Abstract
Introduction
Cavernositis is a rare acute infection of the corporal bodies of the penis. It might result in corporal cavernosal abscesses, fibrosis, and subsequently erectile dysfunction if the treatment is inadequate. Previous reports advocate penile aspiration when cavernosal abscesses were significantly present.
Aim
We report 2 cases of cavernositis treated by the standard antimicrobial therapy in addition to the daily use of phosphodiesterase type 5 inhibitors (iPDE-5).
Methods
We include 2 patients who fulfill the criteria for the diagnosis of cavernositis. They were diagnosed clinically based on history and physical examination. Patient 1 had multifocal abscesses on initial penile contrast-enhanced magnetic resonance imaging (MRI). This patient showed rapid clinical improvement with the addition of phosphodiesterase inhibitor (PDEi) to the antimicrobial therapy without the need for surgical drainage of the abscesses. Patient 2 had persistent infection despite 3 weeks of oral second-generation cephalosporin (Cefuroxime). But he showed significant clinical improvement after being started on PDEi in conjunction with the current antimicrobial therapy. Follow-up after 3 months by clinical examination and penile magnetic resonance imaging in both patients showed normal erectile function with no scarring.
Conclusion
PDEi have promising results on disease progression and outcomes. It synergizes the effect of antimicrobial therapy and can potentially reduce the residual corporal fibrosis and erectile dysfunction. However, large studies are required to validate and generalize this treatment approach.
Bakhsh A, Daqqaq T, Alhasan A, et al. The Role of Phosphodiesterase Inhibitors in the Management of Cavernositis With Multifocal Abscesses: A Report of Case Series. Sex Med 2020;8:318–322.
Key Words: Cavernositis, Impotence, Phosphodiesterase Type 5 Inhibitor, Corpora Cavernosa
Introduction
Cavernositis is a rare disease-causing infection of the corpus cavernosum. Although many cases of cavernositis are idiopathic, different forms can occur in patients who are immunocompromised, having different sites of infection, and/or using intracorporeal injections.1,2 Intracorporeal self-injections used for erectile dysfunction is considered the most common cause of cavernositis in clinical practice. Common organisms include Staphylococcus aureus, Streptococci, and Bacteroides. The mode of therapy has been described in anecdotal reports including antimicrobial therapy and abscess drainage. Although most of the patients require abscess drainage, some of them regain normal erectile function after drainage, and the majority of them may experience variable forms of sexual dysfunction potentially requires further therapy.3,4
Different techniques of abscess drainage have been reported in the literature including image-guided aspiration.4 However, based on reported cases, the incision and drainage approach remain the gold standards to minimize the risk of corporeal fibrosis, penile angulation, and abscess recurrence.4 In the current report, we present 2 cases of cavernositis treated with the standard antimicrobial therapy in addition to daily dose of tadalafil 5 mg, phosphodiesterase type 5 inhibitors (iPDE-5), to potentially optimize the medical therapy and improves the clinical outcomes.
Case series
Patient 1
A 36-year-old healthy male patient presented to the urology clinic with 1-week history of continuous penile pain that was radiated to the pelvis, redness, and swelling [Figure 1]. This was associated with 2-day history of fever, chills, and night sweats. He had no history of urethral discharge. He denied any lower urinary tract symptoms, history of recent infection, extramarital sexual intercourse, or any previous history of sexually transmitted disease. The erection was not experienced by the patient after the onset of infection with a complete flaccid state. On examination, his body temperature was 38.9°C. He was tachycardic with a heart rate of 109 beats/min. His blood pressure was 133/85 mmHg and respiratory rate was 17 breaths/min. The abdominal examination was unremarkable, and there were no palpable inguinal lymph nodes. His genital examination revealed circumcised swollen penile shaft with glandular redness that is associated with deep tenderness over the whole penile shaft. Digital rectal examination revealed the small and non-tender prostate. Urinalysis was unremarkable. The white blood cell count was 8 × 109/L. The urea, electrolyte, liver enzyme, serum blood glucose and hemoglobin levels were all within the normal limits. Sexually transmitted disease workups were negative. Magnetic resonance imaging (MRI) of the penis with contrast showed multiple homogenously enhancing lesions involving the corpus cavernosum compatible with cavenosal abscesses [Figure 2]. The patient was started empirically on intravenous ceftriaxone 1 g every 8 hours, daily dose of oral tadalafil 5 mg, intravenous acetaminophen 1,000 mg every 6 hours, and diclofenac potassium 50 mg orally every 8 hours as per need. During hospitalization, the fever subsided after 48 hours, and gradual improvement of penile edema and swelling was observed on daily clinical examination. As he was improving, penile drainage was not required. His septic workup including blood and urine culture came back negative. The patient was discharged on day 4 on oral cefuroxime 500 mg twice daily and tadalafil 5 mg daily for 3 months. During follow-up, the patient reported normal erection without any adverse sexual function. His erectile hardness score was 4 of 4 and the Sexual Health Inventory for Men score was 25. Follow-up contrast-enhanced MRI of the penis was performed at 3 months [Figure 3] and showed complete disappearance of the previously described corporal abscesses.
Figure 1.

Patient 1: Inflammation of the glans of the penis and edematous penile shaft in the flaccid state (Informed written consent was obtained to demonstrate the clinical finding using the photograph).
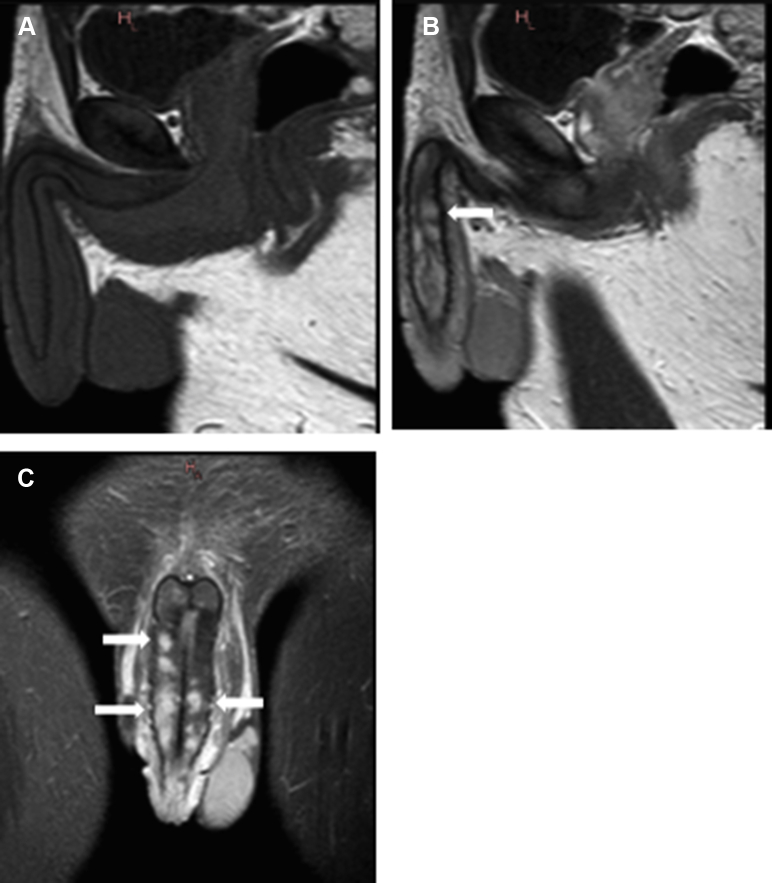
Figure 2.
Patient 1: Magnetic resonance image (MRI) of the penis with multifocal abscesses. (A) Sagittal precontrast T1-weighted MRI. (B) Sagittal T1 after administration of intravenous gadolinium. (C) Coronal postcontrast T1-weighted MRI with fat saturation, showing multiple rounded homogenously enhancing lesions diffusely involving the corpus cavernosum (solid white arrows).
Figure 3.
Patient 1: Magnetic resonance imaging (MRI) of the penis after treatment protocol. (A) Sagittal precontrast T1-weighted MRI. (B) Sagittal postcontrast T1-weighted MRI. (C) Coronal T1-weighted MRI after administration of gadolinium. (D) Coronal postcontrast T1-weighted MRI with fat saturation and after treatment showing normal appearance of the corpus cavernosum with complete resolution of the previously seen abscesses.
