Numerous reports in traditional https://www.theguardian.com/world/2020/mar/24/britons-saying-final-goodbyes-to-dying-relatives-by-videolink-covid-19, social media and academic forums https://www.nejm.org/doi/full/10.1056/NEJMp2007781 highlight the distressing plight of families unable to say good bye to their loved ones dying in intensive care with severe COVID-19 around the world. As in many countries, families in the United Kingdom (UK) are currently restricted from in-person visiting due to the risk to themselves staff and the public, as well as limited supply of personal protective equipment.
Visiting restrictions are causing moral injury to intensive care staff for whom in-person emotional support of family members throughout their loved one’s critical illness is integral to professional practice. This support includes facilitating ‘a good death’ with end of life care that enables the family to be present if preferred and minimises the risk of complicated grief. Family absence from the intensive care unit (ICU) presents a barrier to formal and informal updates to families on their loved one’s condition, as well as discussion of goals of care that reflect the patient’s own wishes.
Restricted family visiting also impacts patients both within and beyond intensive care in the recovery phase following severe COVID-19 infection. Now conscious and aware of their surroundings, but without family and friends to support them, patients are experiencing exceptional social isolation further contributing to acute stress, anxiety and depression. These factors impede weaning from mechanical ventilation and motivation to participate in physiotherapy and rehabilitation.
Communication via various video conferencing methods is being used across the globe as a method to enable virtual family presence at the bedside in intensive care, during end of life care and throughout recovery. Unfortunately, privacy and functionality considerations limit the utility of commercially available video communication tools for when used in the context of enabling a virtual visit and video communication with families of critically ill unconscious patients. Videoconferencing tools such as Whatsapp, Facetime and Skype require use of a personal login or phone number and lack the ability to block call origin. This has led to situations where clinical staff have used personal devices, particularly during emergent and end of life situations, thus inadvertently providing families with a contact number that is presumed to belong to the ICU. Subsequent calls from family members have caused distress to both parties. Another important limitation to commercially available videoconferencing solutions particular to their use in a clinical setting is that there is inability to maintain a digitally secure list of patient and their family contacts easily accessible to the clinical team. This means overstretched clinical staff need to locate, confirm and re-enter phone numbers or email addresses each time a video call is made.
Life Lines is a philanthropic COVID-19 response project hosted by King’s Health Partners (https://www.kingshealthpartners.org/our-work/lifelines) that is providing intensive care units in the UK with a minimum of two electronic tablet devices enabled with 4G connectivity and aTouchAway™. The aTouchAway™ App, created by the Canadian company Aetonix, is a digitally secure, unidirectional communication platform specifically adapted to enable virtual family visits. The video calling function is simple, intuitive and high quality. 4G connectivity means that the Life Lines tablet devices are not reliant on connection to hospital Wifi providing enhanced connectivity. The aTouchAway™ cloud-based directory allows each institution to build a digitally secure patient list with attributed family contacts within the App accessible by multiple tablet devices across an institution.
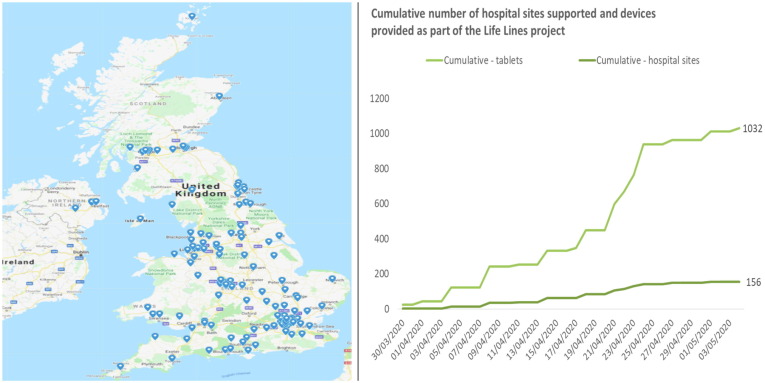
The Life Lines project began on 15th March 2020. As of 6th May 2020 Life Lines has delivered over 1000 tablets to over 150 hospitals throughout the UK (Fig. 1 ) including the Nightingale temporary hospitals created as a COVID-19 response with over 65,000 calls made. Life Lines will continue to supply electronic tablets not only to ICUs but other clinical areas of need such as palliative care thereby enabling thousands of families to experience a digitally secure virtual family visit in these unprecedented times. The rapid implementation and uptake of this technology and understanding of its use as a clinical communication tool has been spurred by the COVID-19 crisis. However, there is also an opportunity to integrate lessons learned from this innovation to enable virtual family visiting as routine clinical care in ICUs not only in the UK but internationally as we learn about the potential applications and benefits of virtual family visiting.
Fig. 1.
Hospitals with electronic devices provided as part of the Life Lines project to May 6th 2020.
Funding of Life Lines
Life Lines has been enabled through generous Covid19 response donations from the Gatsby Foundation and True Colours Trust as well as in kind support from mobile phone and tech companies, specifically British Telecom and Google.
Contributor Information
The Life Lines Team comprising: