Abstract
Background
Neurocritical care by dedicated neurointensivists may improve outcomes of critically ill patients with severe brain injury. In this study, we aimed to validate whether neurointensive care could improve the outcome in patients with critically ill acute ischemic stroke using the linked big dataset on stroke in Korea.
Methods
We included 1,405 acute ischemic stroke patients with mechanical ventilator support in the intensive care unit after an index stroke. Patients were retrieved from linking the Clinical Research Center for Stroke Registry and the Health Insurance Review and Assessment Service data from the period between January 2007 and December 2014. The outcomes were mortality at discharge and at 3 months after an index stroke. The main outcomes were compared between the centers with and without dedicated neurointensivists.
Results
Among the included patients, 303 (21.6%) were admitted to the centers with dedicated neurointensivists. The patients treated by dedicated neurointensivists had significantly lower in-hospital mortality (18.3% vs. 26.8%, P = 0.002) as well as lower mortality at 3-month (38.0% vs. 49.1%, P < 0.001) than those who were treated without neurointensivists. After adjusting for confounders, a treatment without neurointensivists was independently associated with higher in-hospital mortality (odds ratio [OR], 1.59; 95% confidence intervals [CIs], 1.13–2.25; P = 0.008) and 3-month mortality (OR, 1.48; 95% CIs, 1.12–1.95; P = 0.005).
Conclusion
Treatment by dedicated neurointensivists is associated with lower in-hospital and 3-month mortality using the linked big datasets for stroke in Korea. This finding stresses the importance of neurointensivists in treating patients with severe ischemic stroke.
Keywords: Ischemic Stroke, Neurointensivist, Neurocritically Ill Patients, Outcome, Big Data
Graphical Abstract
INTRODUCTION
Neurocritical care is a subspecialty of critical care medicine that provides optimal and specialized care to neurocritically ill patients.1,2,3 Those patients require special, integrated care on the neurological as well as systemic problems as a part of critical care in the neurological intensive care unit (NICU).1,2,3,4 Several studies show that the existence of neurointensivists and NICU had a significant favorable effect on the outcome of critically ill patients with brain injuries, including stroke.1,5,6,7,8,9 In Korea, specialized critical care teams are relatively lacking compared to other countries.10 Although, the beneficial effect of neurocritical care on patients in NICU have been reported in the literature,6,11 those reports were mainly from single-center experience. Moreover, there is no study reported on the outcome of the special care provided by the neurointensivists for patients with ischemic stroke in Korea. Therefore, we aimed to investigate the association between neurocritical care by dedicated neurointensivists and clinical outcomes in patients with acute ischemic stroke using the linked big data for stroke.
METHODS
Study population
This study was performed using large dataset (n = 52,213, ischemic stroke) by linking the Clinical Research Center for Stroke (CRCS) registry and the Health Insurance Review and Assessment Service (HIRA) administrative claim database with the clinical data collected from patients with acute strokes or transient ischemic attacks (TIA) within 7 days of onset. Detailed information on the study population has been described previously.12
We initially included ischemic stroke patients with 3-month modified Rankin scale (mRS) information (n = 27,479) available from the linking of the CRCS registry data with the HIRA data between January 2007 and December 2014. We excluded patients who visited the hospital before July 2007 (n = 2,511) for updating risk factors and medication information using the linked dataset, and those with missing data regarding the stroke mechanism (n = 61). Given that admission criteria of the intensive care unit (ICU) are varied among the centers and respiratory failure is the most frequent non-cerebral systemic complication among the neurologically ill patients,13 we selected patients with acute ischemic stroke who required mechanical ventilator support due to respiratory failure. Among 24,907 patients, we defined critically ill acute ischemic stroke patients using the following criteria: 1) admitted to the ICU (AJ code), and 2) receiving mechanical ventilation treatment (M5850, M5830, M5857, M5858, M5859, M5860, M5873, and M5874 code) within 1 month of admission according to index stroke using the codes of claim data in the linked dataset. We finally identified 1,405 patients fulfilling the above criteria from 20 centers. Among all the included patients (n = 1,405), 303 patients were admitted to three centers with dedicated neurointensivists while 1,102 patients were admitted to the 17 centers without neurointensivists.
Baseline characteristics and clinical information
Baseline characteristics such as demographic data (age and gender) and vascular risk factors including hypertension, diabetes mellitus, hyperlipidemia, coronary artery disease, atrial fibrillation, history of smoking, and a past history of stroke/transient ischemic stroke, were obtained from the linked data. In addition, clinical data related to acute stroke including stroke severity, reperfusion treatment, stroke mechanisms, medications, and status at discharge were collected from the CRCS registry of the linked data. Stroke severity was assessed using the National Institutes of Health Stroke Scale (NIHSS). Ischemic strokes were classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification, into five categories: 1) large artery atherosclerosis (LAA), 2) small vessel occlusion (SVO), 3) cardioembolism (CE), 4) other determined etiology, and 5) undetermined etiology.14 The primary outcome was mortality at 3 months after ischemic stroke, and mortality rates in critically ill acute ischemic stroke patients were stratified by the 3-month mRS (mRS = 6). The secondary outcome was in-hospital mortality as evaluated by the outcomes at discharge from the CRCS registry.
