Abstract
BACKGROUND
Persons with mental disorders are at a higher risk than the general population for the subsequent development of certain medical conditions.
METHODS
We used a population-based cohort from Danish national registries that included data on more than 5.9 million persons born in Denmark from 1900 through 2015 and followed them from 2000 through 2016, for a total of 83.9 million person-years. We assessed 10 broad types of mental disorders and 9 broad categories of medical conditions (which encompassed 31 specific conditions). We used Cox regression models to calculate overall hazard ratios and time-dependent hazard ratios for pairs of mental disorders and medical conditions, after adjustment for age, sex, calendar time, and previous mental disorders. Absolute risks were estimated with the use of competing-risks survival analyses.
RESULTS
A total of 698,874 of 5,940,299 persons (11.8%) were identified as having a mental disorder. The median age of the total population was 32.1 years at entry into the cohort and 48.7 years at the time of the last follow-up. Persons with a mental disorder had a higher risk than those without such disorders with respect to 76 of 90 pairs of mental disorders and medical conditions. The median hazard ratio for an association between a mental disorder and a medical condition was 1.37. The lowest hazard ratio was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval [CI], 0.80 to 0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11 to 4.22). Several specific pairs showed a reduced risk (e.g., schizophrenia and musculoskeletal conditions). Risks varied according to the time since the diagnosis of a mental disorder. The absolute risk of a medical condition within 15 years after a mental disorder was diagnosed varied from 0.6% for a urogenital condition among persons with a developmental disorder to 54.1% for a circulatory disorder among those with an organic mental disorder.
CONCLUSIONS
Most mental disorders were associated with an increased risk of a subsequent medical condition; hazard ratios ranged from 0.82 to 3.62 and varied according to the time since the diagnosis of the mental disorder. (Funded by the Danish National Research Foundation and others; COMO-GMC ClinicalTrials.gov number, NCT03847753.)
PERSONS WITH MENTAL DISORDERS ARE at increased risk for other types of mental disorders1 and for a range of general medical conditions.2,3 These medical conditions contribute to a decreased quality of life, increased health care utilization, and premature death in many persons with mental disorders.4–8
The study of the relationship between mental disorders and medical conditions has often been restricted to particular pairs or a small set of mental disorders and medical conditions. A comprehensive assessment could allow comparisons across a spectrum of coexisting mental disorders and medical conditions. Data regarding both relative and absolute risks of various medical conditions after a diagnosis of a mental disorder over particular time periods — for example, the proportion of persons with depression at the age of 30 years in whom circulatory disorders may develop during the subsequent 5, 10, or 15 years — could help clinicians and health care planners identify the primary-prevention needs of their patients. Because some medical conditions are common in the general population, data regarding persons with specific medical conditions that are categorized according to the presence or absence of specific mental disorders may also be helpful.
The aim of this study, called Exploring the Comorbidity Between Mental Disorders and General Medical Conditions (COMO-GMC), was to acquire a comprehensive compilation of associations between mental disorders and subsequent medical conditions. We used Danish nationwide registries to provide temporally ordered, age-specific, and sex-specific pairwise estimates of risks of a range of mental disorders and subsequent medical conditions. We explored whether the associations between the pairs of mental disorders and medical conditions varied according to the time since the diagnosis of the mental disorder and compared age-specific and sex-specific measures of absolute risk of medical conditions with reference estimates in persons without mental disorders.
METHODS
STUDY POPULATION AND ASCERTAINMENT OF DISORDERS
We adopted the analysis in the current study from one performed by our group on the coexistence of two or more types of mental disorders.1 The population-based cohort study included all 5,940,299 persons born in Denmark from 1900 through 2015 who were residing in the country at the start of the follow-up period (January 1, 2000, or their first birthday, whichever occurred later), as identified in the Danish Civil Registration System.9 Included in the database were 2,958,035 males and 2,982,264 females.
We obtained information on mental disorders from the Danish Psychiatric Central Research Register,10 which contains details of diagnoses. Diagnosis dates were defined as the discharge date of first contact (inpatient, outpatient, or emergency visit). To keep the number of analyses tractable and aid comparability with previous Danish register-based studies,1,11 we focused on 10 broad types of mental disorders, based on the International Classification of Diseases, 10th Revision (ICD-10), Diagnostic Research Criteria subchapter F categories (F00–F09, F10–F19, etc.) and corresponding diagnoses in the ICD-8. Details of the specific diagnoses within each group of mental disorders and their short labels are presented in Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org.
We obtained information about medical conditions going back to 1995 (the year prescription data became complete) using criteria that were based on Danish research on coexisting conditions.12 These criteria focus on 31 medical conditions, within nine broad categories: circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, and neurologic conditions and cancer. Persons with medical conditions were identified by combining data from three sources: diagnoses made during inpatient admissions and outpatient and emergency visits from the Danish National Patient Registry,13 prescriptions for disease-specific medications in the Danish National Prescription Registry,14 and diagnoses recorded as causes of death in the Danish Register of Causes of Death.15 The diagnoses (ICD-10 codes) and drugs (Anatomical Therapeutic Chemical classification system codes) that were included in the definition of each medical condition are provided in Table S2. The diagnosis date of the medical condition of interest was the date of first hospital diagnosis, the date of the relevant repeat prescription, or the date of death from the medical condition, whichever occurred first.
