CoV-2 infection in 12 fitness dance classes in South Korea [32] and recent studies do suggest that asymptomatic carriers can transfer the SARS-CoV-2 virus [33,34].
To the best of our knowledge, there are only a few studies that provide some indirect indication of how physical exercise influences the emission of respiratory droplets. Johnson and Morawska [17] found that deep exhalation resulted in a 4- to 6-fold increase in aerosol concentration and rapid inhalation produced a further 2- to 3-fold increase in concentration. In contrast, rapid exhalation had little effect on the measured concentration. Almstrand et al. [31] analyzed the effect of airway opening on the production of exhaled particles. Ten healthy test subjects were asked to perform different breathing maneuvers in which the initial lung volume preceding an inhalation to total lung capacity was varied between functional residual capacity (FRC – the volume of air in the lungs at the end of passive expiration) and residual volume (RV – the volume of air in the lungs after full exhalation). They measured exhaled particles in the size range 0.30–2.0 μm. The number of exhaled particles demonstrated a 2- to 18-fold increase after exhalations to RV compared with exhalations where no airway closure was shown [31]. However, both studies were performed with persons not conducting physical exercise, therefore more research is needed on whether and to what extent physical exercise can further increase the generation of aerosols.
Considering the contents of the protocol [29], the aforementioned studies on increased aerosol production by deep exhalation and rapid inhalation [17,31], the indication of infection in the fitness dance classes [32] and the aforementioned studies on virus viability in small aerosols that can remain in the air for hours [[11], [12], [13], [14], [15]], it would be judicious to apply additional precautionary measures to handle the potential surplus of aerosols produced by breathing during physical exercise in indoor sports centers. While the study [32] suggested that vigorous exercise in confined spaces should be minimized during outbreaks, the present authors do not necessarily share that opinion, because many other parameters are involved, including those mentioned in the next section, that have received relatively little attention in most SARS-CoV-2 publications so far.
3. Towards a certificate of equivalence with additional measures
3.1. High-intensity building ventilation
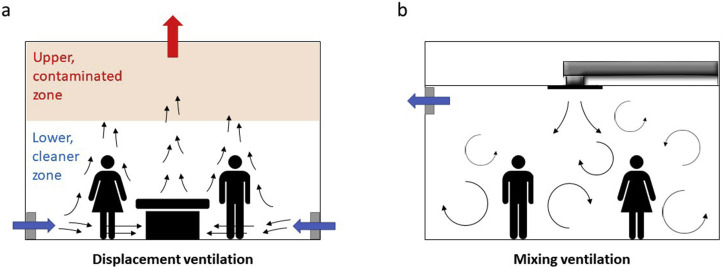
Building or room ventilation can be defined as “the process by which ‘clean’ air (normally outdoor air) is intentionally provided to a space and stale air is removed” [35]. Several authoritative books and extensive reviews have been provided on the topic in the past decades (e.g. Refs. [[36], [37], [38], [39]]). Ventilation can be driven by mechanical systems (mechanical ventilation) or by natural forces such as wind and buoyancy (natural ventilation) or a combination of both. Some mechanical systems employ recirculation of heated or cooled air for the purpose of energy conservation. Strictly, according to the above-mentioned AIVC definition, recirculated air cannot be labeled as ventilation. In this technical note, we strictly follow the definition that ventilation air is outdoor clean air free of infectious aerosols. In its simplest case, high-intensity natural ventilation consists of opening windows and doors in opposite facades (if weather allows). Two main categories of building ventilation are displacement ventilation and mixing ventilation. In displacement ventilation, the outdoor air is generally supplied at a low velocity from diffusers near the floor level and extracted above the occupied zone, near or at the ceiling (Fig. 2 a). In mixing ventilation, the outdoor air is supplied at a high velocity outside the occupied zone, such as near or at the ceiling, and is mixed with the stale indoor air (Fig. 2b), with the intention to dilute the concentrations of e.g. aerosols, after which part of this mixed air is extracted out of the room. Displacement ventilation generally leads to lower aerosol concentrations in the occupied zone and an overall better ventilation efficiency than mixing ventilation, but locating diffusors and ducts near the floor is not always feasible. Mixing ventilation is easier to implement with diffusors and ducts near the ceiling but generally leads to more evenly distributed and overall higher aerosol concentrations in the enclosure. To our knowledge, the vast majority of indoor sports centers are equipped with mixing ventilation systems, but in view of reducing infection risk, the future design of such centers could benefit from displacement ventilation systems if sufficient buoyancy forces will act to generate upward movement of the air.
Fig. 2.
Concept of (a) displacement ventilation; (b) mixing ventilation.
Given the low inertia of the aerosols, after expiration, their movement in the enclosure will rapidly be determined by the indoor airflow patterns. These patterns can be very complex as demonstrated by many earlier studies [[40], [41], [42], [43], [44], [45], [46], [47], [48]]. Persons are sources of heat, vapor and CO2. Not only the expired air and aerosols will therefore be exposed to the resulting upward buoyancy forces, but also a – mainly – thermal convective plume is present around people that causes a clear upward airflow near their body [49]. The movement of people, and finally the ventilation system itself, also contribute to the complexity of the airflow patterns in enclosures.
Li et al. [50] extensively reviewed studies on the role of ventilation in the airborne transmission of infectious agents in buildings. They concluded that there is clear evidence of an association between ventilation, air movement in buildings and the transmission/spread of infectious diseases such as influenza and SARS. However, they also indicated that there was insufficient data to specify and quantify the minimum ventilation requirements in hospitals, schools, offices and other buildings to avoid the spread of these and other infectious diseases via the airborne route. Indeed, ventilation implies air movement and also aerosol movement inside the building, and in some cases the ventilation system uses recirculation of part of the exhausted air back to the inside, which, in case of infectious diseases, is undesirable [51]. Therefore, only high-intensity ventilation without recirculation should be applied in this type of pandemic in order to effectively and quickly remove aerosols and keep indoor aerosol concentrations as low as possible. If recirculation is applied, the recirculated air should be treated so that infectious aerosols are physically removed and/or pathogens are inactivated, for example by UV germicidal irradiation.
Ai and Melikov [52] reviewed studies on the airborne spread of expiratory droplet nuclei between the occupants of indoor environments, with specific focus on the spread of droplet nuclei from mouth/nose to mouth/nose for non-specific diseases. They stressed the importance of indoor airflow patterns and indicated that future research is needed in three specific areas: the importance of the direction of indoor airflow patterns, the dynamics of airborne transmission and the application of CFD simulations.
In most countries world-wide, building ventilation is mandatory by law, as an essential requirement for health and comfort in buildings. In the Netherlands, the minimum requirements for the ventilation of buildings are prescribed by the Building Code (“Bouwbesluit”) published in 2012, and last amended in 2020 [53]. The minimum ventilation flow rates in terms of provision of fresh air for different types of utility buildings are given in Table 1 . A distinction is made between new buildings and existing buildings. In 2008, the Dutch Guidebook for Sports Accommodations was published [54] and in 2014 specific guidelines for sports facilities for people with disabilities were provided [55]. These guidelines stipulate a minimum ventilation flow rate of 11.1 dm³/s per exercising person for sports halls, which is 70% above the minimum required value in the Dutch Building Code for new buildings and even 3.2 times higher for existing buildings. These higher values are probably intended to try to take into account the higher heat, vapor, CO2 and aerosol emission by people during physical exercise. In addition, these specific guidelines for indoor sports accommodations [54,55] suggest a total of 6 air changes per hour (ACH) for fitness spaces (i.e. the volume of air in the room is replaced by clean air 6 times per hour), while the ACH for aerobics and martial arts spaces should be 8 h−1 and for indoor cycling 10 h−1. In view of the COVID-19 pandemic, ASHRAE, the American Society of Heating, Refrigerating and Air-Conditioning Engineers, has acknowledged the potential for aerosol transmission of SARS-CoV-2 and states that facilities of all types should follow, as a minimum, the latest published standards and guidelines and good engineering practice [56]. ASHRAE Standard 62.1 specifies ventilation rates for acceptable indoor air quality [57]. For gyms, health clubs, aerobics rooms, and weight rooms, the minimum outdoor airflow rate is 10 dm3/s/person. This is higher than specified for most retail (3.8 dm³/s/person, except for beauty and nail salons where 10 dm³/s/person is required) and educational buildings (3.8–5 dm³/s/person). Note that the ASRHAE value for gyms aligns well with the 11.1 dm³/s from the Dutch guidelines [55].
Table 1.
Minimum required ventilation flow rates for different types of utility buildings according to the Dutch Building Code [53].
| Function | Requirement in dm³/s/person |
|
|---|---|---|
| New buildings | Existing buildings | |
| Childcare | 6.5 | 3.44 |
| Meeting | 4 | 2.12 |
| Healthcare, bed area | 12 | 3.44 |
| Healthcare, other areas | 6.5 | 3.44 |
| Industrial | 6.5 | 3.44 |
| Office | 6.5 | 3.44 |
| Hotel, dormitory | 12 | 6.40 |
| Education | 8.5 | 3.44 |
| Sports | 6.5 | 3.44 |
| Shopping | 4 | 2.12 |
3.2. Filtering
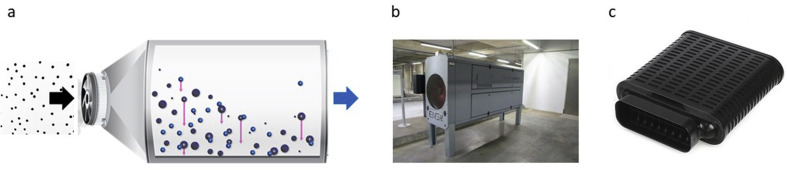
Technological solutions exist for removing moderate to large fractions of aerosols from airstreams inside buildings. These systems can be installed either in the ducts of the HVAC (Heating, Ventilation and Air-Conditioning) system or freely inside the room itself. In both cases, they will need to provide sufficiently high clean air delivery rates. In the former case, they should be able to handle the high volume flow rates through the ducts, while in the latter, they should be able to handle high enough flow rates in balance with the room ventilation flow rates. A first option are HEPA filters (high-efficiency particulate absorbing or high-efficiency particulate arrestance). HEPA filtering can be very effective because these filters remove at least 99.95% of the particles with diameter 0.3 μm and larger fractions of the other sizes. The initial cost is relatively low but the operational costs are high, as the flow resistance of these filters is very high and therefore a lot of energy is required to overcome the large pressure drop over these filters that is unavoidably associated with the large flow rates. HEPA filters are used in clean rooms and some hospital operating theaters, but their future large-scale application for indoor sports centers might be hampered by the associated energy costs. As an alternative, electrostatic precipitators (ESPs) or similar devices can be considered. An ESP is a filtration device where the air is forced to flow through a largely open box by a small industrial fan and where the solid or liquid particles are electrically charged and collected on a generally grounded plate inside the device [58] (Fig. 3 ). The initial cost of an ESP can be relatively high but the operational cost is low due to low energy consumption. However, the efficiency is generally also lower than that of HEPA filters. On-site measurements on a particular commercially available moderate-size ESP (Fig. 3b) have indicated an efficiency of 70% for PM10 and about 45% for PM2.5 [59], which is nevertheless still considerable given that when the ESP is mounted inside the room itself and – depending on the ventilation rate – the same air could be handled this way multiple times yielding higher efficiencies.
