Abstract
Objectives:
This study examined the link between neighborhood social cohesion, disorder, and physical function in older adults, and identified potential racial/ethnic differences in these associations.
Methods:
Data come the National Health and Aging Trends Study (NHATS; N=5,619). A series of linear regression models were used to predict physical function. Subgroup analyses and neighborhood/race interactions were used to examine differences.
Results:
Neighborhood disorder was associated with poorer physical function (p < .05), while neighborhood cohesion was not (p = .06). Although tests of interactions were not significant, subgroup analyses showed that neighborhood disorder, and not social cohesion, was associated with poorer physical function only in Whites.
Discussion:
Disadvantaged neighborhood social environment may contribute to differences in physical function among older adults. Racial and ethnic differences warrant closer investigation in studies of neighborhoods and functional health.
Keywords: minority health, social environment, neighborhood environment
Literature Review
Empirical as well as theoretical scholarship suggest that as individuals age and their physical, cognitive, and social needs change, their immediate environment becomes more relevant to their health and well-being, in part due to more time spent in their neighborhoods and communities (Lawton & Nahemow, 1973; Vasunilashorn, Steinman, Liebig & Pynoos, 2012). Accordingly, neighborhood environments are particularly important for maintaining the health and well-being of older adults. Research links adverse neighborhood environmental characteristics to mortality, chronic health conditions, poor mental health outcomes, and functional limitations in older individuals (Balfour & Kaplan, 2002; Won, Lee, Forjuoh, & Ory, 2016; Yen, Michael, & Perdue, 2009). Overall, findings suggest that neighborhoods with disadvantaged physical and social environments can negatively affect older adults’ health by limiting access for health promotion (e.g., physical activity) and increasing exposure to psychosocial stressors (e.g., fear of crime). On the other hand, advantaged neighborhood physical and social environments can provide opportunities such as health-promoting resources and social networks that promote health and well-being (Diez Roux & Mair, 2010; Hill, Ross & Angel, 2005; Won et al., 2016; Yen et al., 2009).
Social cohesion and physical disorder are among some of the neighborhood-level processes thought to influence community-dwelling older adults’ health and well-being (Cagney et al., 2009; Latham & Clarke, 2018; Mendes de Leon et al., 2009; Sampson, Raudenbush, & Earls, 1997). Neighborhood social cohesion is generally defined as feelings of mutual trust, connectedness, being close-knit, willingness to help others, and shared values among members of a community (Cagney et al., 2009; Sampson et al., 1997). Low neighborhood social cohesion is linked to adverse health outcomes, including depression, hypertension, diabetes, and mortality in middle-aged and older adults (Cramm, Van Dijk & Nieber, 2013; Lagisetty, et al., 2016; Miao, Wu & Sun, 2018). There is also evidence that high neighborhood social cohesion may be protective of the health of older adults by providing sources of social support and facilitating the adoption of positive health behaviors such as physical activity (Cagney et al., 2009; Choi, Kim, DiNitto & Marti, 2015). A limited number of studies directly examine the association between neighborhood social cohesion and indicators of physical functioning. Physical function generally refers to the capacity to carry out tasks that require physical actions, including ability to complete activities of daily living (ADL), lower extremity strength, and mobility (Van Lummel et al., 2015). A few studies report that, compared to residents in neighborhoods with high social cohesion, those in low-cohesion neighborhoods are more likely to experience limitations in physical function (Beard et al., 2009; Nguyen, Rist, & Glymour, 2016). Within this research, physical function has been typically measured as ADL limitations or self-reported functional disability (e.g., Beard et al., 2009; Nguyen, Rist, & Glymour, 2016).
Neighborhood physical disorder, another neighborhood-level process linked to health, refers to visual signs of community decay and deterioration, such as abandoned buildings, signs of vandalism, and the presence of garbage and graffiti (Cagney et al., 2009; Hill et al., 2005). Neighborhood physical disorder and related concepts, including “neighborhood problems”, “neighborhood safety”, and “residential instability”, have been associated with limited physical functioning (i.e., difficulty with ADLs, self-reported disability) (Balfour & Kaplan, 2002; Beard et al., 2009; Clark et al., 2009; Nguyen et al., 2016). Neighborhood physical disorder can affect health and physical functioning by deterring older adults from engaging in activities outside of the home, in part due to fear of victimization or the presence of physical barriers such as garbage (Latham & Clarke, 2018; Latham & Williams, 2015). Neighborhoods with high physical disorder are linked to poorer self-rated health, depression, chronic health conditions, and higher rates of mortality in middle and older adulthood (Bjornstrom, Ralston, & Kuhl, 2013; Hill et al., 2005; Ross & Mirowsky, 2001).
Race/Ethnicity and Neighborhood Health Effects
The neighborhood environment may differentially affect older adults belonging to racial/ethnic minorities (i.e., Black and Hispanic). For instance, policies associated with structural racism (e.g., red-lining) have contributed to racial inequalities in exposure to disadvantaged neighborhoods (Kershaw, Albrecht, & Carnethon, 2013), particularly among older adults. While much heterogeneity exists, residential segregation has historically exposed ethnic minorities to poor quality neighborhoods characterized by concentrated poverty and limited access to health-promoting resources (Kershaw et al., 2013). This unequal exposure to disadvantaged, or high-risk neighborhood environments, appears to partially explain the poorer health outcomes experienced by Black and Hispanic older adults when compared to Whites (Cagney, Browning & Wen, 2005; Ferraro et al., 2017). Living in a neighborhood environment that lacks social, physical, and economic resources is one of the many ways in which health disadvantages have been shown to accumulate across the life course, disproportionally affecting Black and Hispanic older adults, who are historically an underserved populations (Dannefer, 2003; Ferraro et al., 2017; Karriker-Jaffe et al., 2016). Alternatively, the disproportionally high exposure to disadvantaged neighborhoods has the potential to equip racial/ethnic minorities with skills (e.g., resilience) to counteract the negative effects of neighborhood disadvantage, or normalize neighborhood disadvantage in a way that it reduces its impact on the health of traditionally disadvantaged groups (Angel & Angel, 2006; Cagney et al., 2005; Ferraro et al., 2017; Karriker-Jaffe, Liu, & Johnson, 2016; Merkin, et al., 2009). Given their frequency at which they are exposed to disadvantaged environments, minority older adults may be more resilient than Whites in their capacity to cope with stressful and disadvantaged neighborhoods (Angel & Angel, 2006; Ferraro et al., 2017). While this limited area of research yields mixed findings, a number of studies hint at racial and ethnic differences in the associations between neighborhood-level social processes and health. For instance, there is evidence, albeit limited, that neighborhood social cohesion and physical disorder may have qualitatively different effects on health based on race and ethnicity (Echevarria, Diez-Roux, Shea, Borrell, & Jackson, 2008).