Patient 2
A 26-year-old medically free man presented with persistent penile pain and swelling. His pain involved the whole penis that was radiated to the perineum. Onset of symptoms was 3 weeks before the presentation at the clinic. Symptoms included urethral discharge, dysuria, and frequency. The penile pain was exaggerated by erection that lacks rigidity with an erectile hardness score of 2 to 3 of 4 that was different from his usual status. He had regular unprotected vaginal intercourse with his wife. He denied any history of sexually transmitted disease before and denied any new sexual partner apart from his wife who was asymptomatic. He had low-grade fever in 2 different occasions that was documented in other medical centers with 38.9°C in last attack with rigors and sweating. His vital signs were within normal limits during the visit. Abdominal examination was unremarkable with no palpable lymph node. Genital examination revealed a circumcised penis with glandular redness and swelling involving the whole penis associated with tenderness over the penile shaft and perineum. The penile shaft revealed no fluctuation and whitish urethral discharge. Both the testes and epididymis were normal to palpation without tenderness. Digital rectal examination revealed the small and non-tender prostate. Urinalysis was unremarkable. The white blood cell count was 11 × 109/L. The urea, electrolyte, liver enzyme, serum blood glucose, and hemoglobin levels were all within the normal limits. Sexually transmitted disease workup wase negative. The patient did not tolerate MRI study owing to claustrophobia and the imaging study was deferred. Considering the delay in presentation and the lack of complete response to the previously prescribed daily oral antibiotics [doxycycline 100 mg twice a day and cefuroxime 500 mg twice a day] and intramuscular ceftriaxone 250 mg that was given once a time at the onset of the disease, the patient was started on daily tadalafil 5 mg orally in addition to his previously prescribed oral doxycycline 100 mg twice a day and intravenous cefuroxime 750 mg twice a day. The patient showed gradual clinical improvement over the week after starting daily dose of 5 mg tadalafil and shifting to intravenous cefuroxime. He was subsequently followed up in the clinic after 2 weeks. Then, all antibiotics were discontinued, but he continued on oral tadalafil for 3 months and then was discontinued. He reported normal sexual function and potency at 5 months with no residual of sexual dysfunction that was experienced during the disease. The erectile hardness score was 4 of 4 and the Sexual Health Inventory for Men score was 24 of 25.
Discussion
In the current report, we describe a 2 case series for patients with clinical diagnosis of cavernositis. Patient 1 had multifocal abscesses involving both corpora cavernosa bodies. This condition was diagnosed based on clinical history and physical examination and confirmed radiologically by performing a contrast-enhanced MRI of the penis. The management consisted of systemic antibiotics in addition to a daily dose of tadalafil. Despite the presence of multiple corporal abscesses and no surgical drainage performed, complete clinical improvement and recovery of sexual function was achieved. Owing to systemic manifestations at time of presentation, we executed imaging study to rule out abscess that might need drainage. However, previously reported case studies mandate surgical drainage whenever abscess is present. The addition of tadalafil might potentially preclude abscess drainage in our patients and enhanced the clinical improvement.
Patient 2 had no improvement despite oral and intramuscular antibiotics with persistent infection after 3 weeks. However, the urethral discharge disappeared and urinary symptoms improved with the previously prescribed antibiotic regimen. But the clinical picture of cavernositis was persistent that was associated with erectile dysfunction. The addition of daily dose of tadalafil and changing the oral cefuroxime to intravenous mode for 2 weeks in addition to the oral doxycycline resulted in rapid response and complete resolution of symptoms and signs of cavernositis. The improvement could be secondary to the newly modified mode and drug administration, cefuroxime, or mostly secondary to the addition of the tadalafil.
Cavernositis is a rare infectious disease variant. Triggering factors present in the majority of the reported cases that include locally inducing factors or distant infectious disease.4 Different reports described the wide spectrum of infectious agents that include common bacterial, mycobacterial, anaerobic, and fungal infections.4 Several literatures advocate the option of abscess drainage in addition to systemic antimicrobial therapy.4 However, surgical drainage and/or multiple aspirations could result in scarring and consequently might predispose to some elements of sexual dysfunction as reported previously in different case series.5 Explicitly when the penile shaft shows no palpable fluctuation and abscess is multiple and small in imaging studies, early and optimum antimicrobial therapy along with enhancement of blood flow to the corporal bodies can avoid disease progress. And consequently, this will eliminate the need for surgical drainage and could reduce the risk of subsequent corporal fibrosis secondary to inflamed corpora cavernosa tissue as reported in our case series.
Tadalafil has different clinical indications in addition to erectile dysfunction.6,7 The iPDE-5 act differently for each of these clinical indications. The disease spectrum includes chronic prostatitis, stuttering priapism, rehabilitation after radical prostatectomy, and sexual dysfunction in certain patients.6,7 Theoretically, tadalafil may enhances and increases the blood flow and subsequently help in washout and eradication of the infection.8, 9, 10 In our report, we advocate the use of tadalafil in conjunction with the antimicrobial therapy for the management of cavernositis to hasten healing of the inflammatory process by increasing blood supply, which is compromised in case of cavernositis.