Fig. 3.
(a) Concept of ESP with positive ionisation; (b) photo of moderate-size ESP (2.8 × 0.72 × 1.28 m³) in an indoor environment. (Source: ENS Technology, reproduced with permission); (c) photo of small-size ESP (0.79 x 0.40 x 0.13 m³) (Source: PlasmaMade, reproduced with permission).
3.3. Masks
A distinction is made between surgical masks and respirator masks. A surgical mask or face mask is a loose-fitting, disposable device intended to block splashes and large droplets, and it can also filter out some aerosols. A respirator on the other hand should provide a close facial fit and a very efficient filtration of also the aerosols.
Chen and Willeke [60] tested the collection efficiency of surgical masks and respirators with aerosol-size spectrometers. They found that surgical masks with only a shell with a coarse pore structure passed 80% of the aerosols below 1 μm with almost no dependency on the flow. On the other hand, surgical masks including specific filter material allowed only 25% passage at 5 L/min to 70% at 100 L/min [60]. He et al. [61] found that surgical masks sealed to a manikin passed less than 20% of aerosols below 1 μm at flow rates of 15–85 L/min; without sealing, the penetration was higher, up to 45%. Van der Sande et al. [62] analyzed the transmission reduction potential provided by personal respirators, surgical masks and home-made masks when worn during a variety of activities by a small number of healthy volunteers and a simulated patient. They found that all types of masks did reduce aerosol exposure relatively stably over time and unaffected by duration of wear and type of activity, but with a high degree of variation by type of mask [62]. Unsurprisingly, personal respirators were most efficient, followed by surgical masks, followed by home-made masks.
The use of masks is fairly well accepted in many countries in Asia, where often wearing a surgical mask when you are ill is considered as a token of respect towards others. However, in many other countries, the use of masks has been an issue of debate, although currently governments are implementing the mandatory use of surgical or home-made masks at an increasing pace [[63], [64], [65], [66], [67], [68], [69], [70]]. Indeed, while initially in several countries, scientists, political advisors and politicians have made some radical statements pro and con the usefulness of wearing of masks by the public in various situations, an overview of the recent peer-reviewed scientific literature provides a more moderate image (e.g. Ref. [[60], [61], [62]]). There are indeed clear pros and cons concerning masks for the public. First, many will agree that the best quality masks should be provided to our healthcare facilities and only after abundant stock there, could one consider distribution among the public The FDA [69] explicitly states that the Centers for Disease Control and Prevention (CDC) do not recommend the general public to wear N95 respirators to protect themselves from respiratory diseases such as COVID-19. Instead, these are considered critical supplies that must continue to be reserved for health care workers and other medical first responders. Second, facial masks could provide a false sense of security, as people could put them on leaving leakages, touching the outside of the masks, etc., but there is no evidence that this could be detrimental for the general public [70]. The masks also do not cover the eyes that could also be receptors of the virus. Third, wearing masks can have a negative psychological impact on people by reducing the level of human interaction [71]. Conversely, it has been demonstrated that facial masks, even of the most primitive type, can provide some protection (e.g. Ref. [62]). Using such masks in turn can allow people to exercise more freedom in the society, including the use of public transportation and gathering in public places, and could assist in restarting economic activity. In terms of indoor sports centers, the future development of sports face masks is not unlikely. These should provide a compromise between droplet and aerosol collection efficiency, large respiration flow rates and resistance to sweat.
3.4. Certificate
Ideally, one would want to know the specific infection risk for a given activity in a given building as a function of occupation, ventilation settings and other relevant parameters, and decide on re-opening based on risk assessment. However, many aspects of SARS-CoV-2 are still unknown and might remain unknown for a considerable time to come. It could take years before knowledge will be available on which viral dose during which time is an infection risk for a given person performing a given activity. Nevertheless, governments are under pressure from the economy and the public to resume – at least gradually – economic and leisure activity. This should be done as safely as possible. Therefore, in spite of the many unknowns and in view of safely re-opening indoor sports centers, government authorities could consider the implementation of a certificate of equivalence in terms of aerosol exposure. This certificate would be obtained if, apart from the measures outlined in documents such as [28,29], a combination of some of the three above-mentioned measures (high-intensity ventilation, filtering, facial masks) can demonstrably and quantifiably lead to a concentration of aerosols that is equivalent in terms of exposure (including concentration and inhalation) to the exposure occurring in other facilities that are allowed to re-open earlier, such as shops, restaurants and bars, taking into account the maximum allowed number of people per floor area.