STUDY DESIGN
We estimated associations between 90 pairs of mental disorders and broad categories of medical conditions, plus 310 pairs of mental disorders and specific medical conditions. Among persons in whom a mental disorder had been diagnosed during the period from 1969 (when data on psychiatric health care contacts were first available) through 2016, we estimated the risk of a medical-condition category or a particular medical condition during follow-up. The frequency of each medical condition in the study is shown in Table S3. The Danish Data Protection Agency and the Danish Health Data Authority approved this study.
STATISTICAL ANALYSIS
We compared the frequency of a diagnosis of a medical condition (in a broad or specific category) according to the presence or absence of a diagnosed mental disorder using Cox proportional-hazards models with age as the underlying time scale. For these analyses, we used two models. Model A examined the association between the diagnosis of a mental disorder (the mental disorder of interest) and the subsequent development of a medical condition (the medical condition of interest), after adjustment for sex and birth date (with the latter also automatically providing an adjustment for calendar time), in combination with underlying age in the models. Model B included additional time-varying adjustments for other mental disorders diagnosed before the mental disorder of interest. When the rates of a medical condition over time among persons with a mental disorder were not proportional to those among persons without a mental disorder, we interpreted the estimates as an average hazard ratio over the entire follow-up period.16 In addition, we investigated whether the association depended on the time since the mental disorder had been diagnosed (reported as time-dependent hazard ratios) by analyzing seven periods after the diagnosis (0 to 6 months, >6 to 12 months, >1 to 2 years, >2 to 5 years, >5 to 10 years, >10 to 15 years, or >15 years).
Among persons with a mental disorder, we estimated the cumulative incidence of a diagnosis of a medical condition, using competing-risks survival analyses based on the risk of a medical condition, death, or emigration. To evaluate the cumulative incidence of a medical condition according to the presence or absence of a mental disorder, a matched reference group was generated for each mental disorder. For every index person with the mental disorder, up to five age-matched and sex-matched persons who had not received a diagnosis of the relevant mental disorder at or before the age at which the index diagnosis occurred were randomly selected from the entire Danish population, as described in the Methods section in the Supplementary Appendix.
To simplify the presentation of results, we report nine broad categories of medical conditions; however, more detailed results for the nine broad categories of medical conditions and 31 specific medical conditions are provided in the Supplementary Appendix. In addition, estimates can be viewed at http://nbepi.com/gmc.
RESULTS
POPULATION
Among the 5,940,299 persons who were included in the database of Danish residents, 698,874 persons (11.8%) had received a diagnosis of a mental disorder and 5,241,425 (88.2%) had not. The cohort was followed for 83.9 million person-years; the median age was 32.1 years at the time of entry to the cohort and 48.7 years at the last follow-up. During this time, 882,728 persons died and 85,347 emigrated. Table S3 provides the numbers of prevalent cases identified from 1995 through 1999, the population defined for the purposes of the study as being at risk at the start of follow-up, and the number of incident cases identified for each medical condition. Baseline characteristics of the two cohorts are provided in Table S4.
Pairwise associations and absolute risks for all pairs of mental disorders and medical conditions are provided in Figures S1 through S142. The main findings are described below, with a focus on the associations between mental disorders and the nine broad categories of medical conditions. Associations between three specific pairs of mental disorders and medical conditions are presented as examples in the Results section in the Supplementary Appendix.
RELATIVE RISK OF SUBSEQUENT MEDICAL CONDITION
Estimates of hazard ratios for the 9 categories of medical conditions among persons with each of the 10 mental disorders for both model A and model B are shown in Figure 1. After adjustment for sex, age, calendar time, and previous coexisting mental disorders (model B), the median hazard ratio for a subsequent medical condition in a person with a mental disorder was 1.37 (mean, 1.44; range, 0.82 to 3.62; interquartile range, 1.20 to 1.55). The lowest hazard ratio of 0.82 was for the diagnosis of an organic mental disorder and a subsequent cancer (95% confidence interval [CI], 0.80 to 0.84), and the highest was 3.62 for the diagnosis of an eating disorder and a subsequent urogenital condition (95% CI, 3.11 to 4.22). With this model, 76 of 90 pairs of mental disorders and medical conditions had hazard ratios greater than 1 and 95% confidence intervals that did not include 1. In 5 pairs, model B identified a reduced risk, including a hazard ratio of 0.87 (95% CI, 0.84 to 0.91) for schizophrenia and subsequent musculoskeletal conditions. Among persons with a mental disorder, the median hazard ratio for the 31 specific medical conditions was 1.35 (mean, 1.53; range, 0.65 to 4.14; interquartile range, 1.12 to 1.66). Estimates from pairwise comparisons are shown in Figures S3 through S12.
Figure 1. Risk of a Medical Condition after the Diagnosis of a Mental Disorder, According to Category.
