Sir,
In Singapore, a small city-state of 5.7 million population, early detection and contact tracing for coronavirus disease 2019 (COVID-19) allowed for rapid isolation of cases with prompt containment of spread. With this strategy, the early pace was slow and the milestone of 1000 infections was crossed more than two months after, with the majority due to importations. The epidemic's trajectory, however, surged thereafter with outbreaks noted in foreign worker dormitories. At the time of writing, 15,207 (86%) of the 17,548 local COVID-19 cases have arisen from dormitory residents [1].
Dormitory A is a large privately owned dormitory that can accommodate 13,000 inhabitants, in rooms of 12 residents across 13 blocks. With the high number of COVID-19 cases arising from dormitory A, it was gazetted by law as an isolation area on April 5th [2]. We describe results of the outbreak investigation and clinical evaluation in dormitory A.
This study is a review of investigation results from April 11th to April 19th, 2020. Residents in dormitory A who had symptoms of acute respiratory infection were assessed for COVID-19. Symptoms and clinical signs were collected, with fever defined as ≥37.6°C. Oxygen saturations and heart rate were measured using portable pulse oximeters. Nasopharyngeal specimens were sent for polymerase chain reaction (PCR) testing for severe acute respiratory syndrome coronavirus-2.
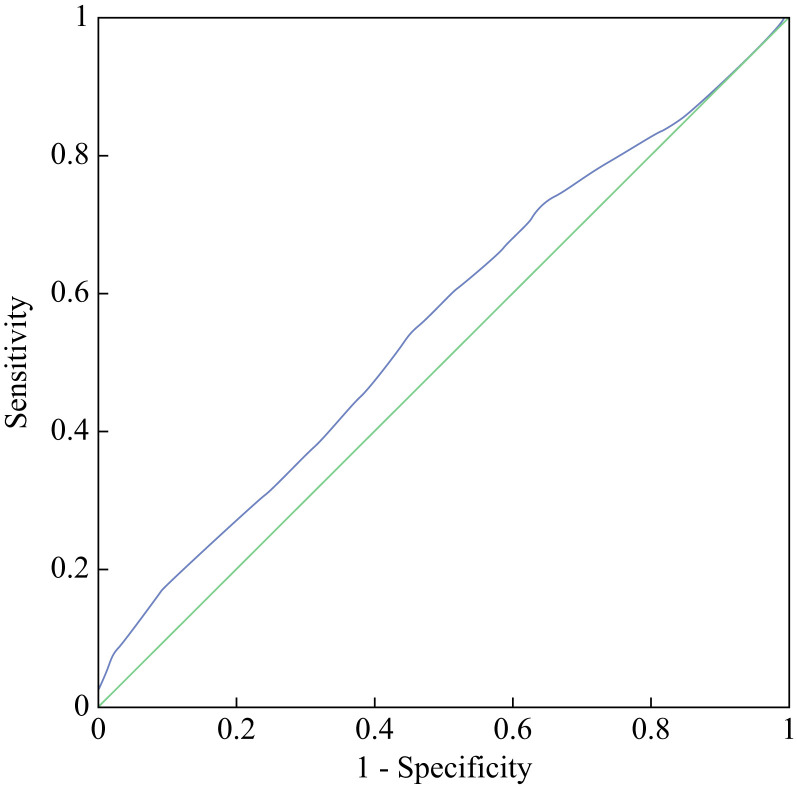
Clinical parameters were stratified to determine sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) according to PCR results. Receiver operating characteristic (ROC) curves were drawn to determine discrimination threshold.
In all, 1832 out of 5977 foreign workers were symptomatic. Of these, 1264 (69%) were found to be positive for COVID-19. COVID-19-positive and -negative groups had similar median age (33 years, P = 0.71) and heart rate (108 vs 107 bpm, P = 0.17). COVID-19-positive foreign workers had slightly higher median temperatures (37.8 vs 37.7, P < 0.01).