Statistical analysis
Baseline characteristics are presented as frequency (%), and continuous variables with normal distributions are presented as mean ± standard deviation (SD), while variables that were not normally distributed are presented as median (interquartile range [IQR]). To compare continuous variables, a Student's t-test or a Wilcoxon rank sum test was used when appropriate. In addition, the proportions of categorical variables were compared using Pearson's χ2 tests or the Fisher's exact test, as appropriate, to evaluate the relationship between the presence of neurointensivists and outcomes. We used multiple logistic regression to evaluate the relationship between the outcome and all other covariates studied, including the presence of a neurointensivist. Covariates with statistically significant differences (P < 0.1) in univariate analyses and factors regarded as clinically relevant for mortality were adjusted for multivariate analysis. In addition, we performed further subgroup analyses for age (age < 72 years vs. age ≥ 72 years, median age 72 years), initial NIHSS (NIHSS 0–7, NIHSS 8–13, and NIHSS ≥ 14),15,16 and thrombolytic therapy, using a test of group assignment according to subgroup interaction. For all analyses, a two-tailed P value < 0.05 was considered statistically significant. All statistical analyses were conducted by professional medical statisticians, using SAS 9.4 (SAS Institute, Inc. Cary, NC, USA).
Ethics statement
The study was approved by the Institutional Review Boards (IRB) of Seoul National University Hospital (IRB No. H-1608-078-785). The informed consent was waived by the IRB due to the retrospective nature of this study.
RESULTS
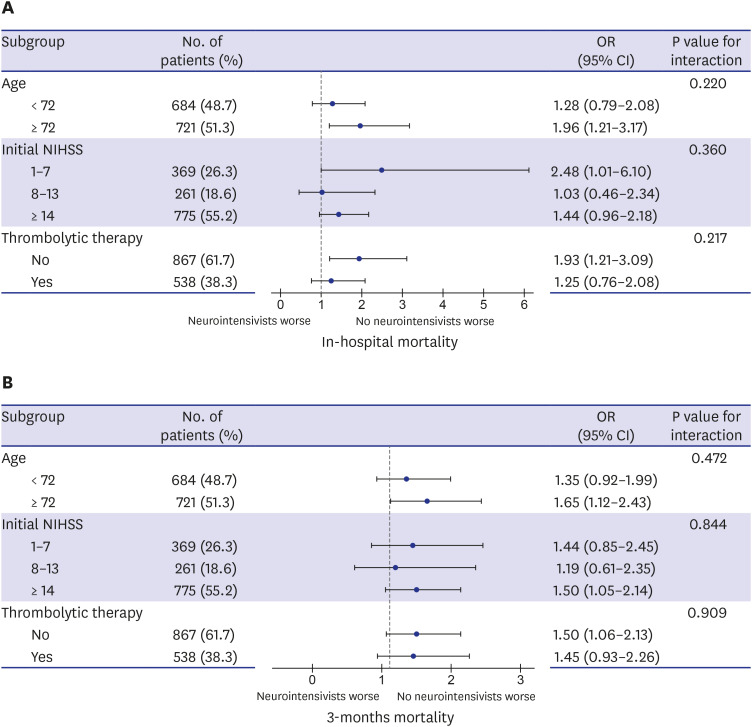
The demographic and baseline characteristics of the included patients are given in Table 1. Among 1,405 patients (men, 58.1%; mean age, 69.1 years), 303 patients (21.6%) were admitted to centers with dedicated neurointensivists and received mechanical ventilation in the ICU after the index ischemic stroke (Table 1). Patients treated in the ICU without dedicated neurointensivists were older, however, vascular risk factors did not differ between the two groups. In addition, the proportion of functionally independent patients prior to index stroke (pre-stroke mRS = 0) was higher in groups treated by neurointensivists. Regarding stroke subtypes, patients with LAA and CE in etiology were more likely to be treated in centers with dedicated neurointensivists while those with undetermined cause were more likely in centers without neurointensivists (P < 0.001) (Table 1). The initial and discharge NIHSS were similar in both groups. Regarding outcomes, the patients treated by neurointensivists had a significantly lower in-hospital mortality (18.3% vs. 26.8%, P = 0.002), 3-month mortality (38.0% vs. 49.1%, P < 0.001) and tended to have more favorable outcome at 3 months (P = 0.05) compared to those treated by non-neurointensivists (Table 1). Multivariate logistic regression analysis showed that treatment without neurointensivists was independently associated with higher in-hospital mortality (odds ratio [OR], 1.59; 95% confidence intervals [CIs], 1.13–2.25; P = 0.008). Moreover, without neurointensivists were associated with higher odds for 3-month mortality (OR, 1.48; 95% CIs, 1.12–1.95; P = 0.005) after adjusting for relevant confounders. In addition, age, coronary artery disease, and initial stroke severity had a profound impact on in-hospital mortality as well as mortality at 3 months (Table 2). The relative benefit of neurointensivists care for in-hospital mortality and 3-month mortality was consistent across all subgroups (P interaction > 0.05 for each) (Fig. 1).