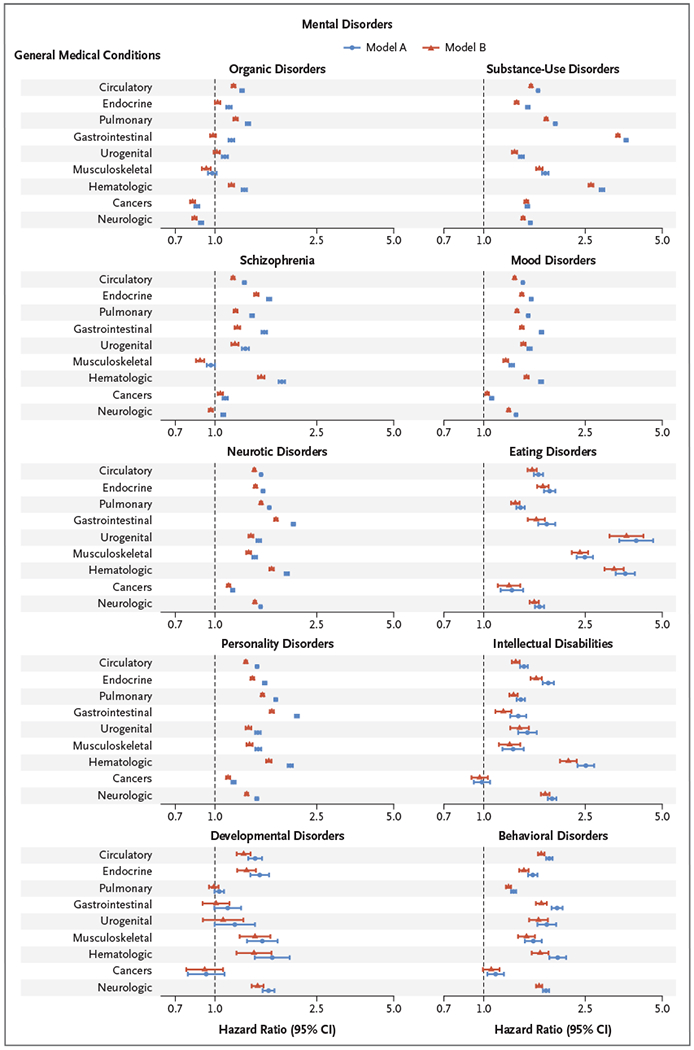
Each panel shows the pairwise risk of a medical condition (listed at the left of the graphs) after the diagnosis of a mental disorder (indicated at the top of each panel). Estimates were calculated with the use of Cox proportional-hazards models with age as the underlying time scale, after adjustment for sex and calendar time (model A) and after further adjustment for other mental disorders that had an onset before the mental disorder under study (model B). The line of unity is shown as a dashed line in each plot. Hazard ratios are shown on a log scale. I bars indicate confidence intervals.
TIME-DEPENDENT RELATIVE RISKS
Time-dependent hazard ratios for receiving a diagnosis within each category of medical condition, depending on previous diagnosis and time since the first diagnosis of a mood disorder, are shown in Figure 2. Temporal patterns for other pairwise comparisons are shown in Figures S23 through S42. For some pairwise comparisons, hazard ratios were high soon after the diagnosis of the mental disorder and declined over subsequent years but still remained elevated (e.g., for mood disorders and neurologic conditions). A steeper decrease was observed for a number of pairs for which hazard ratios were higher in the first year after a diagnosis of a mental disorder but then decreased rapidly (e.g., mood disorders and cancers). Time-dependent hazard ratios for the 31 specific medical conditions are shown in Figures S43 through S62.
Figure 2. Risk of a Medical Condition after the Diagnosis of a Mood Disorder, According to the Timing of the Diagnosis.