There is mixed evidence regarding racial/ethnic differences in the association between neighborhood social cohesion and health (e.g., Murillo, Echevarria, & Vasquez 2016; Mulvaney-Day, Alegría, & Sribney, 2007; Wong et al., 2018). While some researchers find that the relationship between neighborhood social cohesion and health-related outcomes and behaviors vary by race/ethnicity (e.g., Wong et al., 2018; Yi, Trinh-Shevrin, Yen, & Kwon, 2016), others find no evidence for racial/ethnic differences in these associations (e.g., Echevarria et al., 2008; Olamijuwon, Odimegwi, & De Wet, 2018). For instance, Yi and colleagues (2016) report that high neighborhood social cohesion is associated with meeting recommended amounts of physical activity only among Whites and Hispanics, and not among Black older adults. Others find that the health effects associated with neighborhood racial/ethnic composition- a potential indicator of neighborhood social cohesion- vary by minority group. For instance, living in racially homogeneous/ segregated neighborhoods has been linked to poorer health in Black Americans, likely a result of concentrated poverty and limited resources associated with structural racism in housing (Kershaw et al., 2013). On the other hand, neighborhood racial homogeneity has been shown to be protective for the health of Hispanics (Angel & Angel, 2006; Ferraro et al., 2017). This trend hints at ethnic differences in health despite similar exposure to disadvantaged neighborhoods, or those characterized by low cohesion and high disorder. While some research points to ethnic differences in the ways in which neighborhood environments influence health across similarly-disadvantaged minority groups (Black and Hispanic), some find no evidence of such differences. For instance, studies by Echevarria and colleagues (2008) and Olamijuwon and colleagues (2018) find no racial/ethnic differences in the relationship between social cohesion and walking for exercise, depression, or self-rated health among younger and older adults.
Like social cohesion, there is mixed evidence that the relationship between neighborhood disorder and health and health behaviors operate differently by race/ethnicity (Alegría, Molina, & Chen, 2014; Echevarria et al., 2008). For instance, Alegria and colleagues (2014) find evidence of racial/ethnic differences in the way that neighborhood disorder contributes to depressive and anxiety disorder in adults over age 18. On the other hand, Echevarria and colleagues (2008) find no such association between neighborhood disorder and depression or smoking among middle aged and older adults. Such mixed findings begin to highlight the dearth of knowledge regarding how and whether neighborhoods influence health differently across racial/ethnic membership. Some scholars discuss this research in terms of a “epidemiological paradox” in which, despite being exposed to more disadvantaged environments, cultural resources such as religion and familial support may enhance the resilience of minority groups (Angel & Angel, 2006; Merkin et al., 2009). Alternatively, racial/ethnic minorities who reside in disadvantaged neighborhoods (e.g., low cohesion, high disorder) may find themselves with limited opportunities to avoid these stressful environments, and may experience greater, more adverse health effects as a result (Gilster, 2016). Taken together, there are limited and inconsistent findings on the relationship between neighborhood-level contexts and health and health-promoting behaviors across race and ethnicity.
Physical Function in Neighborhood and Health Research
Physical function refers to the individual’s capacity to carry out tasks that require physical actions, including lower extremity strength and mobility (Van Lummel et al., 2015). Physical functional status is recognized as an indicator for the prevention and treatment of disabling conditions in older adults (Guralnik et al., 1994; Van Lummel et al., 2015). As such, a growing number of studies of neighborhoods and health incorporate physical function as an outcome. However, most of these studies use self-reported physical function (Latham & Clarke, 2018; Schootman, Andresen, Wolisnksy, Malmstrom & Miller, 2006). Performance-based, or objective, measures of physical function can provide more insight into functional status than self-reported measures (Ferraro et al., 2017; Guralnik et al., 1994; Latham & Clarke, 2018). Objective measures are more sensitive to limitations in physical capacity, and as such, can be useful for identifying and predicting physical functioning limitations (Ferraro et al., 2017; Latham & Clarke, 2018). The Short Physical Performance Battery (SPPB) is a reliable and valid measure of lower extremity physical function (Guralnik et al., 1994). The SPPB is associated with important health outcomes, including disability limitations, nursing home admissions, and mortality (Guralnik et al., 1994; Vasunilashorn et al., 2009). Despite the advantages of using objective measures such as the SPPB, a limited number of studies of neighborhood environment characteristics incorporate these measures as primary outcomes (e.g., Samuel, Glass, Thorpe, Szanton, & Roth, 2015). Given the practicality and benefits of performance measures of physical function, there is a need for neighborhood effects research that considers these clinical measures.
While there is increasing recognition of the role of the neighborhood social cohesion and physical disorder on the physical functioning in older adults, there are gaps in the existing literature. First, despite some evidence of racial/ethnic differences on the association between neighborhood contexts and health (Angel & Angel, 2006; Cagney et al., 2005; Merkin, et al., 2009), few studies directly examine racial/ethnic differences in the extent to which neighborhood social cohesion and physical disorder affect older adults’ physical function. Second, studies of neighborhood-level social processes and physical function rarely use performance, or objective, measures of functional status, which may be more sensitive than self-reported measures and more useful for predicting future mobility disability, among other adverse health outcomes (Guralnik et al., 1994; Latham & Clarke, 2018). The current study addresses these gaps by directly examining racial/ethnic differences in the role of neighborhood perceived social cohesion and indicators of neighborhood physical disorder on objectively measured physical performance among older adults.
Research Questions
This study addresses the following research questions:
What is the association between neighborhood social cohesion and physical disorder on objectively measured physical function in older adults?
Is the association between neighborhood social cohesion and physical disorder different across racial and ethnic groups?
Methods
Data
Data come from the round five (2015) of the National Health and Aging Trends Study (NHATS), an epidemiologic panel study of nationally representative Medicare beneficiaries ages 65 and older living in community and residential care settings. NHATS is sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. NHATS oversamples the oldest old- or older adults in the oldest age groups, and Black respondents. Data are collected by trained interviewers and include information on respondents’ demographic characteristics, health and physical functioning, social and economic circumstances, as well as environmental conditions. NHATS includes sampling weights, which allow for the estimation of values for a target population of Medicare beneficiaries over age 65 (DeMatteis, Freedman, & Kasper, 2016). Detailed information on NHATS is available elsewhere (Montaquilla, Freedman, Edwards, & Kaster, 2012).