PPV was highest for those with body temperature ≥38.5°C (89.0%) (Table I , Figure 1 ) and oxygen saturations of <95% (78.9%). Heart rate of ≥130 bpm was found to have a specificity of 88.9%. After plotting ROC curves for individual parameters, the areas under the curves were only between 0.5 and 0.6, indicating that vital signs were poorly discriminatory for COVID-19 status.
Table I.
Co-relating body temperature with COVID-19 status
| Temperature (°C) | COVID-19+ | COVID-19– | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| ≥37.6 | 848 | 325 | 67.1 | 40.7 | 72.3 | 34.9 |
| <37.6 | 416 | 223 | ||||
| ≥38.5 | 97 | 12 | 7.7 | 97.8 | 89.0 | 31.5 |
| <38.5 | 1167 | 536 |
COVID-19, coronavirus disease 2019; PPV, positive predictive value; NPV, negative predictive value.
Figure 1.
Receiver operating characteristic curve, co-relating body temperature with COVID-19 status. Area under the curve: 0.558 (95% confidence interval: 0.529–0.586). Diagonal segments are produced by ties.
Whereas 21% of the cohort (of 5977 foreign workers) were found to be positive for COVID-19, the true prevalence is likely higher if asymptomatic individuals are also assessed, with incidence up to 36% in other closed environments [3]. In such environments, presymptomatic transmission risks are high [4]. In our study, we had set the cut-offs of ≥37.6°C for fever definition in view of higher risks of viral transmission in this population. Nonetheless, this cohort is generally young (mean age: 33 years) and fit, with likely lower mortality risks as compared to residents in other closed-living environments such as nursing homes [5].
Our screening was performed by a primary care team deployed without chest X-ray or point-of-care testing. Whereas clinical features alone may have a low discriminatory value, additional testing capabilities in the field such as mobile chest X-ray perhaps may improve diagnostic accuracy. We also acknowledge that a single negative test does not exclude COVID-19 infections. It may thus have to be assumed that all symptomatic individuals housed in the affected dormitory should be suspected cases.
The strategy for containment in closed-living environments therefore would be to isolate symptomatic individuals, and to establish public health measures for social distancing. Infected individuals with higher risk for deterioration – for example above the age of 50 years, medical comorbidities, or with low oxygen saturation on diagnosis – may require hospital admission. Relocating higher-risk individuals even without infection may also be possible to reduce risk of disease transmission in the closed-living environment. In large closed-living environments these strategies are needed to contain the spread of disease.
Acknowledgements
Ms H.-C. Tan helped to validate the statistics and assisted in plotting the ROC curves. Ms Q.-X. Chua contributed to data collection.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Ministry of Health . 2020. COVID-19 local situation report archive – situation report.https://www.moh.gov.sg/docs/librariesprovider5/2019-ncov/situation-report---02-may-2020.pdf Available at: [last accessed May 2020] [Google Scholar]
- 2.Ministry of Manpower Comprehensive Approach to take care of the well-being of foreign workers living in dormitories. 2020. https://www.mom.gov.sg/newsroom/press-releases/2020/0501-comprehensive-approach-to-take-care-of-the-well-being-of-foreign-workers-living-in-dormitories Available at: [last accessed May 2020] [Google Scholar]
- 3.Baggett T.P., Keyes H., Sporn N., Gaeta J.M. Prevalence of SARS-CoV-2 infection of residents of a large homeless shelter in Boston. JAMA. 2020 doi: 10.1001/jama.2020.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei W.E., Li Z.B., Chiew C.J., Yong S.E., Toh M.P., Lee V.J. Presymptomatic transmission of SARS-CoV-2 – Singapore, January 23–March 16, 2020. March 2020. Morb Mort Wkly Rep. 2020;69:411–415. doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Comas-Herrera A., Zalakain J., Litwin C., Hsu A.T., Fernandez-Plotka J.-L. 2020. Mortality associated with COVID-19 outbreaks in care homes: early international evidence: international long term care policy network.https://ltccovid.org/2020/04/12/mortality-associated-with-covid-19-outbreaks-in-care-homes-early-international-evidence/ Available at: [last accessed May 2020] [Google Scholar]