A first substantial step towards equivalence could be high-intensity ventilation in order to compensate for the increased aerosol generation and the increased aerosol inhalation by physical exercise. A small calculation example is presented, in which we do not consider specific government-imposed limits in terms of maximum number of persons per floor area per type of building – as some of these numbers are being adjusted frequently. Consider an indoor sports center with a total rectangular floor area of 50 × 20 m2 = 1000 m2. Physical distancing of 1.5 m will generally not be an issue as many of the exercise machines already consume considerable space. We assume that the center, in setting up the machines, very strictly adheres to the required physical distancing between exercising visitors of 1.5 m. This implies that around every machine a 3 × 3 m2 perimeter is indicated that is a “no go” zone for visitors using other machines. In this situation, a maximum of 96 visitors (assuming no corridor space) can be present at the same time. This corresponds to about 1 person per 10 m2. Table 2 provides the resulting minimum ventilation flow rates for this center and for a shop of the same floor area as provided by the Dutch Building Code. For the sports center, also the larger ventilation flow rates recommended by the Dutch Sports Guidelines [54,55] are listed. Table 2 shows that for the most critical situation of new buildings, the ACH of a fitness area as recommended by Ref. [54,55] is about 20 times larger than the minimum for a shop of equal floor area and the same maximum number of 100 persons present as required by the Dutch Building Code. Note however that the ventilation rates from the building code are minimum requirements and that actual ventilation rates in e.g. supermarkets are probably designed and set to be higher than those in the Building Code.
Table 2.
Minimum required ventilation flow rates (Q) in dm³/s and air change rates per hour (n) for an indoor sports center and a shop of 1000 m2 floor area, 5 m height and 100 persons present, according to Ref. [49,[[54], [55]]].
| Function | Indoor sports center |
Shop |
||
|---|---|---|---|---|
| Q (dm³/s) | n (h−1) | Q (dm³/s) | n (h−1) | |
| Building Code (new buildings) [49] | 650 | 0.47 | 400 | 0.29 |
| Building Code (existing buildings) [49] | 344 | 0.25 | 212 | 0.15 |
| Sports Guidelines [[54], [55]] | ||||
| General (11.11 dm³/s/person) | 1111 | 0.80 | ||
| Fitness area | 8333 | 6 | ||
| Aerobics and martial sports area | 11111 | 8 | ||
| Indoor cycling area | 13889 | 10 | ||
Equivalence in terms of aerosol exposure between the indoor sports center and the shop could be achieved by balancing a number of factors. Some main factors that can be controlled and engaged to reduce aerosol concentrations are the higher ventilation rates, limiting the number of persons in the indoor sports center well below the maximum occupation and limiting the intensity of the exercise. On the other hand, factors contributing to aerosol exposure are the higher aerosol production by exercising people and the possibility that aerosols can be inhaled deeper into the respiratory system by exercising persons. The studies by Johnson and Morawska [17] and Almstrand et al. [31] provide a first indication of the aerosol production during deep inhalation and exhalation, where an increase up to a factor 18 has been found between functional residual capacity and residual volume. However, at present there is insufficient information in the scientific literature to argue that this 18-fold increase in aerosol production could be balanced by a 20-fold increase in ventilation flow rates. Indeed, both studies [17,31] were performed with persons not performing physical exercise and it is possible that physical exercise increases the aerosol production even further. Note also that even the best mixing ventilation systems will not provide perfect mixing and therefore provide non-uniform aerosol concentrations will occur in the room. Much more research is needed on each of these topics. But if this extra information would be available, it seems plausible that the ventilation flow rates could be augmented and the maximum allowed number of people and the intensity of the physical exercise could be reduced in such a way that they balance the higher aerosol exposure (production and inhalation) leading to a quantifiably equivalent situation between indoor sports centers and other spaces such as shops, restaurants and bars.
Key parameters in terms of ventilation are the floor area A, the room height H, the required ventilation flow rate per person (Q/N) with N the number of persons, the maximum allowed number of persons per unit floor area (N/A) and the air change rate per hour n. Eq. (1) represents the simplified mass balance in the room assuming a uniform concentration c in the room with volume V, a total aerosol production rate G and a clean air ventilation flow rate Q. Under steady-state conditions, it yields Q = G/c which can be rewritten as Eq. (2), where g is the aerosol production rate per person. Eq. (2) can be expanded into Eq. (3) that relates N/A to Q/N or to g/c.
| (1) |
| (2) |
| (3) |
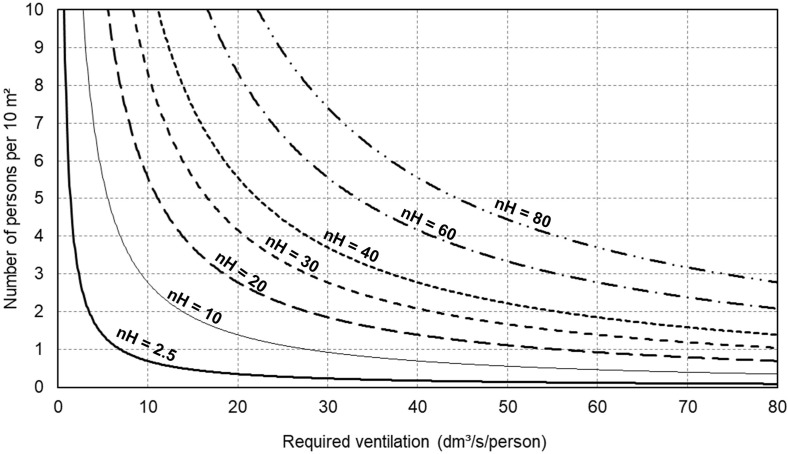
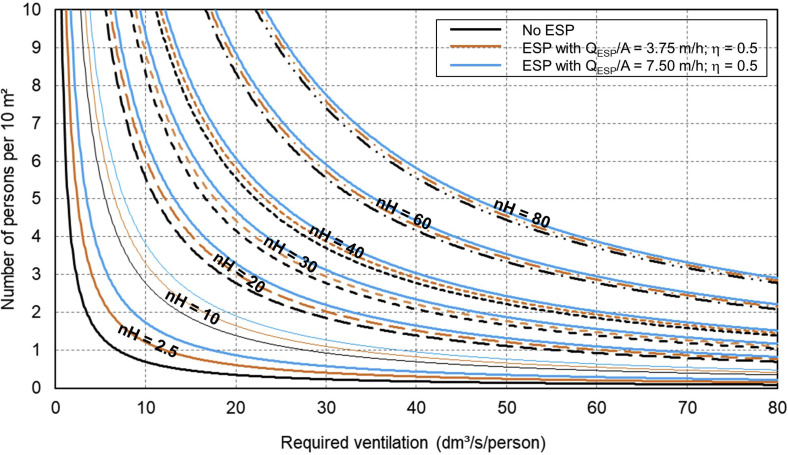
Based on Eq. (3), Fig. 4 presents a simple nomogram that provides N/A per 10 m2 as a function of Q/N with the product of n and room height H as a parameter, with nH in unit m/h. Given the required N/A, the air change ratio per hour n and the room height H, the maximum number of persons per 10 m2 can easily be determined.