Of 8,334 respondents in round five, a total of 7,070 interviews were conducted with community-dwelling individuals. The final listwise analytic sample (N = 5,619) is comprised of respondents with valid data on all variables.
Variables
Outcome.
Physical function was objectively assessed using the NHATS expanded SPPB. The original SPPB includes three subtests of physical performance indicators: three increasingly difficult balance stands, a three meter usual-time walking speed to measure locomotion, and five rapid chair stands to reflect lower body muscle function (Kasper, Freedman, & Niefeld, 2012). The NHATS expanded SPPB measure includes an additional balance stand test (standing on one leg with eyes open and closed), which provides a more sensitive indicator of physical function by expanding the range of functioning being tested (Kasper et al., 2012). Summed scores for the NHATS-SPPB range from 0 to 12, with higher scores reflecting better physical functioning. A score of zero was assigned to individuals who were unable to complete a task due to concerns for safety and/or those who attempted the task but did not complete it. NHATS-specific SPPB scoring is based on cut-points that reflect quartiles of the NHATS sample distribution (Kasper et al., 2012). When weighted, the NHATS-SPPB the summary score is representative of non-institutionalized Medicare beneficiaries over the age of 65 (Kasper et al., 2012).
Predictors.
Neighborhood social cohesion was assessed based on participants’ response to three questions: (1) people in my community know each other well, (2) people are willing to help each other, and (3) people can be trusted. Community or neighborhood is self-defined by respondents based on these questions. Each question was answered on a three-point scale (1=do not agree, 2 = agree a little, 3 = agree a lot). Consistent with previous use of this scale, scores were averaged to capture perceptions of community social cohesion (Cronbach’s a= .72) and dichotomized based on the lowest 15th percentile of the distribution (score of 2 or less) to indicate low social cohesion (Latham & Clarke, 2018). Neighborhood physical disorder was measured by an environment checklist in which three items asked interviewers to indicate the presence of litter/trash, graffiti, and number of vacant homes and businesses surrounding the participants’ homes. Interviewers answered as 1=none, 2=a little, 3= some, 4=a lot. Like social cohesion, scores for the three items were averaged (Cronbach’s a =. 72) and dichotomized to indicate any sign of disorder (score of 1.33 or greater) (Latham & Clarke, 2018). The two indicators of neighborhood environment characteristics are based on validated scales and are commonly used in research (Cagney et al., 2009; Kasper & Freedman, 2014; Sampson et al., 1997). The use of both subjective and objective neighborhood characteristics helps understand the unique contribution of perceptions of neighborhood quality (Weden, Carpiano & Robert, 2008).
Covariates.
Race/ethnicity was measured in three categories, as White, Black, and Hispanic; those recorded as “other” were not included in the analyses. Given the sensitive nature of birth date, NHATS public use files categorize age by six 5-year intervals (i.e., 65-69, 70-74, 75-79, 80-84, 85-89, and 90+); these age groups were analyzed as an ordinal scale. Gender was measured as 1=female and 0=male. Educational attainment was measured as 1= college education or higher and 0= less than a college education. For respondents with missing income information, imputed values were used to create a categorical measure of joint household yearly; the five income categories were treated as an ordinal variable. A dichotomous variable was created to indicate marital status, where 1= married/living with partner and 0=other. A dichotomous variable was used to indicate nativity status (1= US-born and 0=foreign-born). Self-rated health was assessed based on an ordinal scale ranging from 1= poor to 5=excellent. Finally, given the importance of physical activity as a mechanism explaining the association between neighborhood environment and physical performance status (Yen et al., 2009), an indicator of physical activity was included in the analysis. Physical activity was indicated by a dichotomous measure (1=physical activity and 0=no physical activity), based on the survey question, “In the last month, did you ever go walking for exercise?”
Analytic Approach
Descriptive.
After data cleaning and recoding, the first phase of analysis focused on examining descriptive statistics for the full analytic sample, as well as by race/ethnicity. Table 1 shows unweighted and weighted descriptive statistics for the full sample and by racial/ethnic subgroups.
Table 1.
Descriptive Statistics for Total Analytic Sample and by Racial/Ethnic Subgroups
| Total (N=5619) | Racial/Ethnic Subsamples | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted | Weighted | - | Weighted | - | |||||||||
| White (n=4091) | Black (n=1163) | Hispanic (n= 365) | |||||||||||
| Mean | SD | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Range | |||
| SPPB Score | 6.38 | 3.40 | 7.22 | 0.04 | 7.47 | 0.05 | 5.74 | 0.10 | 6.01 | 0.18 | 0-12 | ||
| Neighborhood | |||||||||||||
| Low Cohesion | 0.15 | 0.35 | 0.15 | 0.00 | 0.13 | 0.01 | 0.20 | 0.01 | 0.27 | 0.02 | 0-1 | ||
| High Disorder | 0.10 | 0.30 | 0.08 | 0.00 | 0.05 | 0.00 | 0.24 | 0.01 | 0.28 | 0.02 | 0-1 | ||
| Covariates | |||||||||||||
| Age | 3.12 | 1.47 | 2.49 | 0.02 | 2.50 | 0.02 | 2.44 | 0.04 | 2.38 | 0.07 | 1-6 | ||
| Female | 0.57 | 0.50 | 0.55 | 0.01 | 0.54 | 0.01 | 0.60 | 0.02 | 0.56 | 0.03 | 0-1 | ||
| College | 0.45 | 0.50 | 0.50 | 0.01 | 0.53 | 0.01 | 0.37 | 0.01 | 0.21 | 0.02 | 0-1 | ||
| Income | 2.34 | 1.41 | 2.60 | 0.02 | 2.77 | 0.02 | 1.80 | 0.04 | 1.52 | 0.06 | 1-5 | ||
| Partnered | 0.52 | 0.50 | 0.60 | 0.01 | 0.63 | 0.01 | 0.39 | 0.01 | 0.50 | 0.03 | 0-1 | ||
| US Born | 0.91 | 0.28 | 0.90 | 0.00 | 0.95 | 0.00 | 0.91 | 0.01 | 0.32 | 0.03 | 0-1 | ||
| Walk for Exercise | 0.59 | 0.49 | 0.63 | 0.01 | 0.62 | 0.01 | 0.59 | 0.01 | 0.62 | 0.03 | 0-1 | ||
| Self-Rated Health | 3.25 | 1.05 | 3.38 | 0.01 | 3.48 | 0.02 | 2.93 | 0.03 | 2.75 | 0.06 | 1-5 | ||
Note: SPPB=Short Physical Performance Battery; SD= Standard deviation; SE=standard error; Age based on six categories (i.e., 1=65-69, 2=70-74, 3=75-79, 4=80-84, 5=85-89, 6=90+); Self-rated health based on five categories (i.e., 1=poor, 2=fair, 3=good, 4=very good, and 5=excellent). NHATS Round 5 Community Dwelling (N=5619)
Bivariate.