Our 2 cases show a new potentially promising treatment approach for cavernositis. And this report describes the potentially beneficial effect of tadalafil when added to antibiotics in cases of bacterial infection of the corpus cavernosum. All previously reported series of cavernositis end up with corporal fibrosis and need corporeal drainage with erectile dysfunction. However, our 2 patients showed complete recovery of erectile function without the need for drainage. This could be the advantageous effect of temporary daily use of tadalafil that was not used in the previously reported series. Although randomization is mandatory to prove the effect in 2 comparable arms of patients that are difficult to conduct owing to infrequency of cases, further case reports in the future might be necessary to prove the effect, required dose, and treatment duration. This case series is limited by the small number of patients explained by the rarity of the disease. Larger study with adequate number of patients in addition to a control group is needed to confirm the potentially beneficial role of adding tadalafil to the standard antimicrobial therapy.
In conclusion, previous reports advocate abscess drainage in addition to systemic antimicrobial therapy for the management of cavernositis. There are no reported cases in the literature regarding the role of tadalafil in the management of cavernositis. The current report describes the potentially beneficial role of the combined therapy to achieve faster and complete recovery from the disease without the need for corpora cavernosa surgical drainage/aspiration and consequently reduce the risk of penile fibrosis and erectile dysfunction.
Statement of authorship
Category 1
-
(a)Conception and Design
- Emad Rajih; Abdulaziz Bakhsh; Mansour Alnazari
-
(b)Acquisition of Data
- Emad Rajih; Abdulaziz Bakhsh
-
(c)Analysis and Interpretation of Data
- Emad Rajih; Ayman Alhasan; Tareef Daqqaq; Abdulaziz Bakhsh; Mansour Alnazari
Category 2
-
(a)Drafting the Article
- Emad Rajih; Tareef Daqqaq; Ayman Alhasan
-
(b)Revising It for Intellectual Content
- Emad Rajih; Ayman Alhasan
Category 3
-
(a)Final Approval of the Completed Article
- Emad Rajih; Abdulaziz Bakhsh
Footnotes
Conflict of Interest: All the authors declare that they have no conflict of interest.
Funding: None.
References
- 1.Moemen M.N., Hamed H.A., Kamel ll. Clinical and sonographic assessment of the side effects of intracavernous injection of vasoactive substances. Int J Impot Res. 2004;16:143–145. doi: 10.1038/sj.ijir.3901194. [DOI] [PubMed] [Google Scholar]
- 2.Pearle M.S., Wendel E.F. Necrotizing cavernositis secondary to periodontal abscess. J Urol. 1993;149:1137–1138. doi: 10.1016/s0022-5347(17)36321-8. [DOI] [PubMed] [Google Scholar]
- 3.Burford C.E., Glenn J.E., Burford E.H. Fibrous cavernositis: further observation with report of 31 additional cases. J Urol. 1946;56:118–120. doi: 10.1016/S0022-5347(17)69782-9. [DOI] [PubMed] [Google Scholar]
- 4.Dugdale C.M., Tompkins A.J., Reece R.M. Cavernosal abscess due to Streptococcus anginosus: a case report and comprehensive review of the literature. Curr Urol. 2013;7:51–56. doi: 10.1159/000343555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shamloul R., Kamel I. Early treatment of cavernositis resulted in erectile function preservation. J Sex Med. 2006;3:320–322. doi: 10.1111/j.1743-6109.2005.00108.x. [DOI] [PubMed] [Google Scholar]
- 6.Masadeh M.M., Alzoubi K.H., Khabour O.F. Ciprofloxacin-induced antibacterial activity is attenuated by phosphodiesterase inhibitors. Curr Ther Res Clin Exp. 2014;77:14–17. doi: 10.1016/j.curtheres.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burnett A.L., Bivalacqua T.J., Champion H.C. Long-term oral phosphodiesterase 5 inhibitor therapy alleviates recurrent priapism. Urology. 2006;67:1043–1048. doi: 10.1016/j.urology.2005.11.045. [DOI] [PubMed] [Google Scholar]
- 8.Peixoto C.A., Santos Gomes F.O. The role of phosphodiesterase-5 inhibitors in prostatic inflammation: a review. J Inflamm. 2015;12:54. doi: 10.1186/s12950-015-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao S., Zhang L., Lian G. Sildenafil attenuates LPS-induced pro-inflammatory responses through down-regulation of intracellular ROS-related MAPK/NF-ΚB signaling pathways in n9 microglia. Int Immunopharmacol. 2011;11:468–474. doi: 10.1016/j.intimp.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Khoshakhlagh P., Bahrololoumi-Shapourabadi M., Mohammadirad A. Beneficial effect of phosphodiesterase-5 inhibitor in experimental inflammatory bowel disease; molecular evidence for involvement of oxidative stress. Toxicol Mech Methods. 2007;17:281–288. doi: 10.1080/15376510601003769. [DOI] [PubMed] [Google Scholar]