Abstract
Background
The world is currently experiencing a pandemic of coronavirus disease 2019 (COVID-19). In Korea, as in other countries, the number of confirmed cases and deaths due to COVID-19 have been rising. This study aimed to calculate the burden of disease due to COVID-19 in Korea.
Methods
We used data on confirmed cases and deaths due to COVID-19 between January 20 and April 24, 2020 provided by the Korea Centers for Disease Control and Prevention, the local governments and the public media to determine disability-adjusted life years (DALYs) by sex and age. Morbidity was estimated directly among the confirmed, cured, and fatal cases. Disability weights were adopted from previous similar causes on the severity of COVID-19 for the years of life lived with disability (YLDs). The years of life lost (YLLs) were calculated using the standard life expectancy from the 2018 life tables for each sex and age.
Results
The YLDs were higher in females (155.2) than in males (105.1), but the YLLs were higher in males (1,274.3) than in females (996.4). The total disease burden attributable to COVID-19 in Korea during the study period, was estimated to be 2,531.0 DALYs, and 4.930 DALYs per 100,000 population. The YLDs and the YLLs constituted 10.3% and 89.7% of the total DALYs, respectively. The DALYs per 100,000 population were highest in people aged ≥ 80 years, followed by those aged 70–79, 60–69, and 50–59 years, but the incidence was the highest in individuals aged 20–29 years.
Conclusion
This study provided the estimates of DALYs due to COVID-19 in Korea. Most of the disease burden from COVID-19 was derived from YLL; this indicates that decision-makers should focus and make an effort on reducing fatality for preparing the second wave of COVID-19.
Keywords: COVID-19, SARS-CoV-2, Burden of Disease, Disability-adjusted Life Years, Years of Life Lost, Years Lived with Disability
Graphical Abstract
INTRODUCTION
The World Health Organization declared a pandemic of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), on March 11, 2020. Between December 2019, when the virus was identified, and end-April 2020, there were more than 2.6 million cases of COVID-19 globally. While it was initially reported that about 80% of confirmed COVID-19 cases are mild with an estimated case fatality of 2.3%,1 the exceptional infection rates of COVID-19 have created multiple cases everywhere at the same time, resulting in increased burden of disease and increased case fatality which has now risen above 7.1%.2
After the first case in Korea was reported from a passenger who had entered via Incheon International Airport outside Seoul on a plane from Wuhan in China, Korea had 10,708 reported COVID-19 cases and 240 reported COVID-19 deaths on April 24, 2020.2,3 Although there are still new imported cases and cases due to community-spread, the number of new cases has slowed; therefore, Korea might be at an end phase of the first wave of the COVID-19 epidemic. However, the whole society is still maintaining the highest level of alert and practicing measures such as social distancing, extensive testing and tracing, and wearing facemasks in public because it is possible that a second wave of COVID-19 will occur.
Despite being a respiratory illness caused by a virus, COVID-19 shows different characteristics to those of other respiratory viruses such as severe acute respiratory syndrome (SARS) and influenza. Knowledge of the natural history of coronavirus is limited, but the burden of disease to our society appears to be substantial. Therefore, this study aimed to calculate the burden of disease due to COVID-19 between January 20 and April 24 in Korea.
METHODS
The disability-adjusted life years (DALYs) in Korea due to COVID-19 were measured using an incidence-based approach.4,5,6 The DALYs were calculated by the sum of the years of life lived with disability (YLDs) and the years of life lost (YLLs).
For the calculation of the YLDs, we used the numbers of confirmed cases by sex and age group, the duration of disease, and disability weights (DWs). The numbers of confirmed cases of COVID-19 by sex or age group were obtained from Korea Centers for Disease Control and Prevention (KCDC).3 The data covered all cases confirmed in Korea, including foreign nationals. To estimate the duration of disease directly, we used the person-days of the confirmed case and days of symptoms before the confirmation of case. The person-days were directly calculated from the numbers of confirmed, cured, and dead cases.