Bivariate analyses using t-tests were conducted to compare average SPPB scores across categories of key predictor variables, including race/ethnicity as well as low/high neighborhood social cohesion and low/high neighborhood physical disorder (Figure 1) for the full sample and by racial/ethnic group. Additional analyses explored average SPPB scores across all predictors and covariates.
Figure 1.
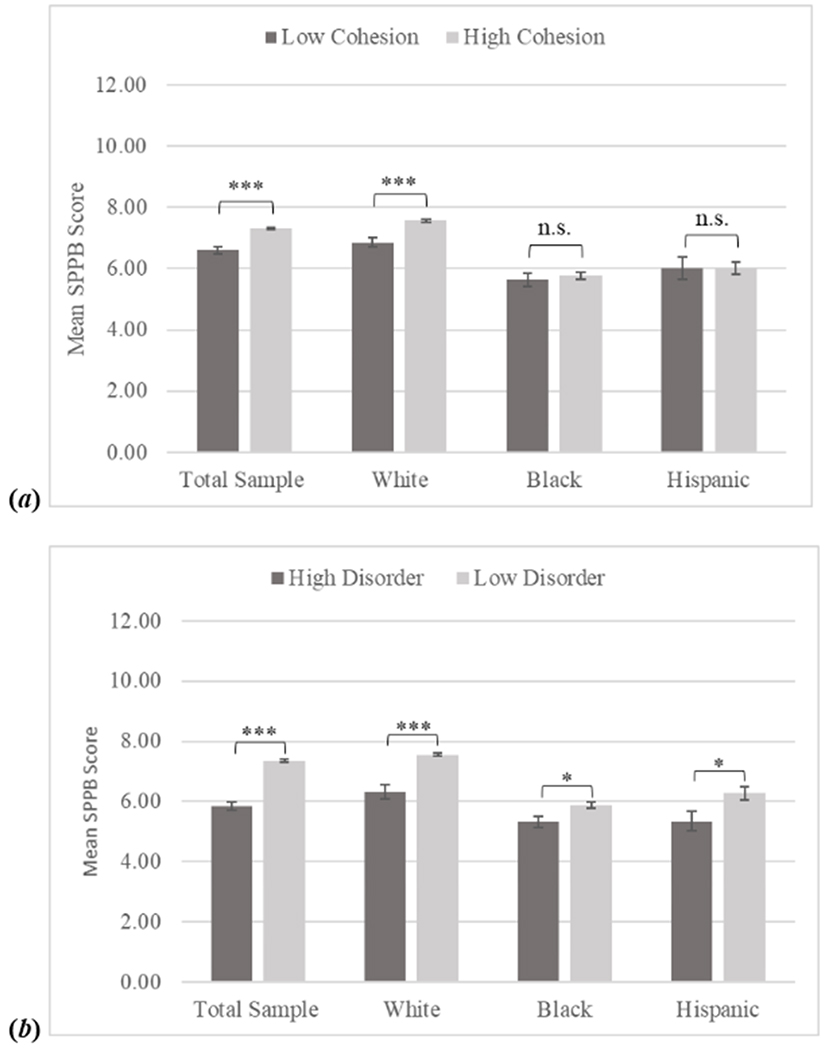
Mean SPPB Score by Neighborhood Context
Note: SPPB=Short Physical Performance Battery Based on weighted data. *** p<.001; * p <.05; n.s. no significance Standard error in bar. NHATS Round 5 (N=5619)
Multivariate.
A series of OLS linear regression models were used to examine the relationships between neighborhood conditions and race/ethnicity on physical functioning (Table 2). Models 1, 2, and 3 progressively build to answer the first research question of whether there is an association between neighborhood conditions and physical function. The last model, Model 4, includes interaction terms for race and neighborhood indicators in order to address research question two, or examine potential differences by race/ethnicity. To expand on these results, Table 4 shows a series of subgroup analyses by race/ethnicity. Multiple additional analyses were conducted to assess the integrity of findings, including regression models that excluded one of the two neighborhood indicators and models including neighborhood indicators as continuous scales. Additionally, sensitivity analyses were conducted to ensure that subgroup analyses were not an artifact of differences in sample size. Results from these additional analyses were consistent with the final findings and therefore not shown but are available on request. Sampling weights were used in all analyses to estimate values representative of Medicare beneficiaries over 65 years of age (DeMatteis et al., 2016). All analyses were conducted using SAS version 9.4 (Copyright © 2013, SAS Institute Inc.).
Table 2.
Nested OLS Regression Models Predicting SPPB Score
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Intercept | 7.47 *** | 7.59 *** | 4.71 *** | 4.73 *** |
| (0.05) | (0.05) | (0.22) | (0.22) | |
| Race/Ethnicity | ||||
| White (ref.) | ||||
| Black | −1.73 *** | −1.52 *** | −0.80 *** | −0.87 *** |
| (0.16) | (0.16) | (0.13) | (0.15) | |
| Hispanic | −1.46 *** | −1.17 *** | −0.54 ** | −0.66 ** |
| (0.16) | (0.17) | (0.16) | (0.19) | |
| Neighborhood | ||||
| Low Social Cohesion | −0.51 *** | −0.16 † | −0.21 † | |
| (0.12) | (0.10) | (0.11) | ||
| High Physical Disorder | −0.98 *** | −0.30* | −0.33* | |
| (0.16) | (0.13) | (0.16) | ||
| Covariates | ||||
| Age | −0.76 *** | −0.76 *** | ||
| (0.03) | (0.03) | |||
| Female | −0.17 * | −0.18 * | ||
| (0.07) | (0.07) | |||
| College | 0.29 *** | 0.29 *** | ||
| (0.08) | (0.08) | |||
| Income | 0.27 *** | 0.27 *** | ||
| (0.03) | (0.03) | |||
| Partnered | 0.16 † | 0.16 † | ||
| (0.08) | (0.08) | |||
| US Born | −0.37 *** | −0.38 *** | ||
| (0.14) | (0.14) | |||
| Walk for Exercise | 1.21 *** | 1.21 *** | ||
| (0.07) | (0.07) | |||
| Self-Rated Health | 0.97 *** | 0.97 *** | ||
| (0.03) | (0.03) | |||
| Interactions | ||||
| Black*Low Cohesion | 0.28 | |||
| (0.32) | ||||
| Hispanic*Low Cohesion | 0.52† | |||
| (0.29) | ||||
| Black*High Disorder | 0.12 | |||
| (0.32) | ||||
| Hispanic*High Disorder | 0.00 | |||
| (0.32) | ||||
| Adjusted R Sq. | 0.03 | 0.04 | 0.42 | 0.42 |
| Model F | 92.25 *** | 61.44 *** | 336.77 *** | 252.81 *** |
| df | 2.00 | 4.00 | 12.00 | 16.00 |
Note: SPPB=Short Physical Performance Battery; Calculated using sample weights; Unstandardized coefficients shown with standard errors in parenthesis;
p <.001;
p <.01;
p < .05;
p <.10.