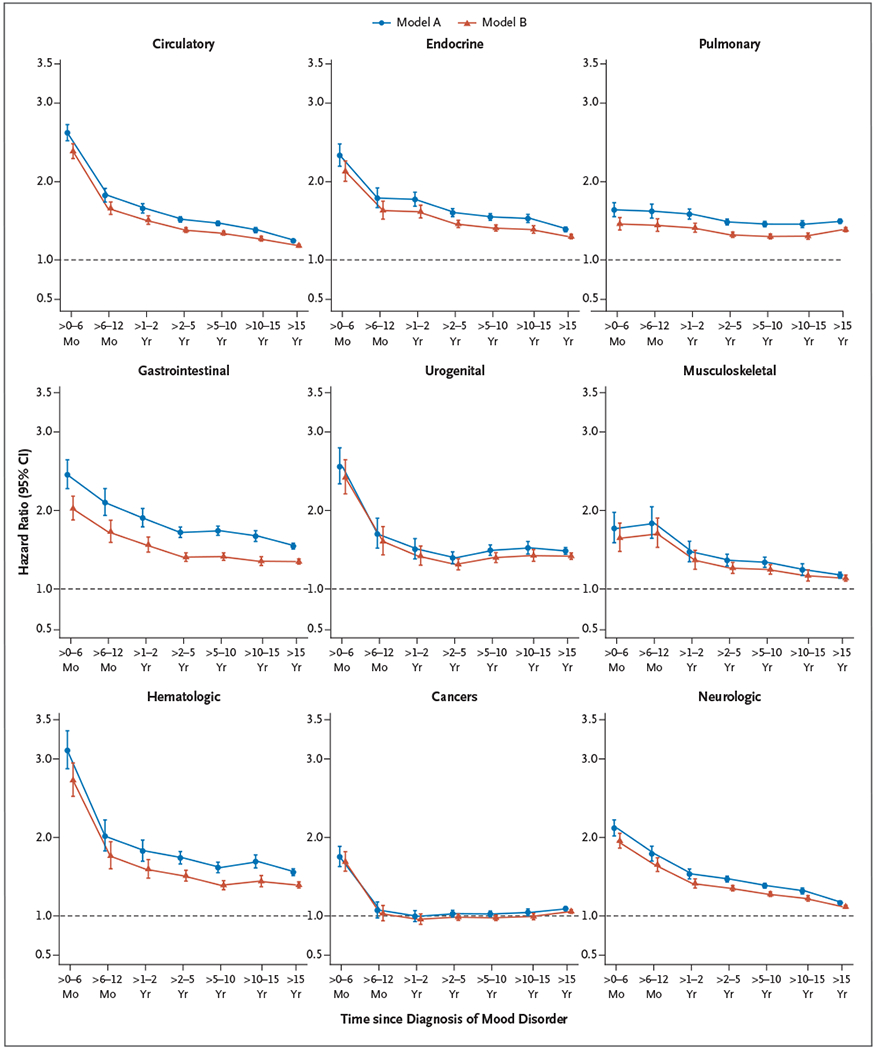
Each panel shows the time-dependent hazard ratios for a medical condition after the diagnosis of a mood disorder, according to two models. Estimates were obtained with the use of Cox proportional-hazards models with age as the underlying time scale, after adjustment for sex and calendar time (model A) and after further adjustment for other mental disorders that had an onset before the mental disorder under study (model B). The line of unity is shown as a dashed line in each plot. The horizontal axes show the time period since the first diagnosis of a mood disorder. All other pairwise comparisons between mental disorders and medical conditions are shown in Figures S23 through S62.
ABSOLUTE RISK OF SUBSEQUENT MEDICAL CONDITION
Among persons with a mood disorder, the absolute risk of a subsequent medical condition according to sex and the time since the mental disorder had been diagnosed is shown in Figure 3A. One of the highest cumulative incidences within 15 years after the diagnosis of a mental disorder was for mood disorders and circulatory conditions (40.9%; 95% CI, 40.5 to 41.3). For the matched reference group without a mood disorder, the cumulative incidence at 15 years was 32.6% (95% CI, 32.4 to 32.8). The absolute risk of a circulatory condition according to the age at the time of diagnosis of a mood disorder is shown in Figure 3B.
Figure 3. Risk of a Medical Condition after the Diagnosis of a Mood Disorder, According to Sex and the Time since the Diagnosis.
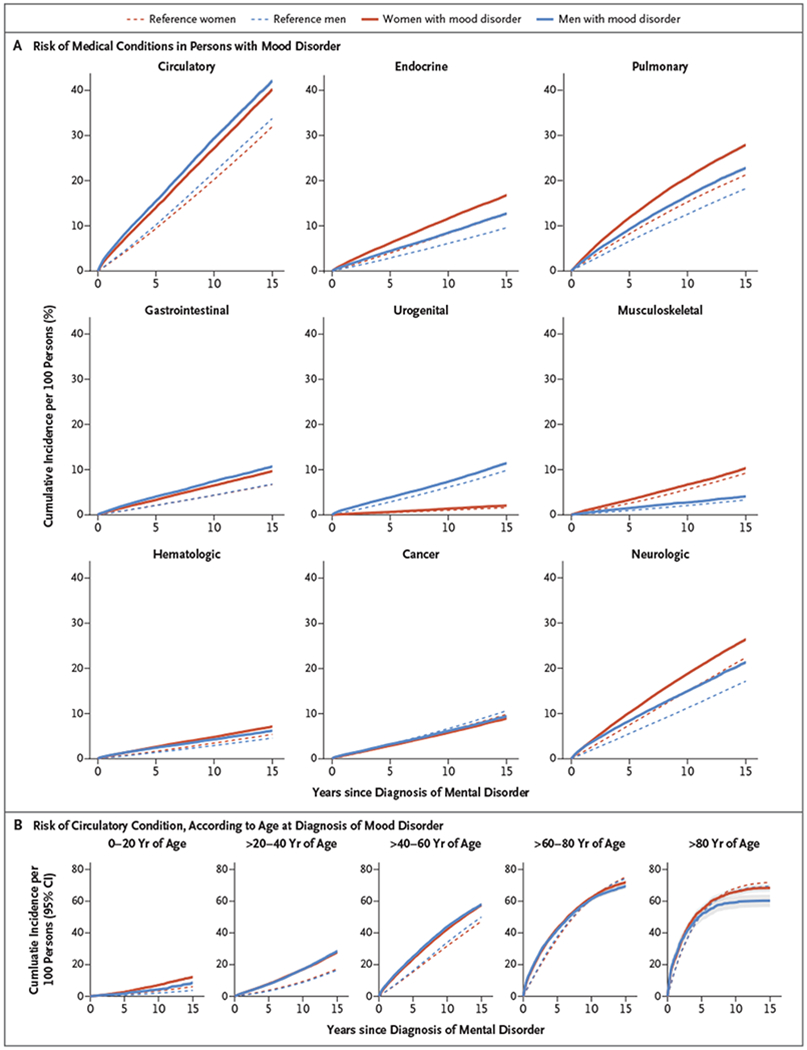
Shown is the risk (as measured by cumulative incidence per 100 persons) of a medical condition after the diagnosis of a mood disorder, according to sex and the category of medical condition. Panel A shows the estimates among all the persons in the study, according to the time since the diagnosis of the mood disorder. Panel B shows the risk of a circulatory condition according to the age at the time of the diagnosis of a mood disorder, with the time since the diagnosis of the mood disorder shown on the horizontal axes. The 95% confidence intervals (indicated by shaded gray areas around the curves) are so small that they are obscured by the estimate curves in Panel A and are visible only in the graph at the far right in Panel B. The absolute risks of all other pairs of mental disorders and medical conditions are shown in Figures S63 through S142.