In order to determine the DW of COVID-19, we considered the severity of the disease and its mental health effects even though the classical incidence-based approach does not consider the severity of disease. As the severity of COVID-19 varies from asymptomatic SARS-CoV-2 infection to a severe, and sometimes fatal, disease, we categorized the severity of COVID-19 into 4 categories (asymptomatic, mild, moderate and severe).2,7 In addition, COVID-19-associated anxiety due to the lack of a known effective treatment or cure was also considered. However, as there were no published DW for COVID-19 according to its severity, we adopted DWs of similar conditions. A multiplicative approach was used to combine two DWs.8 Table 1 shows the parameters used for calculation of YLDs and range of sensitivity analyses. We considered the number of confirmed cases and deaths, range of severity distribution, disability weight, and morbid duration as variables with uncertainties.
Table 1. Parameters used to calculate the years lived with disability.
| Parameters | Baseline | Sensitivity analysis | Reference | |||
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| No. of cases | - | 10%/20%/30% increase | Estimation | |||
| Mild | 7,603 | |||||
| All | 10,708 | |||||
| No. of deaths | ||||||
| All | 240 | - | 10%/20%/30% increase | Estimation | ||
| Severity distribution | 7 | |||||
| Proportion of mild | ||||||
| Asymptomatic | 10.0% | 0.0% | - | |||
| Mild | 71.0% | - | 81.0% | |||
| Proportion of severe | ||||||
| Moderate | 14.0% | 10.0% | 18.0% | |||
| Severe | 5.0% | 1.0% | 9.0% | |||
| Disability weight | 8 | |||||
| Upper respiratory infection | 0.088 | 0.045 | 0.154 | |||
| Hemophilus influenzae type B pneumonia | 0.309 | 0.215 | 0.418 | |||
| Maternal sepsis | 0.825 | 0.755 | 0.881 | |||
| Dysthymia | 0.194 | 0.122 | 0.286 | |||
| Duration of disease, day | 28.4 | 21.4 | 35.4 | Estimation | ||
| Burden of isolation for 2 wk after the discharge, per person | - | - | 0.007 | 7,8 | ||
To calculate YLLs, we used the number of deaths and the standard life expectancy for each sex and age. In order to obtain information of death case such as sex and age, we reviewed the press releases from the KCDC. We also checked the official homepage of the local government where the death occurred and the public media to identify the exact sex and age, because the KCDC only reported the number of deaths by sex and age group. The standard life expectancy was obtained from 2018 life tables according to sex and age, published by the Statistics Korea.9 A time discount rate of 3% was applied to the years of standard life expectancy in the future to estimate the net present value of YLLs.5