NHATS Round 5 (N=5619)
Results
Descriptive.
Table 1 presents descriptive statistics for the total analytic sample and by race/ethnic subgroups. Briefly, the majority (74 %) of respondents identified as non-Hispanic White, followed by non-Hispanic Black (20 %), and Hispanic (6 %). Whites had the highest mean SPPB score (7.47), followed by Hispanics (6.01), and Black older adults (5.74). An estimated 15 percent of the total sample was categorized into low social cohesion neighborhoods, and approximately 8 percent lived in neighborhoods with high physical disorder. Hispanics had the highest rates of low social cohesion and high physical disorder (27% and 28%, respectively), followed by Blacks (20% and 24%), then Whites (13% and 5%). The three racial/ethnic subgroups were approximately equally distributed across age and gender. Whites were the group with the highest percentage of college educated adults (53%), highest income category (2.77 out of 5), highest percentage of partnered (63%), and US-born (95%). Approximately 60 percent of older adults across all three-race/ethnic categories reported walking for exercise. Finally, White older adults reported better health, followed by Black, and finally Hispanic.
Bivariate.
A comparison of means test showed significant differences in mean physical function for Whites (M= 7.47, SE=0.05) compared to Blacks (M=5.74, SE=. 10) and Hispanics (M= 6.01, SE=. 18) (t (5252)=15.84, p <. 001, t (4454)= 8.39, p <. 001, respectively), while no meaningful association was observed between Blacks and Hispanics (t (1526)= −1.32, p =. 11). There were significant differences in physical function between those in low versus high cohesion neighborhoods for the total sample and for Whites, but not for Blacks and Hispanics (Figure 1a). Differences in physical function between respondents in high versus low neighborhood disorder were statistically significant across all race/ethnicities, but this relationship was stronger for Whites (Figure 1b).
Multivariate.
A progressive series of OLS regression results predicted lower physical function for Black and Hispanic older adults when compared to Whites, the reference group. These associations remained significant with the introduction of neighborhood characteristics (Table 2; Model 2). Model 2 shows that both, low neighborhood social cohesion and physical disorder are associated with lower physical function. After including covariates (Model 3), physical disorder remained a significant predictor of physical function, while the relationship between social cohesion and physical function weakened. Finally, Model 4 shows that the interaction of Hispanic ethnicity and neighborhood social cohesion was weakly associated, while this was not the case for other interactions of race/ethnicity and neighborhood characteristics. Fully adjusted subgroup analyses (Table 3) showed that both, social cohesion and physical disorder were predictive of physical function among White older adults, with social cohesion having a weaker association. There were no statistically significant associations between neighborhood indicators and physical function for Black or Hispanic older adults.
Table 3.
OLS Regression Models Predicting SPPB Score by Racial/Ethnic Group
| White (n=4091) | Black (n=1163) | Hispanic (n= 365) | |
|---|---|---|---|
| Intercept | 4.83 *** | 3.67 *** | 3.53 *** |
| (0.27) | (0.45) | (0.71) | |
| Neighborhood | |||
| Low Social Cohesion | −0.21 † | 0.08 | 0.20 |
| (0.11) | (0.20) | (0.34) | |
| High Physical Disorder | −0.36 * | −0.12 | 0.00 |
| (0.17) | (0.19) | (0.35) | |
| Covariates | |||
| Age | −0.76 *** | −0.71 *** | −0.79 *** |
| (0.03) | (0.06) | (0.12) | |
| Female | −0.17 * | −0.64 *** | 0.14 |
| (0.08) | (0.17) | (0.32) | |
| College | 0.27 ** | 0.65 *** | 0.07 |
| (0.09) | (0.18) | (0.42) | |
| Income | 0.24 *** | 0.43 *** | 0.83 *** |
| (0.04) | (0.08) | (0.18) | |
| Partnered | 0.15 | −0.17 | 0.74 * |
| (0.09) | (0.18) | (0.32) | |
| US Born | −0.45 * | −0.55 | −0.11 |
| (0.19) | (0.27) | (0.33) | |
| Walk for Exercise | 1.20 *** | 1.08 *** | 1.44 *** |
| (0.08) | (0.17) | (0.32) | |
| Self-Rated Health | 1.00 *** | 1.06 *** | 0.62 *** |
| (0.04) | (0.08) | (0.15) | |
| Adjusted R Sq. | 0.41 | 0.41 | 1.34 |
| Model F | 282.48 *** | 80.11 *** | 20.03 *** |
| df | 10.00 | 10.00 | 10.00 |
Note: SPPB=Short Physical Performance Battery; Calculated using sample weights; Unstandardized coefficients shown with standard errors in parenthesis.
p <.001;
p <.05;
p <.10
NHATS Round 5 (N=5619)
Discussion
There is increasing interest in the association between neighborhood environmental characteristics and functional health outcomes in older adults (Beard et al., 2009; Latham & Williams, 2015; Nguyen et al., 2016). However, several gaps remain in this literature. Namely, neighborhood and health effects studies rarely use performance-based indicators of physical function, and racial/ethnic differences are often overlooked. The current study addresses these gaps by directly examining racial and ethnic differences in the association between neighborhood social cohesion and physical disorder on objectively measured physical function in a sample of older Americans. This study answers two research questions. First, what is the association between neighborhood social cohesion and physical disorder on objectively measured physical function in older adults? Second, is the association between these neighborhood indicators and physical function different across racial and ethnic groups?