The cumulative incidences according to age and sex for every pair of mental disorders and medical conditions are provided in Figures S63 through S142. The temporal patterns were similar among almost all pairs. In competing-risk analyses, the cumulative incidences of diagnoses of medical conditions within 15 years were higher among persons who had received a diagnosis of a mental disorder at a younger age. In older persons, the cumulative incidence of selected medical conditions was often lower among those in whom a mental disorder had been first diagnosed after the age of 60 years than among those in the reference group.
DISCUSSION
This population-based study of registry entries for more than 5.9 million persons provided detailed estimates regarding the relationships between various mental disorders and subsequent medical conditions in Denmark. In general, the presence of a mental disorder was associated with an increased risk of subsequent medical conditions — a finding that is similar to the outcomes of previous studies2,3,17–25 and that extends our previous research related to coexisting types of mental disorders.1 Estimates of the risk of a subsequent medical condition among persons with a diagnosed mental disorder were attenuated after adjustment for additional previous mental disorders. Possible reasons for the temporal patterns we observed are included in the Discussion section in the Supplementary Appendix. Some of our findings of a reduced risk of certain medical conditions after specific mental disorders are also consistent with previous reports. For example, investigators have found that persons with schizophrenia have a reduced risk of connective-tissue disorders (e.g., rheumatoid arthritis).26,27 In addition, studies have shown the somewhat paradoxical finding that some patients with mental disorders apparently have a lower risk of cancers,28–30 even though risk factors for cancer (e.g., smoking, obesity, and reduced physical activity) tend to be prevalent in persons with mental disorders. We previously found that men with mental disorders had a higher risk of dying from cancer than men without mental disorders but were less likely than the general population to die prematurely from cancer.31 This finding probably reflects the shortened survival of these men as the result of other medical conditions (e.g., circulatory diseases).
The absolute risks of most medical conditions among persons who received a diagnosis of a mental disorder before the age of 40 years were lower than the risks among those with a later diagnosis. These medical conditions were also prevalent among older persons in the general population, as we found in our population reference group. There were several pairs of mental disorders and medical conditions for which absolute risks for the reference group became greater with age than the risks in the group with mental disorders, particularly at older ages (e.g., circulatory conditions in persons with schizophrenia). This finding may also be a reflection of earlier mortality in persons with mental disorders.5,31
Several factors may have influenced the detection of medical conditions in persons with mental disorders. Studies have shown that persons with mental disorders may be less likely to receive thorough testing for and timely diagnoses of coexisting conditions.32,33 Despite this factor, our findings suggest increased relative and absolute risks of many medical conditions. We do not propose a causal relationship between mental disorders and subsequent medical conditions. The presence of both a mental disorder and a medical condition may be confounded by previous exposures (e.g., substance use, childhood abuse, socioeconomic factors, and shared environmental risk factors) or shared genetic factors.34 Mental disorders affect lifestyle, daily habits, and socioeconomic status, which in turn may mediate the risk of subsequent medical conditions.
Our registry-based study had a large sample size and limited susceptibility to problems caused by recall or self-reporting bias. Because data were available for the entire population, selection bias was minimized. Since Danish citizens have free and equal access to health care, any effect related to the ability to afford private insurance or access to health care was reduced. It is mandatory in Denmark for all hospitals to report discharge diagnoses and for all pharmacies to report redeemed drugs to central registries.
There are important limitations to this study. We restricted medical conditions to 31 specific types, which did not include accidents and injuries or acute conditions. Furthermore, our analyses considered individual pairs of mental disorders and medical conditions, an approach that did not reflect the full spectrum of coexisting conditions because patients may have multiple mental disorders and multiple medical conditions. In addition, there is uncertainty regarding complete ascertainment of mental disorders and medical conditions and precise dates of onset of these conditions. Although registry-based psychiatric diagnoses in Denmark have been found to be generally valid for a range of disorders,10,35–38 validity varies across diagnoses. Underdetection of both mental disorders and medical conditions is likely because we do not have data for persons who did not seek help for their disorders, and no data on diagnoses made by general practitioners are recorded in the registries. These factors may be partially balanced by the recording of prescriptions for disease-specific medications made by general practitioners. Thus, cases were most likely biased to the more severe end of the clinical spectrum for both mental disorders and medical conditions, and the washout period may not have completely removed all prevalent cases of medical conditions. The date of onset, as recorded in the registries, was likely to be later than the actual onset for mental disorders and for many medical conditions. In some cases, this factor may have led to incorrect temporal ordering of mental disorders and medical conditions. Results that relied on the apparent first onset of mental disorders in the seventh to ninth decades of life (e.g., age-specific absolute risks) should be interpreted cautiously. Furthermore, the presence of a medical condition may also lead to an increased risk of subsequent mental disorders.39
Among these limitations, it should be noted that registries allow for a limited length of follow-up. The incidence of mental disorders peaks in the second and third decades of life, whereas the peak for many medical conditions under study occurs later in life. For the calculation of absolute risks in our study, medical conditions had to be diagnosed within 15 years after the diagnosis of the mental disorder because of data availability. This time period may not have been long enough for persons to reach peak ages for the diagnosis of a medical condition and to capture all coexisting conditions. Finally, the generalizability of our findings outside of Denmark is limited. Patterns of coexisting conditions may vary in other countries, especially in those with different health care and socioeconomic structures.
In a large Danish population study, we found that the presence of a mental disorder was associated with a higher risk of many types of subsequent medical conditions. These risks varied according to the pairs of mental disorders and medical conditions and had different temporal patterns of occurrence.
Supplementary Material
Acknowledgments
Supported by the Danish National Research Foundation (Niels Bohr Professorship, to Dr. McGrath), by the John Cade Fellowship (grant number APP1056929, to Dr. McGrath) from the National Health and Medical Research Council, by grants from the Novo Nordisk Foundation (NNF18OC0031194, to Dr. Prior; 22018, to Dr. Dalsgaard; and to Dr. Ribe), by the European Union’s Horizon 2020 Research and Innovation Program under the Marie Sklodowska-Curie grant (agreement number 837180, to Dr. Plana-Ripoll), by a grant from the Aarhus University Research Foundation (AUFF-E-2015-FLS-8-61, to Dr. Dalsgaard), by grants from the Lundbeck Foundation (R102-A9118, R155-2014-1724, and R248-2017-2003, to Dr. Dalsgaard; R102-A9118, to Drs. Werge, Nordentoft, Schork, and Vilhjalmsson; R276-2017-4581 and R248-2017-2003, to Dr. Petersen; R303-2018-3551, to Dr. Musliner; R268-2016-3925 and R278-2018-1411, to Dr. Benros; and R155-2012-11280, to Dr. Vestergaard), by a grant (R01 ES026993, to Dr. Dalsgaard) from the National Institutes of Health (NIH), by a grant (Horizon 2020, grant number 667302, to Dr. Dalsgaard) from the European Commission, by a grant (19-8-0260, to Dr. Dalsgaard) from Helsefonden, by a grant (8020-00013B, to Dr. Debost) from the Danish Council for Independent Research, by a grant (7025-00078B, to Dr. Benros) from the Independent Research Fund Denmark, by a Senior Principal Research Fellowship from the National Health and Medical Research Council of Australia (to Dr. Degenhardt), and by a grant (R01DA1104470, to Dr. Degenhardt) from the NIH National Institute on Drug Abuse.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
APPENDIX
The authors’ full names and academic degrees are as follows: Natalie C. Momen, Ph.D., Oleguer Plana-Ripoll, Ph.D., Esben Agerbo, Dr.Med.Sc., Michael E. Benros, M.D., Ph.D., Anders D. Børglum, M.D., Ph.D., Maria K. Christensen, M.Sc.P.H., Søren Dalsgaard, M.D., Ph.D., Louisa Degenhardt, Ph.D., Peter de Jonge, Ph.D., Jean-Christophe P.G. Debost, M.D., Ph.D., Morten Fenger-Grøn, Ph.D., Jane M. Gunn, Ph.D., M.B., B.S., Kim M. Iburg, Ph.D., Lars V. Kessing, M.D., Dr.Med.Sc., Ronald C. Kessler, Ph.D., Thomas M. Laursen, Ph.D., Carmen C.W. Lim, M.Sc., Ole Mors, M.D., Ph.D., Preben B. Mortensen, M.D., Ph.D., Katherine L. Musliner, Ph.D., Merete Nordentoft, M.D., Dr.Med.Sc., Carsten B. Pedersen, Dr.Med.Sc., Liselotte V. Petersen, Ph.D., Anette R. Ribe, M.D., Ph.D., Annelieke M. Roest, Ph.D., Sukanta Saha, Ph.D., Andrew J. Schork, Ph.D., Kate M. Scott, Ph.D., Carson Sievert, Ph.D., Holger J. Sørensen, M.D., Ph.D., Terry J. Stedman, M.B., B.S., Mogens Vestergaard, M.D., Ph.D., Bjarni Vilhjalmsson, Ph.D., Thomas Werge, Ph.D., Nanna Weye, M.Sc., Harvey A. Whiteford, M.D., Ph.D., Anders Prior, M.D., Ph.D., and John J. McGrath, M.D., Ph.D.