Fig. 4.
Nomogram of number of persons per 10 m2 as a function of required ventilation rate per person, with the product of air change rate per hour (n) and room height (H) as a parameter (nH with unit m/h).
A second step towards equivalence, possibly in combination with high-intensity ventilation, is the use of filters, which can be HEPA filters of ESPs. When part of the air exhausted from the room is handled (heated, cooled, dehumidified, filtered) and recirculated back into the room after handling, filtering will be necessary in the return duct and should have been completed before the air is re-injected into the room. Whether a filter system with HEPA filters or an ESP is installed inside the room itself and should work in addition to the clean air ventilation, its effect will depend on the efficiency and the capacity (m³/h) of the filter system and the degree to which high-intensity ventilation is possible. At very high ventilation rates, the effect of the filter system might be limited. But if required, it could assist a less powerful ventilation system towards equivalence. This is shown in Fig. 5 , which is an extension of Fig. 4 in which – as an example – an ESP with a capacity of 3750 m³/h or 7500 m³/h and an efficiency of 50% is installed in the room, assuming perfect mixing, i.e. a uniform aerosol concentration in the room. Fig. 5 is based on the mass balance in the room:
| (4) |
Where QESP is the ESP flow rate and η the ESP efficiency. Under steady-state conditions, Eq. (4) can be used to extend Eq. (3) as follows:
| (5) |
Fig. 5.
Nomogram of number of persons per 10 m2 as a function of required ventilation rate per person, with the product of air change rate per hour (n) and room height (H) and the ESP characteristics as parameters (unit of nH is m/h).
Fig. 5 suggests that for N/A of about 10 dm³/s/person, installing an ESP with QESP = 7500 m³/h (QESP/A = 7.5 m/h) would allow doubling the occupancy from 1 to 2 person per 10 m2 while keeping the ventilation flow rate per person and thus the aerosol concentration constant. Note that Eq. (5) and Fig. 5 assume that the 50% ESP efficiency effectively applies to the potentially infectious aerosols generated inside the room, while also (non-infectious) aerosols can be brought from outside to inside by the ventilation system.
A third step towards equivalence could be the use of masks, although especially here more research and development is needed in view of masks that are both efficient and suitable for indoor physical exercise.
4. Discussion
An additional question in indoor sports centers is whether or not sweat can contribute to the transmission of infection. Ding et al. [72] found that SARS-CoV is present in sweat gland. There is potential for aerosolization of sweat, but the measures suggested to mitigate transmission from respiratory droplets and aerosols also apply to aerosolized sweat. If the virus is shed in sweat, probably the bigger concern is the contact route: people leaving behind sweat on machines, either high-touch areas of cardio machines or the seats and handles of weight machines and free weights/benches. This could be tackled by the guidelines in Ref. [29].
Mixing ventilation will not provide uniform aerosol concentrations in the entire volume of the room. This should be taken into account when implementing the certificate of equivalence. In view of this limitation, one could consider real-time monitoring of some environmental parameters at a few strategic locations in the sports center. These parameters could be aerosol concentrations or parameters that can be measured with less costly equipment and that could be used as indicators for aerosol concentrations, such as relative humidity and CO2 concentration. This real-time monitoring could also be used to control both the settings of the ventilation and the potentially present ESPs.
More research is needed on the production of respiratory droplets and aerosols during physical exercise but also concerning the increased and deeper inhalation of aerosols during such exercise. The latter could be studied with advanced computational fluid dynamics (CFD) models [[73], [74], [75], [76]].
For the three indoor sports categories covered in this technical note (cardio training; workout training with weights; non-contact group exercises in classes), if the outdoor space is available and if weather allows, these could partially be restarted outside. In such cases, it is advised to position the equipment and the participants as much as possible in rows perpendicular to the wind direction, so that they are not downwind and directly exposed to exhaled droplets and aerosols of other participants.
This technical note did not address contact sports. Physical distancing is clearly not an option here so the only viable route remaining might be testing and contact tracing followed by quarantining if necessary, as done in the German football competition that re-started on 16 May 2020.
5. Closing
COVID-19 is not the first and likely also not the last pandemic to rage around the globe and to disturb human life and activity world-wide. While in most countries, supermarkets have remained open, due to the COVID-19 situation, authorities have ordered many other shops, restaurants, bars, music theaters and indoor sports centers to be closed. As part of COVID-19 (semi)lock-down exit strategies, many government authorities are now (May-June 2020) allowing a gradual re-opening, where sometimes indoor sport centers are last in line to be permitted to re-open. This technical note discusses the challenges in safely re-opening these facilities and the measures already suggested by others to partly tackle these challenges. It also elaborates three potential additional measures: high-intensity building ventilation, filtering and face masks. These measures should be applied on top of the existing basic measures imposed by the government and the indoor sports school branche organizations. Of the additional measures, high-intensity building ventilation is considered as the most straightforward measure. However, large ventilation flow rates also require large energy consumption for heating, cooling and/or (de)humidifying of the clean intake air, which in turn might necessitate heat exchangers to be installed. Certainly if the capacity of the existing ventilation system is limited, direct filtering of the indoor air could be attempted by HEPA filters or electrostatic precipitators (ESPs). Finally, facial masks could be an option. Although in many countries the use of masks has been an issue of debate, governments are now implementing the mandatory use of surgical or home-made masks at an increasing pace. However, masks that are both efficient and suitable for physical exercise might require considerable additional research and development. Based on the adoption of some of these three additional measures, this technical note suggests the concept of a quantifiable certificate of equivalence that could allow indoor sports centers with such a certificate to re-open more safely and more rapidly. This technical note is also an attempt to stimulate increased preparedness of indoor sports centers that should allow them to remain open safely during potential next waves of SARS-CoV-2 as well as future pandemics. The complexity of SARS-CoV-2 and its behavior in the indoor environment indicates that fighting crises such as the COVID-19 situation and limiting economic damage requires increased collaboration and research by virologists, epidemiologists, microbiologists, aerosol scientists, building physicists, building services engineers and sports scientists.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Twan van Hooff is currently a postdoctoral fellow of the Research Foundation – Flanders (FWO) and acknowledges its financial support (project FWO 12R9718N).
References
- 1.European Centre for Disease Prevention and Control COVID-19 Situation update 19 May 2020, dataset collected 6:00-10:00 CET. 2020. https://www.ecdc.europa.eu/en/covid-19-pandemic Retrieved on.
- 2.Chan J., Yuan S., Kok K. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382: 1199-1207. [DOI] [PMC free article] [PubMed]
- 4.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke R.M., Midgley C.M., Dratch A. Active monitoring of persons exposed to patients with confirmed COVID-19 — United States, January–February 2020. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69(9):245–246. doi: 10.15585/mmwr.mm6909e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . World Health Organization; Geneva: 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16-24 February 2020.https://www.who.int/docs/default- source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf [Internet] Available from: [Google Scholar]
- 7.World Health Organization Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Sci. Brief. 2020;29 www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations March 2020. [Internet]. Geneva: World Health Organization; 2020 Available from: [Google Scholar]
- 8.Xie X., Li Y., Chwang A.T.Y. How far droplets can move in indoor environments - revisiting the Wells evaporation-falling curve. Indoor Air. 2007;17(3):211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- 9.Bourouiba L., Dehandschoewercker E., Bush J.W.M. Violent expiratory events: on coughing and sneezing. J. Fluid Mech. 2014;745:537–563. [Google Scholar]
- 10.Wie J., Li Y. Enhanced spread of expiratory droplets by turbulence in a cough jet. Build. Environ. 2015;93:86–96. [Google Scholar]
- 11.Liu Y., Ning Z., Chen Yu. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020 doi: 10.1038/s41586-020-2271-3. https://www.nature.com/articles/s41586-020-2271-3 in press. [DOI] [PubMed] [Google Scholar]
- 12.van Doremalen N., Morris D.H., Holbrook M.G. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadei M., Hopke P.K., Jonidi A., Shahsavani A. A letter about the airborne transmission of SARS-CoV-2 based on the current evidence. Aerosol Air Qual. Res. 2020;20:991. doi: 10.4209/aaqr.2020.04.0158. 914. [DOI] [Google Scholar]
- 15.Asadi S., Bouvier N., Wexler A.S., Ristenpart W.D. The coronavirus pandemic and aerosols: does COVID-19 transmit via expiratory particles? Aerosol. Sci. Technol. 2020;54(6):635–638. doi: 10.1080/02786826.2020.1749229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morawska L., Johnson G.R., Ristovski Z.D. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J. Aerosol Sci. 2009;40(3):256–269. [Google Scholar]
- 17.Johnson G.R., Morawska L. The mechanism of breath aerosol formation. J. Aerosol Med. Pulm. Drug Deliv. 2009;22(3):229–237. doi: 10.1089/jamp.2008.0720. [DOI] [PubMed] [Google Scholar]
- 18.Johnson G.R., Morawska L., Ristovski Z.D. Modality of human expired aerosol size distributions. J. Aerosol Sci. 2011;42(12):839–851. [Google Scholar]
- 19.Han Z.Y., Weng W.G., Huang Q.Y. Characterizations of particle size distribution of the droplets exhaled by sneeze. J. R. Soc. Interface. 2013;10(88):20130560. doi: 10.1098/rsif.2013.0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asadi S., Wexler A.S., Cappa C.D. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 2019;9(1):2348. doi: 10.1038/s41598-019-38808-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitttal R., Ni R., Seo J.H. The flow physics of COVID-19. J. Fluid Mech. 2020;894 Article nr. F2. [Google Scholar]
- 22.United Nations United Nations sustainable development Goals. https://www.un.org/sustainabledevelopment/sustainable-development-goals/
- 23.Van Der Merwe F.J.G. British and South African soccer on the western front during World War I. South Afr. J. Res. Sport, Phys. Educ. Recreat. 2013;35(2):197–209. [Google Scholar]
- 24.Waquet A. Sport in the trenches: the new deal for masculinity in France. Int. J. Hist. Sport. 2011;28(3–4):331–350. doi: 10.1080/09523367.2011.544861. [DOI] [PubMed] [Google Scholar]
- 25.Nyenhuis S.M., Greiwe J., Zeiger J.S. Exercise and Fitness in the age of social distancing during the COVID-19 Pandemic. J. Allergy Clin. Immunol.: In Pract. 2020 doi: 10.1016/j.jaip.2020.04.039. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen P., Mao L., Nassis G.P. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020;9(2):103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rubin G.J., Wessely S. The psychological effects of quarantining a city. Br. Med. J. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 28.NOC*NSF Protocol responsible physical exercise (in Dutch) 2020. https://nocnsf.nl/media/2669/nocnsf_protocol_verantwoord-sporten-v3.pdf Retrieved on.