Low Cohesion, Physical Disorder, and Poorer Physical Function
In terms of the first research question, signs of neighborhood physical disorder and, to a lesser extent, low perceived social cohesion were associated with poorer physical function. These findings add to a wealth of literature linking specific neighborhood-level contexts to poor health (Cagney et al., 2009; Mendes de Leon et al., 2009; Sampson et al., 1997), and in particular, poor physical functioning and mobility limitations (Balfour & Kaplan, 2002; Beard et al., 2009; Nguyen et al., 2016). Importantly, once individual characteristics such as demographic and socioeconomic indicators, self-rated health, and physical activity are considered, observed neighborhood physical disorder remains associated with poor physical functioning, while social cohesion loses its association. It is worthwhile noting that individual sociodemographic factors and health behaviors are well-established predictors of health and well-being (Winkleby, Jatulis, Frank, & Fortmann, 1992). However, these factors did not entirely explain the association between neighborhood physical disorder and poor physical function in this sample. Results of this study suggest that neighborhood context, particularly signs of physical disorder, may be associated with poor physical function above and beyond individual sociodemographics, health behaviors, and self-rated health.
Few studies report similar findings in relation to these neighborhood environment indicators and health and health behaviors. One of such studies is by Mendes de Leon et al. (2009), who report physical disorder, but not cohesion, to be associated with walking for exercise in older adults. Based on a wealth of previous research (Cagney et al., 2009, Clark et al., 2009; Latham & Clarke, 2018; Nguyen et al., 2016), however, it was hypothesized that both indicators of the neighborhood social environment (social cohesion and physical disorder) would negatively affect physical function. Findings from this study did not find support for this conclusion. A discussion by Bjornstrom and colleagues (2013) brings forward a potential explanation for these results. Their report suggests that while high neighborhood social cohesion and signs of physical disorder are both associated with poorer health outcomes, signs of physical disorder may be stronger and may moderate the relationship between perceived cohesion and health. They argue that perceptions of closeness to one’s neighborhood environment (high social cohesion) may have detrimental health effects for residents in neighborhoods characterized by signs of physical disorder. While this may explain the results, sensitivity analyses provided no such evidence of a moderation in the context of the current study.
Differences in findings across the two neighborhood indicators (social cohesion and physical disorder) may be reflective of the way these concepts are measured; social cohesion is reported by older adults themselves, while physical disorder is assessed by an interviewer at the time the assessment is administered. Additionally, social cohesion is determined by asking respondents about their community, while interviewers assess signs of physical disorder in front of the respondent’s home. While both, self-reported and assessed neighborhood characteristics contribute to our understanding of the association between neighborhoods and health, this difference in measurement may lead to inconsistent findings across social cohesion and physical disorder (Diez Roux & Mair, 2010; Weden, M. M., Carpiano, R. M. Robert, S. A. (2008). Taken together, findings suggest the potential for different pathways between neighborhood social cohesion, physical disorder, and functional health. However, differences in measurement for these two neighborhood social processes warrant caution when interpreting these findings.
Physical Disorder and Poorer Function in Whites, not in Black or Hispanic Older Adults
Related to the second research question, results show limited evidence of racial/ethnic differences in the association between neighborhood social cohesion and physical disorder on physical function. Specifically, disadvantaged neighborhood environments, characterized by signs of physical disorder, were associated with poorer physical function among Whites, but not among Black or Hispanic older adults. These findings add to a growing body of research that shows how neighborhood environmental characteristics may operate differently on health across racial/ethnic groups (Alegria et al., 2014; Karriker-Jaffe et al., 2016). Specifically, these findings may suggest the presence of protective factors for minority older adults and higher risk for White older adults.
While it is erroneous to conclude that all Black and Hispanic older adults reside in disadvantaged neighborhood environments, structural racism, including residential segregation has historically exposed ethnic minorities to poor quality neighborhoods characterized by concentrated poverty and limited access to health-promoting resources (Kershaw et al., 2013). Thus, race and ethnicity may be critical confounders in the neighborhood and health association, given that minority groups are more likely to live in more disadvantaged neighborhoods than Whites, engage less regularly in physical activity than Whites, or be exposed to cultural values (e.g., resiliency) that serve in a protective manner against adverse neighborhood environments (Angel & Angel, 2006; Dannefer, 2003; Ferraro et al., 2017; Mendes de Leon et al., 2009). Indeed, the higher exposure to disadvantaged environments resulting from institutionalized racism and policies such as red-lining may desensitize minority group members to disadvantaged neighborhood conditions and equip them with additional skills, or resilience, to cope with neighborhoods characterized by low cohesion and signs of disorder (Dannefer, 2003; Ferraro et al., 2017; Mendes de Leon et al., 2009). Among members of minority groups, social institutions like family and church may provide sources of support that compensate for exposure to disadvantaged neighborhood contexts (Angel & Angel, 2006). These alternative sources of social support may exist despite exposure to disadvantaged neighborhoods, and may attenuate a neighborhood’s effect on health and health behaviors among racial/ethnically diverse older adults. Thus, future studies could directly examine the roles of social support and social isolation as additional pathways by which the neighborhood context can influence physical function.
A final consideration for these findings relates to the use of culturally-valid measures for assessing neighborhood conditions. The importance of using culturally-valid measurement to make comparisons across perceptions of the environment have been previously mentioned (Dannefer, 2003; Ferraro et al., 2017). In the context of this study, it is possible that racial/ethnic differences stem from measurement error related to the racial/ethnic validity of the neighborhood measures considered. For instance, perceptions of social cohesion may manifest differently among minority older adults than they would for White older adults. Overall, racial/ethnic differences in neighborhood and health research remain poorly understood. Findings from this study add to this literature by highlighting the importance of considering racial/ethnic variability in neighborhood context and physical function.
Limitations and Strengths
This study has several limitations and strengths worth noting. First, the cross-sectional nature of the data limits the ability to assume causal relationships. Issues of causal inference are particularly relevant in neighborhood and health effects research (Diez Roux & Mair, 2010). For instance, healthier individuals may self-select into neighborhoods that encourage health behaviors and promote physical function, such as neighborhoods with high levels of social cohesion and low disorder (Mendes de Leon et al., 2009). Second, analyses are based on a limited measure of physical activity (i.e., “In the last month, did you ever go walking for exercise?”). This broad measure may not accurately capture the amount or frequency of older adults’ engagement in physical activity. Relatedly, this study is unable to distinguish whether respondents use their neighborhood for physical activity. This limitation may result in the over or underestimation in the association between the quality of neighborhood social environments, physical activity, and physical function. Third, neighborhood cohesion and disorder are measured in two different ways; while cohesion is self-reported by older adults, disorder is assessed by an interviewer. These differences in measurement warrant caution when interpreting findings. Fourth, there was no inclusion of measures of comorbidities or perceptions of pain, which, in addition to self-rated health, may help disentangle the association between the neighborhood social environment and physical function. Finally, this study is limited to measures of neighborhood social environment. Characteristics of the neighborhood physical and built environments, such as pedestrian infrastructure, access to facilities, and availability of public transit should all be considered in future research, as they are linked to health and health behaviors (Diez Roux & Mair, 2010; Yen et al., 2009). Notwithstanding these limitations, this study makes important contributions to the literature. First, the study uses nationally representative data with survey weights to examine racial/ethnic differences in the association between indicators of the neighborhood social environment and physical function. Second, physical function is measured using a comprehensive performance-based indicator that captures three important domains of lower extremity function (i.e., gait speed, balance, and strength) (Guralnik et al., 1994; Vasunilashorn et al., 2009). Third, racial/ethnic differences are examined in an attempt to clarify the differential influence of neighborhood contexts on physical function across racial/ethnically diverse groups of older adults.