The authors’ affiliations are as follows: the National Center for Register-based Research (N.C.M., O.P.-R., E.A., M.K.C., S.D., J.-C.P.G.D., T.M.L., P.B.M., K.L.M., C.B.P., L.V.P., B.V., N.W., J.J.M.), Center for Integrated Register-based Research (E.A., P.B.M., C.B.P.), the Departments of Biomedicine–Human Genetics (A.D.B.) and Public Health (M.K.C., M.F.-G., K.M.I., M.V., A.P.), the Center for Integrative Sequencing (A.D.B.), and the Big Data Center for Environment and Health (C.B.P.), Aarhus University, the Lundbeck Foundation Initiative for Integrative Psychiatric Research (E.A., A.D.B., S.D., O.M., P.B.M., K.L.M., M.N., C.B.P., L.V.P., A.J.S., B.V., T.W.), the Center for Genomics and Personalized Medicine (A.D.B.), the Department of Neurology (J.-C.P.G.D.), and the Research Unit, Department of Psychosis (O.M.), Aarhus University Hospital, and the Research Unit for General Practice (M.F.-G., A.R.R., M.V., A.P.), Aarhus, the Copenhagen Research Center for Mental Health, Mental Health Center Copenhagen, Copenhagen University Hospital (M.E.B., M.N., H.J.S.), Psychiatric Center Copenhagen (L.V.K.), Faculty of Health and Medical Sciences (L.V.K.), the Department of Clinical Medicine (T.W.), and the Lundbeck Foundation GeoGenetics Center, GLOBE Institute (T.W.), University of Copenhagen, Copenhagen, and the Institute of Biological Psychiatry, Mental Health Center Sankt Hans, Mental Health Services Capital Region, Roskilde (A.J.S., T.W.) — all in Denmark; the National Drug and Alcohol Research Centre, University of New South Wales, Sydney (L.D.), the Department of General Practice, Melbourne Medical School, University of Melbourne, Melbourne, VIC (J.M.G.), and the Queensland Brain Institute (C.C.W.L., S.S., J.J.M.), Queensland Centre for Mental Health Research, the Park Centre for Mental Health (C.C.W.L., S.S., T.J.S., H.A.W., J.J.M.), and the School of Public Health, Faculty of Medicine (H.A.W.), University of Queensland, Brisbane — all in Australia; the Departments of Psychology (P.J.) and Developmental Psychology (A.M.R.), Heymans Institute, and the Interdisciplinary Center, Psychopathology and Emotion Regulation (P.J., A.M.R.), University of Groningen, Groningen, the Netherlands; the Department of Health Care Policy, Harvard Medical School, Boston (R.C.K.); the Neurogenomics Division, Translational Genomics Research Institute, Phoenix, AZ (A.J.S.); the Department of Psychological Medicine, Dunedin School of Medicine, University of Otago, Dunedin, New Zealand (K.M.S.); Sievert Consulting, Minneapolis (C.S.); and the Institute for Health Metrics and Evaluation, University of Washington, Seattle (H.A.W.).
REFERENCES
- 1.Plana-Ripoll O, Pedersen CB, Holtz Y, et al. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiatry 2019;76:259–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 2016;73:150–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tegethoff M, Belardi A, Stalujanis E, Meinlschmidt G. Comorbidity of mental disorders and chronic pain: chronology of onset in adolescents of a national representative cohort. J Pain 2015;16:1054–64. [DOI] [PubMed] [Google Scholar]
- 4.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998;173:11–53. [DOI] [PubMed] [Google Scholar]
- 5.Erlangsen A, Andersen PK, Toender A, Laursen TM, Nordentoft M, Canudas-Romo V. Cause-specific life-years lost in people with mental disorders: a nationwide, register-based cohort study. Lancet Psychiatry 2017;4:937–45. [DOI] [PubMed] [Google Scholar]
- 6.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851–8. [DOI] [PubMed] [Google Scholar]
- 7.Bock JO, Luppa M, Brettschneider C, et al. Impact of depression on health care utilization and costs among multimorbid patients — from the MultiCare Cohort Study. PLoS One 2014;9(3):e91973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brettschneider C, Leicht H, Bickel H, et al. Relative impact of multimorbid chronic conditions on health-related quality of life — results from the MultiCare Cohort Study. PLoS One 2013;8(6):e66742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39:Suppl:22–5. [DOI] [PubMed] [Google Scholar]
- 10.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health 2011;39:Suppl:54–7. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 2014;71:573–81. [DOI] [PubMed] [Google Scholar]
- 12.Prior A, Fenger-Grøn M, Larsen KK, et al. The association between perceived stress and mortality among people with multimorbidity: a prospective population-based cohort study. Am J Epidemiol 2016; 184:199–210. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015;7:449–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health 2011;39:Suppl:38–41. [DOI] [PubMed] [Google Scholar]
- 15.Helweg-Larsen K The Danish Register of Causes of Death. Scand J Public Health 2011;39:Suppl:26–9. [DOI] [PubMed] [Google Scholar]