To compare the results with previous studies, we estimated the YLLs, YLDs, and DALYs per 100,000 population for the mid-year population of 2019 by sex and age, using data from the Statistics Korea demographic survey.10
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Korea University (KU-IRB-18-EX-51-A-1). The requirement for informed consent was waived because no individual-level data were used.
RESULTS
Between January 20, 2020, when the first case of COVID-19 was reported, and April 24, 2020 a total of 10,708 confirmed cases of COVID-19 (20.86 per 100,000 population) were reported in Korea, comprising 4,323 males (16.88 per 100,000 population) and 6,385 females (24.82 per 100,000 population).
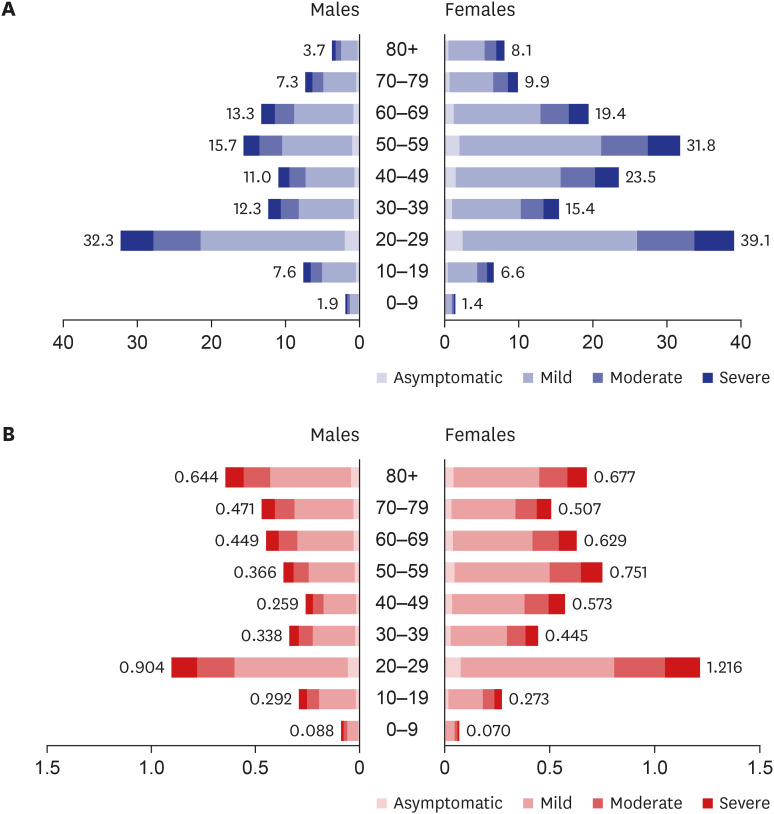
During the study period, there were 260.3 YLDs attributable to COVID-19 in Korea, and 0.507 YLDs per 100,000 population. Females had greater YLDs than males. The YLDs per 100,000 population caused by COVID-19 was 0.410 in males and 0.603 in females. The burden of YLDs was highest in those aged 20–29 years as 32.3 in males and 39.1 in females, and the 0–9-year-old age group had the lowest proportion of YLDs as 1.9 in males and 1.4 in females (Fig. 1A). The YLDs rate per 100,000 population was highest in those aged 20–29 years (1.051) followed by those aged ≥ 80 years (0.666), 50–59 years (0.557), and 60–69 years (0.541) (Fig. 1B).
Fig. 1. YLDs for coronavirus disease 2019 by sex and age group. (A) YLDs; (B) YLDs per 100,000 population.
YLDs = years lived with disability.
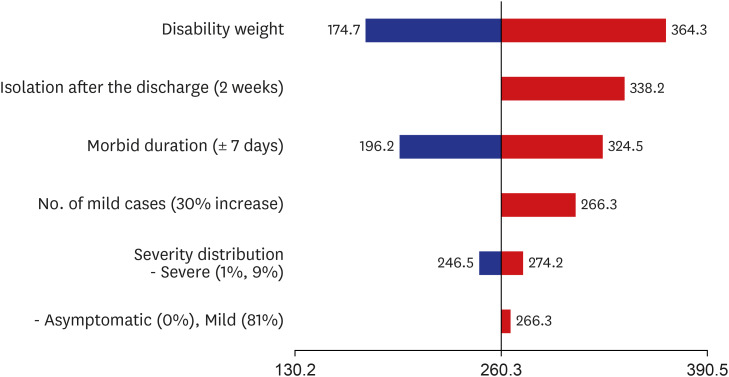
Fig. 2 shows the results of the sensitivity analyses investigating the effect of changes of the parameter estimates on the estimated YLDs. DW was the most sensitive: decreasing the DWs to the lower limit decreased the YLDs to 174.7 (−32.9%), whereas increasing the DWs to the upper limit increased the YLDs to 364.3 (+39.9%). When the duration of COVID-19 was one week longer than the baseline (28.4 days), the YLDs increased to 324.5 (+24.6%). We also considered the scenario of two weeks isolation after discharge. The additional burden from the stress of prolonged isolation increased the YLDs to 338.2, increasing the baseline for YLDs and DALYs by 29.9% and 3.1%, respectively. In addition, we also investigated the effect of a change in the distribution of severity. When the proportion of severe cases was increased to 9%, the YLDs increased to 274.2 (+5.3%). If the classification was based on three stages, reclassification of the asymptomatic cases to the mild category, the YLDs increased to 266.3 (+2.3%).
Fig. 2. Sensitivity analyses of variables used in the calculation of years lived with disability.
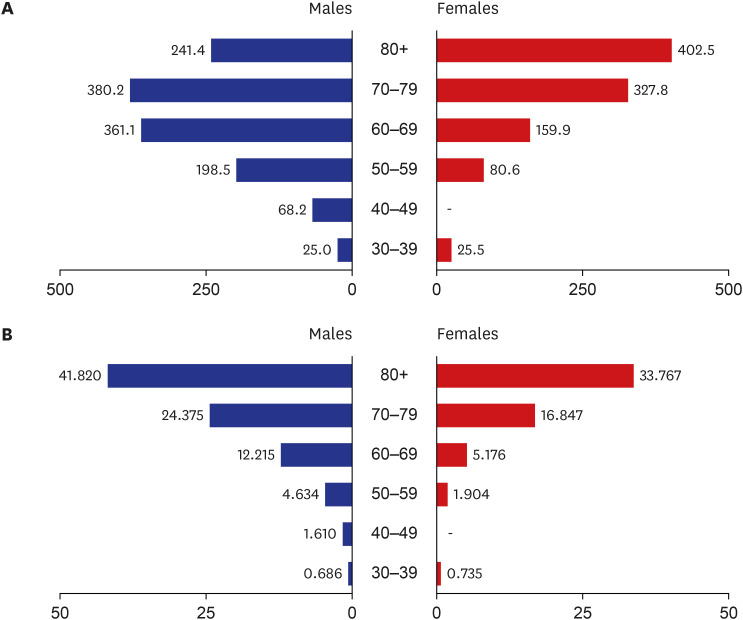
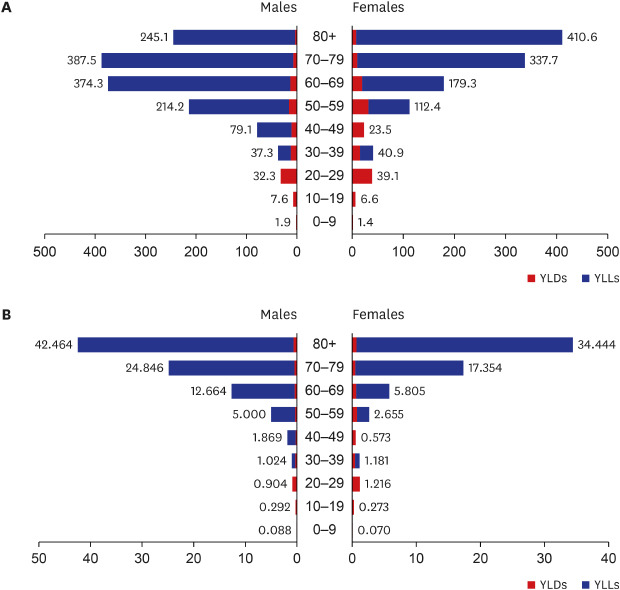
The total number of YLLs caused by COVID-19 was 2,270.7, and YLLs per 100,000 people were 4.423. Contrary to YLDs, the YLLs were greater in males than in females. The deaths from COVID-19 occurred in individuals over 30 years old, the proportion of YLLs was the highest in 70–79 years age group (29.8%) in males, and the ≥ 80 years age group (40.4%) in females (Fig. 3A). The YLLs per 100,000 population increased with age in both sexes (Fig. 3B).
Fig. 3. YLLs for coronavirus disease 2019 by sex and age group. (A) YLLs; (B) YLLs per 100,000 population.
YLLs = years of life lost.
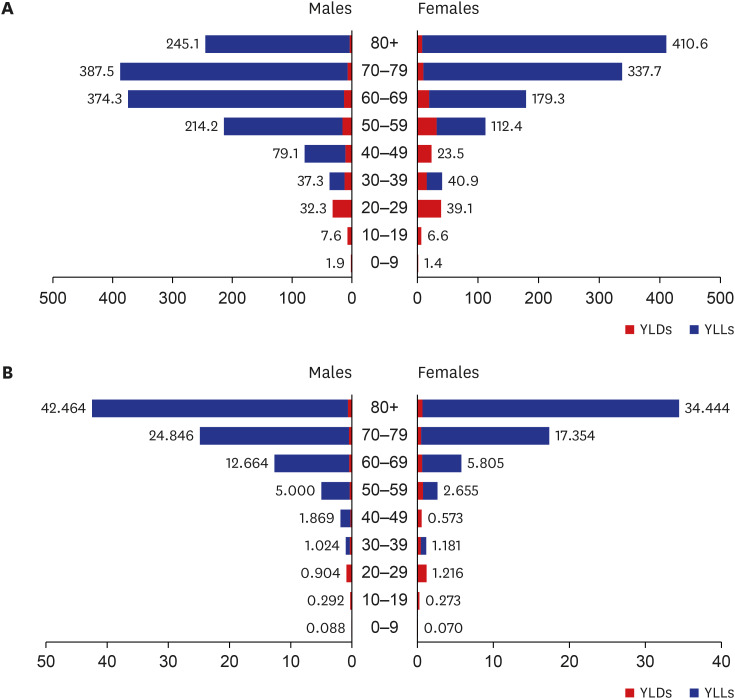
The total DALYs for COVID-19 was 2,531.0, and 4.930 DALYs per 100,000 population. YLDs and YLLs constituted 10.3% and 89.7% of the DALYs, respectively. The relative contribution of YLDs and YLLs to DALYs varied by age, and the contribution of the YLLs increased with age. The proportions of YLDs and YLLs were 100% and 0%, respectively, in under 30 years age group, and 1.8% and 98.2%, respectively, in the ≥ 80 years age group. The total DALYs were highest in the 70–79 years age group (744.7), followed by the ≥ 80 years (662.5), 60–69 years (573.1), and 50–59 years (335.3) age groups (Fig. 4A). The DALYs per 100,000 population were highest in ≥ 80 years age group (37.444), followed by 70–79 years (21.243), 60–69 years (9.481), and the 50–59 years (3.936) age groups (Fig. 4B).
Fig. 4. DALYs for coronavirus disease 2019 by sex and age group. (A) DALYs; (B) DALYs per 100,000 population.
DALYs = disability-adjusted life years.
DISCUSSION
We measured the burden of COVID-19 from the first wave of COVID-19 outbreak from January 20 to April 24 in Korea using incidence-based DALYs. By April 24, there were a total number of 2,531.0 DALYs attributable to COVID-19, comprising 260.3 YLDs and 2,270.7 YLLs at an end of the first wave of COVID-19 in Korea.
The COVID-19 DALYs from the first wave were responsible for 0.017% (males, 0.019%; females, 0.015%) of all-cause DALYs and for 0.61% (males, 1.32%; females, 0.37%) of the communicable disease DALYs, compared to the total disease burden based on the 2016 estimates.11 When we compared with 28 diseases categorized in “Diarrhea, lower respiratory infections, meningitis, and other common infectious diseases,” COVID-19 accounted for 3.52% of DALYs, making it the fifth largest cause of DALYs, after acute bronchitis, upper respiratory infections, giardiasis and pneumococcal pneumonia. Out of 243 diseases, COVID-19 ranked 85th in YLLs and 172nd in YLDs. The burden of COVID-19 had a higher percentage of YLLs (89.7%) and a lower percentage of YLDs (10.3%). The proportion of YLLs is higher than the average of communicable diseases (72.0%), indicating that COVID-19 has a greater impact on premature death.11,12 The portion of YLL will be increasing because the case fatality is increasing for a while in this first wave.
In terms of sex and age group, the DALYs were higher in females than in males and increased with age. We found that the absolute numbers of DALYs were the highest in 70–79 years age group, however, the population adjusted value, representing the DALYs per 100,000 population, showed the highest in ≥ 80 years stage of development group. This implies that the higher the age group, the higher the risk of developing COVID-19 disease and death due to COVID-19, which is consistent with the findings of previous studies reporting age-specific mortality in other countries.13,14,15,16 In the last few days of Korea, the burden of premature death was greater than the burden from the new cases. The care for those at high-risk, who are older adults or have serious underlying medical conditions is now a higher priority.
Compared to other communicable diseases from the KNBD 2016 study, the COVID-19 burden from January 20 to April 24 was 1.39-fold greater than influenza, and 1.16 and 5.18-fold less than pneumococcal pneumonia and upper respiratory infections, respectively. However, the YLDs of COVID-19 were lower than upper respiratory infections and influenza, and greater than pneumococcal pneumonia and Haemophilus influenzae type B pneumonia. In addition, the YLLs were lower than those attributable to pneumococcal pneumonia, and greater than those attributable to the other three diseases. Although comparison with the diseases having similar symptoms, rather than similar epidemiological characteristics has limitations, the number of cases and the incidence rate of COVID-19 was relatively low, on the other hand, the contribution in terms of DALYs was relatively high, because of the higher case fatality rate.
Total burdens of COVID-19 in Korea are expected to be greater than these estimates, and the percentage of total DALYs or rankings could be higher than those reported in this results because it is an ongoing outbreak. There could be undetected cases and there might be more death cases even in the first wave. Especially, if the second wave of COVID will occur, the COVID-19 DALYs will be larger. According to the sensitivity analysis, the number of confirmed cases increased by 10%, 20%, and 30%, the total DALYs increased by 1.0%, 2.1%, and 3.1%, respectively. Alternatively, if only the number of mild cases increased by 10%, 20%, and 30%, the total DALYs increased by 0.6%, 1.2%, and 1.9%, respectively. In addition, the fatality of COVID-19 on April 24 was 2.24% (240/10,708) but increased to 2.35% (256/10,909) on May 11.3 The fatality is likely to increase for a while. According to the sensitivity analysis, as the number of the deaths increased by 10%, 20%, and 30%, the total DALYs increased by 9.0%, 17.9%, and 26.9%, respectively, and the proportion of the YLLs attributable to DALYs increased to 90.6%, 91.3%, and 91.9%, respectively.