Implications for Practice and Research
This study brings attention to potential differences in the association between neighborhood contexts (e.g., social cohesion, physical disorder) and physical function among older adults from different racial/ethnic backgrounds. Policies and programs aimed at reducing disparities in physical function can direct resources to improve the quality of neighborhood contexts, particularly reducing signs of neighborhood disorder (e.g., trash, graffiti, abandoned structures). Furthermore, interventions can focus efforts to prevent disparities in functional decline by identifying vulnerable older adults exposed to disadvantaged neighborhood environments.
In order to understand the processes leading to functional disparities, there is a need for research that pays closer attention to racial and ethnic health differences within the context of neighborhood social environments (Dannefer, 2003; Ferraro et al., 2017; Mendes de Leon et al., 2009). Given the findings of this study, future research could examine the protective role that cultural values, such as familial support and spirituality may play in attenuating the effect of adverse neighborhood environments. There is also a need for reliable, valid, and culturally-sensitive scales that allow comparisons across diverse groups of older adults. Perceptions of neighborhood conditions and their effects on health may indeed vary significantly across ethnic membership. Performance-based indicators of physical function may enhance the use of self-reported measures in research and facilitate comparisons across individuals and studies (Ferraro et al., 2017). Taken together, researchers should consider disaggregating data by race/ethnicity and cautiously selecting measures that are valid to the population of interest. Such precautions will improve our understanding of how neighborhood environments can influence health among an increasingly diverse aging population.
Conclusion
Based on an analysis of a nationally representative sample of community dwelling Medicare beneficiaries, findings suggest that there is an association between disadvantaged neighborhood social environments and poor physical function, and that this association varies by race/ethnicity. Community-level interventions should consider the complex interrelation between ethnic membership and neighborhood social environments when addressing issues of health and physical function. Future research should explore racial/ethnic differences in pathways linking neighborhood environments to health and well-being.
References
- Alegría M, Molina KM, & Chen C (2014). Neighborhood characteristics and differential risk for depressive and anxiety disorders across racial/ethnic groups in the United States. Depression and Anxiety, 31(1), 27–37. doi: 10.1002/da.22197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angel JL, & Angel RJ (2006). Minority group status and healthful aging: Social structure still matters. American Journal of Public Health, 96(7), 1152–1159. doi: 10.2105/AJPH.2006.085530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balfour JL, & Kaplan GA (2002). Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. American Journal of Epidemiology, 155(6), 507–515. [DOI] [PubMed] [Google Scholar]
- Beard JR, Blaney S, Cerda M, Frye V, Lovasi GS, Ompad D, Rundle A, & Vlahov D (2009). Neighborhood characteristics and disability in older adults. Journal of Gerontology: Social Sciences, 64B(2), 252–257, doi: 10.1093/geronb/gbn018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjornstrom EES, Ralston ML, & Kuhl DC (2013). Social cohesion and self-rated health: The moderating effect of neighborhood physical disorder. American Journal of Community Psychology, 52(3/4), 302–312. doi: 10.1007/s10464-013-9595-1 [DOI] [PubMed] [Google Scholar]
- Cagney KA, Browning CR, & Wen M (2005). Racial disparities in self-rated health at older ages: What difference does neighborhood make? Journal of Gerontology: Series B Psychological Sciences and Social Sciences, 60(4), 181–190. [DOI] [PubMed] [Google Scholar]
- Cagney KA, Glass TA, Skarupski KA, Barnes LL, Schwartz BS, & Mendes de Leon CF (2009). Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. The Journals of Gerontology, Series B: Social Sciences, 64, 415–424. doi: 10.1093/geronb/gbn041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi NG, Kim J, DiNitto D & Marti CN (2015). Perceived social cohesion, frequency of going out, and depressive symptoms in older adults: Examination of longitudinal relationships. Gerontology and Geriatric Medicine,1–15. doi: 10.1177/2333721415615468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark CR, Kawachi I, Ryan L, Ertel K, Fay ME & Berkman LF (2009) Perceived neighborhood safety and incident mobility disability among elders: the hazards of poverty. BMC Public Health , 9(162). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramm JM, Van Dijk HM, & Nieber AP (2013). The importance of neighborhood social cohesion and social capital for the well being of older adults in the community. The Gerontologist, 53(1), 142–152. [DOI] [PubMed] [Google Scholar]
- DeMatteis J, Freedman VA, & Kasper D (2016). National Health and Aging Trends Study development of round 5 survey weights. NHATS Technical Paper #14 Baltimore: Johns Hopkins University School of Public Health; Available at www.NHATS.org. [Google Scholar]
- Dannefer D (2003). Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory, The Journals of Gerontology: Series B, 58 (6), S327–S337, doi: 10.1093/geronb/58.6.S327 [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, & Mair C (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 125–145, doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Echevarria A, Diez-Roux AV, Shea S, Borrell LN, & Jackson S (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The multi-ethnic study of atherosclerosis. Health & Place , 14(4), 853–865 [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Kemp BR, & Williams MM (2017). Diverse aging and health inequality by race and ethnicity. Innovations in Aging, 00(00) 1–11. doi: 10.1093/geroni/igx002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilster ME (2016). Racial and ethnic differences in the neighborhood context of mastery. Journal of Community Psychology, 44(1), 38–50.https://doi-org.proxy-bc.researchport.umd.edu/10.1002/jcop.21741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, & Wallace RB (1994). A Short Physical Performance Battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49(2), M85–M94. doi: 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Hill TD, Ross CE & Angel RJ (2005). Neighborhood disorder, psychophysiological distress, and health. Journal of Health & Social Behavior, 46 (2), 170–186. [DOI] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ, Liu H Johnson RM (2016). Racial/ethnic differences in associations between neighborhood socioeconomic status, distress and smoking among U.S. adults. Journal of Ethnicity and Substance Abuse, 15(1), 73–91. doi: 10.1080/15332640.2014.1002879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper JD Freedman VA & Niefeld MR (2012). Construction of performance-based summary measures of physical capacity in the National Health and Aging Trends Study. NHATS Technical Paper #4 Baltimore: Johns Hopkins University School of Public Health; Available at www.NHATS.org. [Google Scholar]