- 16.Xu R, O’Quigley J. Estimating average regression effect under non-proportional hazards. Biostatistics 2000;1:423–39. [DOI] [PubMed] [Google Scholar]
- 17.Swain NR, Lim CC, Levinson D, et al. Associations between DSM-IV mental disorders and subsequent non-fatal, self-reported stroke. J Psychosom Res 2015; 79:130–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams LS, Ghose SS, Swindle RW. Depression and other mental health diagnoses increase mortality risk after ische-mic stroke. Am J Psychiatry 2004;161:1090–5. [DOI] [PubMed] [Google Scholar]
- 19.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA 2011;306:1241–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stein DJ, Aguilar-Gaxiola S, Alonso J, et al. Associations between mental disorders and subsequent onset of hypertension. Gen Hosp Psychiatry 2014;36:142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Jonge P, Alonso J, Stein DJ, et al. Associations between DSM-IV mental disorders and diabetes mellitus: a role for impulse control disorders and depresssion. Diabetologia 2014;57:699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rapsey CM, Lim CC, Al-Hamzawi A, et al. Associations between DSM-IV mental disorders and subsequent COPD diagnosis. J Psychosom Res 2015;79:333–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scott KM, de Jonge P, Alonso J, et al. Associations between DSM-IV mental disorders and subsequent heart disease onset: beyond depression. Int J Cardiol 2013; 168:5293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson CA, Mishra GD. Depression and risk of stroke in midaged women: a prospective longitudinal study. Stroke 2013;44:1555–60. [DOI] [PubMed] [Google Scholar]
- 25.Merikangas KR, Calkins ME, Burstein M, et al. Comorbidity of physical and mental disorders in the Neurodevelopmental Genomics Cohort Study. Pediatrics 2015;135(4):e927–e938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mors O, Mortensen PB, Ewald H. A population-based register study of the association between schizophrenia and rheumatoid arthritis. Schizophr Res 1999;40:67–74. [DOI] [PubMed] [Google Scholar]
- 27.Chen SJ, Chao YL, Chen CY, et al. Prevalence of autoimmune diseases in inpatients with schizophrenia: nationwide population-based study. Br J Psychiatry 2012;200:374–80. [DOI] [PubMed] [Google Scholar]
- 28.Mortensen PB. The occurrence of cancer in first admitted schizophrenic patients. Schizophr Res 1994;12:185–94. [DOI] [PubMed] [Google Scholar]
- 29.Toender A, Munk-Olsen T, Vestergaard M, et al. Impact of severe mental illness on cancer stage at diagnosis and subsequent mortality: a population-based register study. Schizophr Res 2018;201:62–9. [DOI] [PubMed] [Google Scholar]
- 30.Gulbinat W, Dupont A, Jablensky A, et al. Cancer incidence of schizophrenic patients: results of record linkage studies in three countries. Br J Psychiatry Suppl 1992;18:75–83. [PubMed] [Google Scholar]
- 31.Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet 2019; 394:1827–35. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry 2009;194:491–9. [DOI] [PubMed] [Google Scholar]
- 33.Mai Q, Holman CD, Sanfilippo FM, Emery JD, Preen DB. Mental illness related disparities in diabetes prevalence, quality of care and outcomes: a population-based longitudinal study. BMC Med 2011;9:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amare AT, Schubert KO, Klingler- Hoffmann M, Cohen-Woods S, Baune BT. The genetic overlap between mood disorders and cardiometabolic diseases: a systematic review of genome wide and candidate gene studies. Transl Psychiatry 2017; 7(1):e1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bock C, Bukh JD, Vinberg M, Gether U, Kessing LV. Validity of the diagnosis of a single depressive episode in a case register. Clin Pract Epidemiol Ment Health 2009;5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kessing L Validity of diagnoses and other clinical register data in patients with affective disorder. Eur Psychiatry 1998;13:392–8. [DOI] [PubMed] [Google Scholar]
- 37.Phung TK, Andersen BB, Høgh P, Kessing LV, Mortensen PB, Waldemar G. Validity of dementia diagnoses in the Danish hospital registers. Dement Geriatr Cogn Disord 2007;24:220–8. [DOI] [PubMed] [Google Scholar]
- 38.Lauritsen MB, Jørgensen M, Madsen KM, et al. Validity of childhood autism in the Danish Psychiatric Central Register: findings from a cohort sample born 1990-1999. J Autism Dev Disord 2010;40:139–48. [DOI] [PubMed] [Google Scholar]
- 39.Scott KM, Kokaua J, Baxter J. Does having a chronic physical condition affect the likelihood of treatment seeking for a mental health problem and does this vary by ethnicity? Int J Psychiatry Med 2011;42:421–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