Considering these perspectives of COVID-19 burden, we can reduce the burden of COVID-19 even if the second wave will occur. The most important strategy to reduce DALYs of COVID-19 in the second wave will be to focus on reducing case fatality because the portion of YLL was very high. For example, we can set very low case fatality as a target (0.3% of the case fatality of COVID-19 in Seoul). It might be achieved through a well-allocation of healthcare resources like healthcare professionals and beds on severity (i.e., While it could provide a care for mild cases in community treatment centers, severe cases were cared for in hospitals.) It was a lesson from the experiences of the first wave of COVID-19 outbreak. In addition, it is also important to do primary preventions to reduce the incidence through various preventive approaches such a social distancing in a daily life. If the occurrence will overflow than the healthcare resource capacity, it will be very hard to control, and the COVID-19 will increase rapidly. Lastly, as early detections of cases also could reduce their reproductive number, it might reduce incidence of COVID-19.17
The DALY metric, as a summary measure of disease burden, is useful in identifying the impact of a disease on public health, especially the impact of infectious diseases in epidemic situations. This study adopted the incident approach for estimation of DALYs rather than the prevalent approach which was adopted more recently by the Institute for Health Metrics and Evaluation for the Global Burden of Disease study.18,19 The reason why the Institute for Health Metrics and Evaluation adopted the prevalent approach was that it might be easy to obtain the prevalence than the incidence generally.20 However, for COVID-19 in Korea, the confirmed cases were reported in real time by the government. In addition, because the KCDC has been conducting widespread screening for SARS-CoV-2 infection using real-time polymerase chain reaction, the real incidence could be identified.20,21 Moreover, in most cases, information on the outcome (cure or death) and the severity of the disease also were reported by the KCDC, therefore we were able to obtain most of the epidemiologic parameters required to estimate the DALYs based on the COVID-19 notification data. As most governments have reported this information, the methods used in this study could be used to estimate DALYs due to COVID-19 in other countries.
To apply the DWs by severity, we used DWs of diseases having similar symptoms to COVID-19. In addition, we considered the effect of COVID-19 on mental health. One study reported that about 10% of cases were asymptomatic.7 Although there were no respiratory or infectious symptoms, asymptomatic infection can have negative mental health effects because COVID-19 is an emerging disease without a vaccine or any specific treatment. Some studies have reported that COVID-19 patients experience mental health symptoms such as anxiety.22,23 Although many previous burdens of disease studies using an incidence-based approach did not consider disease severity, we considered the disease severity when calculating the DWs because SARS-CoV-2 infection has a wide range of severity from no symptoms to death.7,24 The uncertainty regarding the new disease and anxiety that it could harm other people cause more burden than other diseases. In addition, there is no vaccine or other known effective treatment yet, and the government's actions such as tracking the route of the confirmed patients and informing it to the public, cause not only the disease burden but also the mental burden. Therefore, we tried to calculate the COVID-19 considering its severity and mental impacts. To combine two DWs, multiplicative method was applied because the Global Burden of Disease group also used this approach to combine two or more DWs when they mapped health states into sequalae.20
There are some limitations to this study. First, DWs for COVID-19 were adopted from those of similar respiratory infections diseases because COVID-19 is an emerging disease and COVID-19-specific DWs have not yet been determined. Therefore, the results were interpreted with carefully. In addition, we conducted sensitivity analyses to assess the impact of the assumptions to the range of DALYs estimates. Fortunately, the impact was relatively small because the portion of YLD was relatively smaller than that of YLL. However, it is necessary to estimate specific DWs for COVID-19/SARS-CoV-2 infection to reflect the exact level of disability in the near future. Second, the KCDC only reported the number of deaths by sex and age group, we additionally confirmed data published by local governments and the public media. There was one inconsistent death case between the KCDC and the media in sex classification. The number of female and male was 114 and 126 in this study, whereas 113 and 127 in the KCDC data. The difference in sex caused different life expectancy, however the difference in YLLs is small. After the epidemic stables, the data should be confirmed accurately. Third, the results from this study are not final one because the epidemic is ongoing. We calculated the DALYs of COVID-19 even though the epidemic is ongoing because it is necessary to know the exact burden of COVID-19 to make informed decisions. Once the COVID-19 epidemic has ended, we can estimate the final burden of disease due to COVID-19, and in future it may be useful to estimate it annually.
In conclusion, this is the first study to characterize the disease burden caused by COVID-19 in Korea using DALYs. The methodological framework used in this study can be applied to other countries where disease notification data are collected by the government. Determination of the DALYs attributable to COVID-19 in other countries could provide the basis for international comparisons and prioritization of healthcare resources to control the pandemic. Most of the disease burden from COVID-19 was derived from YLL (89.7%); this indicates that decision-makers should focus and make an effort on reducing fatality for preparing the second wave of COVID-19.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant No. HI18C0446).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yoon SJ, Park H.
- Data curation: Go DS, Kim YE.
- Investigation: Jo MW, Oh IH, Ock M.
- Writing - original draft: Go DS, Kim R.
- Writing - review & editing: Jo MW, Lee SW.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Central Disaster and Safety Countermeasures Headquarters. COVID-19 regular briefing, 2020. [Updated 2020]. [Accessed May 11, 2020]. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=15&CONT_SEQ=353265.
- 3.Korea Centers for Disease Control and Prevention. Cases of COVID-19 in Korea. [Updated 2020]. [Accessed May 11, 2020]. http://ncov.mohw.go.kr/bdBoardList_Real.do?brdId=1&brdGubun=11&ncvContSeq=&contSeq=&board_id=&gubun=
- 4.Yoon J, Yoon SJ. Quantifying burden of disease to measure population health in Korea. J Korean Med Sci. 2016;31(Suppl 2):S101–7. doi: 10.3346/jkms.2016.31.S2.S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global burden of disease and risk factors. The World Bank; 2006. [PubMed] [Google Scholar]
- 6.Yoon SJ, Go DS, Park H, Jo MW, Oh IH, Kim YE. The Korean national burden of disease study: from evidence to policy. J Korean Med Sci. 2018;34(Suppl 1):e89. doi: 10.3346/jkms.2019.34.e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song JY, Yun JG, Noh JY, Cheong HJ, Kim WJ. COVID-19 in South Korea - challenges of subclinical manifestations. N Engl J Med. 2020;382(19):1858–1859. doi: 10.1056/NEJMc2001801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ock M, Lee JY, Oh IH, Park H, Yoon SJ, Jo MW. Disability weights measurement for 228 causes of disease in the Korean burden of disease study 2012. J Korean Med Sci. 2016;31(Suppl 2):S129–38. doi: 10.3346/jkms.2016.31.S2.S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Statistics Korea. Life table. [Updated 2020]. [Accessed April 8, 2020]. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B42&conn_path=I3.
- 10.Statistics Korea. Population Statistics based on resident registration. [Updated 2020]. [Accessed April 8, 2020]. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040M1&conn_path=I3.
- 11.Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019;34(Suppl 1):e75. doi: 10.3346/jkms.2019.34.e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee YR, Moon K, Kim YA, Park SY, Oh CM, Lee KS, et al. Disability-adjusted life years for communicable disease in the Korean burden of disease study 2012. J Korean Med Sci. 2016;31(Suppl 2):S178–S183. doi: 10.3346/jkms.2016.31.S2.S178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chowell G, Mizumoto K. The COVID-19 pandemic in the USA: what might we expect? Lancet. 2020;395(10230):1093–1094. doi: 10.1016/S0140-6736(20)30743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bialek S, Boundy E, Bowen V, Chow N, Cohn A, Dowling N, et al. COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 17.Na BJ, Park Y, Hur IS, Kang CR, Lee J, Lee JY. Seventy two hours, targeting time from first COVID-19 symptom onset to hospitalization. J Korean Med Sci. 2020;35(20):e192. doi: 10.3346/jkms.2020.35.e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 22.Kim SW, Su KP. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caulfield KA, George MS. Treating the mental health effects of COVID-19: The need for at-home neurotherapeutics is now. Brain Stimulat. 2020;13(4):939–940. doi: 10.1016/j.brs.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]