- Kershaw KN Albrecht SS, & Carnethon MR (2013). Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans. American Journal of Epidemiology , 177, 299–309. doi: 10.1093/aje/kws372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagisetty PA, Wen M, Choi H, Heisler M, Kanaya AM, & Kandula NR (2016). Neighborhood social cohesion and prevalence of hypertension and diabetes in a south Asian population. Journal of Immigrant and Minority Health, 18(6), 1309–1316. hdoi: 10.1007/s10903-015-0308-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham K & Clarke PJ (2018). Neighborhood disorder, perceived social cohesion, and social participation among older Americans: Findings from the National Health & Aging Trends Study. Journal of Aging and Health, 30(1), 3–26. doi: 10.1177/0898264316665933 [DOI] [PubMed] [Google Scholar]
- Latham K & Williams MM (2015). Does neighborhood disorder predict recovery from mobility limitations? Findings from the Health and Retirement Study. Journal of Aging and Health, 27, 1415–1442. doi: 10.1177/0898264315584328 [DOI] [PubMed] [Google Scholar]
- Lawton MP, & Nahemow L (1973). Ecology and the aging process In Eisendorf C & Lawton MP (Eds.), The psychology of adult development and aging (pp. 619–674). Washington, D.C.: American Psychological Association [Google Scholar]
- Mendes de Leon CF, Cagney KA, Bienias JL, Barnes LL, Skarupski KA, Scherr PA, & Evans DA (2009). Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults: A multi-level analysis. Journal of Aging and Health, 21(1), 155–171. doi: 10.1177/0898264308328650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkin SS, Basurto-Davila R, Karlamangla A, Bird CE, Kurie N, Escarce J, & Seeman T (2009). Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Annals of Epidemiology, 19(3), 194–201. dio: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao J, Wu X Sun X (2018). Neighborhood, social cohesion, and the elderly’s depression in Shangai. Social Science and Medicine. doi: 10.1016/j.socscimed.2018.08.022 [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day NE, Alegria M, & Sribney W (2007). Social cohesion, social support, and health among Latinos in the United States. Social Science and Medicine, 64(2), 477–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murillo R, Echevarria S, & Vasquez E (2016) Differences in neighborhood social cohesion and aerobic physical activity by Latino subgroup. SSM-Population Health, 2, 536–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TT, Rist PM, & Glymour MM (2016). Are self-reported neighbourhood characteristics associated with onset of functional limitations in older adults with or without memory impairment? Journal of Epidemiology & Community Health. doi: 10.1136/jech-2016-207241 [DOI] [PubMed] [Google Scholar]
- NHATS Public Use Data. (Round 5), Sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. Available at www.nhats.org
- Olamijuwon EO, Odimegwu CO, & De Wet N (2018). Social cohesion and self-rated health among adults in South Africa. The moderating role of race. Health and Place, 51, 89–96. [DOI] [PubMed] [Google Scholar]
- Ross CE & Mirowsky J (2001). Neighborhood disadvantage, disorder, and health. Journal of Health and Social Behavior, 42, 258–276 [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW & Earls F (1997). Neighborhoods and violent crime: a multilevel study of collective efficacy. Science, 277 (5328), 918–924. [DOI] [PubMed] [Google Scholar]
- Samuel LJ, Glass TA, Thorpe RJ, Szanton SL & Roth DL (2015). Household and neighborhood conditions partially account for associations between education and physical capacity in the National Health and Aging Trends Study. Social Science and Medicine, 128, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schootman M, Andresen EM, Wolisnksy FD, Malmstrom TK. & Miller JP (2006). Neighborhood conditions and risk of incident lower-body functional limitations among middle-aged African Americans, American Journal of Epidemiology, 163(5), 450–458. [DOI] [PubMed] [Google Scholar]
- Van Lummel RC, Walgaard S, Pijnappels M, Elders PJM, Garcia-Aymerich J, van Dieën JH, & Beek PJ (2015). Physical performance and physical activity in older Adults: Associated but separate domains of physical function in old age. PLoS ONE, 10(12), e0144048.doi: 10.1371/journal.pone.0144048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasunilashorn S, Coppin AK, Patel KV, Lauretani F, Ferrucci L, Bandinelli S, & Guralnik JM (2009). Use of the Short Physical Performance Battery score to predict loss of ability to walk 400 meters: Analysis from the InCHIANTI study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 64A(2), 223–229. doi: 10.1093/gerona/gln022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasunilashorn S, Steinman BA, Liebig PS, & Pynoos J (2012). Aging in place: Evolution of a research topic whose time has come. Journal of Aging Research, doi: 10.1155/2012/120952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weden MM, Carpiano RM Robert SA (2008). Subjective and objective neighborhood characteristics and adults health. Social Science and Medicine, 66(6), 1256–1270. doi: 10.1016/j.socscimed.2007.11.041 [DOI] [PubMed] [Google Scholar]
- Winkleby MA, Jatulis DE, Frank E & Fortmann SP (1992). Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health, 82(6), 816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Won J, Lee C, Forjuoh SN, & Ory MG (2016). Review article: Neighborhood safety factors associated with older adults’ health-related outcomes: A systematic literature review. Social Science & Medicine, 165, 177–186. doi: 10.1016/j.socscimed.2016.07.024 [DOI] [PubMed] [Google Scholar]
- Wong MS, Chan KS, Jones-Smith JC, Colantuoni E, Thorpe JR, & Bleich SN (2018). The neighborhood environment and obesity: Understanding variation by race/ethnicity. Preventative Medicine, 111, 371–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Michael YL, & Perdue L (2009). Neighborhood environment in studies of health of older adults: A systematic review. American Journal of Preventive Medicine, 37(5), 455–463. doi: 10.1016/j.amepre.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi SS, Trinh-Shevrin C, Yen IH, & Kwon SC (2016). Racial/Ethnic differences in associations between neighborhood social cohesion and meeting physical activity guidelines, United States, 2013–2014. Preventing Chronic Disease, 13, E165. doi: 10.5888/pcd13.160261 [DOI] [PMC free article] [PubMed] [Google Scholar]