- 29.NL Actief Protocol responsible physical exercise – Branche: fitness (in Dutch). Concept version. 2020. www.nlactief.nl Retrieved on.
- 30.Metselaar D. Indoor sports centers surprised by longer closure (in Dutch) 2020. https://www.nrc.nl/nieuws/2020/05/07/we-staan-in-hetzelfde-rijtje-als-de-seksclubs-a3999041 7 May 2020.
- 31.Almstrand A.C., Bake B., Ljungström E.L. Effect of airway opening on production of exhaled particles. J. Appl. Physiol. 2010;108:584–588. doi: 10.1152/japplphysiol.00873.2009. [DOI] [PubMed] [Google Scholar]
- 32.Jang S., Han S.H., Rhee J.Y. Cluster of coronavirus disease associated with fitness dance classes, South Korea. Emerg. Infect. Dis. 2020;268 doi: 10.3201/eid2608.200633. Research Letter. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ye F., Xu S., Rong Z. Delivery of infection from asymptomatic carriers of COVID-19 in a familial cluster. Int. J. Infect. Dis. 2020;94:133–138. doi: 10.1016/j.ijid.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rothe C., Schunk M., Sothmann P. Transmission of 2019-ncov infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.AIVC . International Energy Agency; 2020. Air Infiltration and Ventilation Centre.https://www.aivc.org/resources/faqs/what-ventilation Retrieved on 11 May 2020: [Google Scholar]
- 36.Etheridge D., Sandberg M. Wiley; 1996. Building Ventilation: Theory and Measurements. -13: 978-0471960874. [Google Scholar]
- 37.Awbi H. Spon Press; 2003. Ventilation of Buildings. [Google Scholar]
- 38.Chen Q. Ventilation performance prediction for buildings: a method overview and recent applications. Build. Environ. 2009;44(4):848–858. [Google Scholar]
- 39.Blocken B. 50 years of computational wind engineering: past, present and future. J. Wind Eng. Ind. Aerod. 2014;129:69–102. [Google Scholar]
- 40.Nielsen P.V. Technical University of Denmark; Copenhagen: 1976. Flow in Air Conditioned Rooms. English Translation and Revision of PhD Thesis. [Google Scholar]
- 41.Nielsen P.V. Computational fluid dynamics and room air movement. Indoor Air. 2004;14(Suppl. 7):134–143. doi: 10.1111/j.1600-0668.2004.00282.x. [DOI] [PubMed] [Google Scholar]
- 42.Chen Q. Prediction of room air motion by Reynolds-stress models. Build. Environ. 1996;31:233–244. [Google Scholar]
- 43.Chen Q., Chao N.T. Comparing turbulence models for buoyant plume and displacement ventilation simulation. Indoor Built Environ. 1997;6:140–149. [Google Scholar]
- 44.Karava P., Stathopoulos T., Athienitis A.K. Airflow assessment in cross-ventilated buildings with operable facade elements. Build. Environ. 2011;46:266–279. [Google Scholar]
- 45.Kato S., Murakami S., Mochida A., Akabayashi S., Tominaga Y. Velocity-pressure field of cross-ventilation with open windows analyzed by wind tunnel and numerical simulation. J. Wind Eng. Ind. Aerod. 1992;44:2575–2586. [Google Scholar]
- 46.van Hooff T., Blocken B. Coupled urban wind flow and indoor natural ventilation modelling on a high-resolution grid: a case study for the Amsterdam ArenA stadium. Environ. Model. Software. 2010;25(1):51–65. [Google Scholar]
- 47.Ramponi R., Blocken B. CFD simulation of cross-ventilation for a generic isolated building: impact of computational parameters. Build. Environ. 2012;53:34–48. [Google Scholar]
- 48.Blocken B. Computational Fluid Dynamics for Urban Physics: importance, scales, possibilities, limitations and ten tips and tricks towards accurate and reliable simulations. Build. Environ. 2015;91:219–245. [Google Scholar]
- 49.Craven B.A., Settles G.S. A computational and experimental investigation of the human thermal plume. J. Fluids Eng. Trans. ASME. 2006;128(6):1251–1258. [Google Scholar]
- 50.Li Y., Leung G.M., Tang J.W. Role of ventilation in airborne transmission of infectious agents in the built environment – a multidisciplinary systematic review. Indoor Air. 2007;17:2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 51.REHVA How to operate and use building services in order to prevent the spread of the coronavirus disease (COVID-19) virus (SARS-CoV-2) in workplaces. COVID-19 Guidance Document, 3 April 2020aa. 2020. https://www.rehva.eu/fileadmin/user_upload/REHVA_COVID-19_guidance_document_ver2_20200403_1.pdf
- 52.Ai Z.T., Melikov A.K. Airborne spread of expiratory droplet nuclei between the occupants of indoor environments: a review. Indoor Air. 2018;28:500–524. doi: 10.1111/ina.12465. [DOI] [PubMed] [Google Scholar]
- 53.Ministerie van Binnenlandse Zaken en Koninkrijksrelaties Building code. Bouwbesluit online (in Dutch) 2012. https://rijksoverheid.bouwbesluit.com/Inhoud/docs/wet/bb2012/hfd3 Retrieved on 11 May 2020.
- 54.Ariëns J.P.E., Joosten T.A., Schriemer W. NOC*NSF, Arko Sports Media BV; 2008. Guidebook Sports Accommodations (In Dutch). Handboek Sportaccommodaties. ISA Sport. [Google Scholar]
- 55.Stichting Onbeperkt Sportief . Richtlijnen Toegankelijkheid Indoor Sportaccommodaties; 2014. Guidelines for Access Indoor Sports Accommodations (In Dutch) [Google Scholar]
- 56.ASHRAE Pandemic COVID-19 and airborne transmission. Environmental health committee (EHC) emerging issue brief. 2020. https://www.ashrae.org/file%20library/technical%20resources/covid-19/eiband-airbornetransmission.pdf Retrieved on.
- 57.ASHRAE Ventilation for acceptable indoor air quality. ANSI/ASHRAE Standard. 2019;62:1. 2019. [Google Scholar]
- 58.IUPAC . (the "Gold Book") (1997). Online Corrected Version: (2006–) "electrostatic Precipitator". second ed. 2006. Compendium of chemical terminology. [DOI] [Google Scholar]
- 59.Vervoort R.P.M., van Hooff T., Blocken B. Reduction of particulate matter concentrations by local removal in a building courtyard: case study for the Delhi American Embassy School. Sci. Total Environ. 2019;686:657–680. doi: 10.1016/j.scitotenv.2019.05.154. [DOI] [PubMed] [Google Scholar]
- 60.Chen C.C., Willeke K. Aerosol penetration through surgical masks. Am. J. Infect. Contr. 1992;20:177–184. doi: 10.1016/s0196-6553(05)80143-9. [DOI] [PubMed] [Google Scholar]
- 61.He X., Reponen T., McKay R.T. Effect of particle size on the performance of an N95 filtering facepiece respirator and a surgical mask at various breathing conditions. Aerosol. Sci. Technol. 2013;47(11):1180–1187. doi: 10.1080/02786826.2013.829209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Van der Sande M., Teunis P., Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PloS One. 2008;3(7) doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhai J. Facial mask: a necessity to beat COVID-19: the review of an air quality and ventilation expert. Build. Environ. 2020;175:106827. doi: 10.1016/j.buildenv.2020.106827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dwyer C., Aubrey A. CDC now recommends Americans consider wearing cloth face coverings in public. 2020. https://www.npr.org/sections/coronavirus-live-updates/2020/04/03/826219824/president-trump-says-cdc-now-recommends-americans-wear-cloth-masksin- public Available at:
- 65.Elegant N.X. Coronavirus outbreak changes US's mind on everyone wearing face masks. Fortune. 2020 https://fortune.com/2020/04/03/coronavirus-face-mask-cdc/ Available at: [Google Scholar]
- 66.Feng S, Shen C, Xia N, et al Rational use of face masks in the covid-19 pandemic. Lancet Respir. Med. Available at: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30134-X/fulltext. [DOI] [PMC free article] [PubMed]
- 67.The Bulletin Coronavirus in Belgium: what are the rules on wearing masks? 9 May 2020. 2020. https://www.thebulletin.be/coronavirus-belgium-should-we-be-wearing-masks-0
- 68.nl DutchNews. Dutch start easing coronavirus restrictions, face masks a must on public transport. 6 May 2020. 2020. https://www.dutchnews.nl/news/2020/05/dutch-start-easing-coronavirus-restrictions-face-masks-a-must-on-public-transport/
- 69.FDA Personal protective equipment for infection control, N95 respirators and surgical masks (face masks) 2020. www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks Retreived on 12 May 2020.
- 70.Howard J., Huang A., Li Z. Face masks against COVID-19: an evidence review. Preprints. 2020;2020:2020040203. doi: 10.20944/preprints202004.0203.v1. [DOI] [Google Scholar]
- 71.Wong C.K.M., Yip B.H.K., Mercer S. Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BCM Family Pract. 2013;14:200. doi: 10.1186/1471-2296-14-200. PMID: 24364989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ding Y., He L., Zhang Q. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J. Pathol. 2004;203(2):622–630. doi: 10.1002/path.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tawhai M.H., Hunter P.J., Tschirren J. CT-based geometry analysis and finite element models of the human and ovine bronchial tree. J. Appl. Physiol. 2004;97(6):2310–2321. doi: 10.1152/japplphysiol.00520.2004. [DOI] [PubMed] [Google Scholar]
- 74.Yin Y., Choi J., Hoffman E.A. A multiscale MDCT image-based breathing lung model with time-varying regional ventilation. J. Comput. Phys. 2013;244:168–192. doi: 10.1016/j.jcp.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yin Y., Choi J., Hoffman E.A. Simulation of pulmonary air flow with a subject-specific boundary condition. J. Biomech. 2010;43(11):2159–2163. doi: 10.1016/j.jbiomech.2010.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Burrowes K.S., Doel T., Brightling C. Computational modeling of the obstructive lung diseases asthma and COPD. J. Transl. Med. 2014;12:S5. doi: 10.1186/1479-5876-12-S2-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]