Table 1. Baseline characteristics of included patients.
| Characteristics | With neurointensivists (n = 303, 21.6%) | Without neurointensivists (n = 1,102, 78.4%) | P value | |
|---|---|---|---|---|
| Age, yr | 68.1 ± 13.6 | 70.1 ± 12.1 | 0.022 | |
| Men | 186 (61.4) | 630 (57.2) | 0.190 | |
| Hypertension | 239 (78.9) | 876 (79.5) | 0.810 | |
| Diabetes mellitus | 118 (38.9) | 414 (37.6) | 0.688 | |
| Hyperlipidemia | 113 (37.3) | 430 (39.0) | 0.595 | |
| Atrial fibrillation | 134 (44.2) | 506 (45.9) | 0.649 | |
| Coronary artery disease | 99 (32.7) | 335 (30.4) | 0.483 | |
| Previous stroke/TIA | 93 (30.7) | 326 (29.6) | 0.723 | |
| Smoking | 105 (34.7) | 402 (36.5) | 0.589 | |
| Pre-stroke mRS=0 | 232 (76.6) | 753 (68.3) | 0.009 | |
| Initial NIHSS | 15 (5–21) | 15 (7–19) | 0.653 | |
| Stroke subtypes | < 0.001 | |||
| LAA | 92 (30.4) | 268 (24.3) | ||
| SVO | 5 (1.7) | 19 (1.7) | ||
| CE | 155 (51.2) | 471 (42.7) | ||
| Other determined | 16 (5.3) | 25 (2.3) | ||
| Undetermined | 35 (11.6) | 319 (28.9) | ||
| Thrombolytic therapya | 113 (37.3) | 425 (38.6) | 0.687 | |
| Discharge NIHSS | 17 (6–28) | 16 (6–26) | 0.142 | |
| In-hospital mortality | 54 (18.3) | 291 (26.8) | 0.002 | |
| 3 months mortality | 115 (38.0) | 541 (49.1) | < 0.001 | |
| Good outcome (mRS 0-2) at 3 months | 54 (17.8) | 146 (13.2) | 0.050 | |
Data are presented as mean ± standard deviation or median (interquartile range) or number (%).
TIA = transient ischemic attack, mRS = modified Rankin Scale, NIHSS = National Institute of Health Stroke Scale, LAA = large artery atherosclerosis, SVO = small vessel occlusion, CE = cardioembolism.
aThrombolytic therapy included either intravenous thrombolysis, endovascular recanalization or both.
Table 2. Multivariate logistic regression analysis for mortality.
| Variables | Crude OR | 95% CI | P value | Adjusted OR | 95% CI | P value | |
|---|---|---|---|---|---|---|---|
| In-hospital mortality | |||||||
| Age | 1.02 | 1.01–1.04 | < 0.001 | 1.02 | 1.01–1.03 | 0.004 | |
| Previous stroke/TIA | 0.83 | 0.64–1.09 | 0.187 | 0.79 | 0.58–1.07 | 0.132 | |
| Hyperlipidemia | 1.13 | 0.88–1.45 | 0.323 | 1.23 | 0.93–1.63 | 0.152 | |
| Atrial fibrillation | 1.36 | 1.06–1.74 | 0.014 | 1.12 | 0.77–1.64 | 0.560 | |
| Coronary artery disease | 1.51 | 1.17–1.95 | 0.002 | 1.58 | 1.19–2.11 | 0.002 | |
| Initial NIHSS | 1.06 | 1.04–1.07 | < 0.001 | 1.05 | 1.03–1.07 | < 0.001 | |
| Pre-stroke mRS 1–5 | 1.20 | 0.92–1.56 | 0.176 | 1.08 | 0.80–1.45 | 0.618 | |
| Thrombolytic therapy | 1.14 | 0.89–1.46 | 0.308 | 1.00 | 0.76–1.30 | 0.975 | |
| Without neurointensivists | 1.64 | 1.18–2.26 | 0.003 | 1.59 | 1.13–2.25 | 0.008 | |
| Mortality at 3 months | |||||||
| Age | 1.03 | 1.03–1.04 | < 0.001 | 1.03 | 1.02–1.04 | < 0.001 | |
| Previous stroke/TIA | 0.93 | 0.74–1.17 | 0.511 | 0.79 | 0.61–1.02 | 0.072 | |
| Hyperlipidemia | 1.04 | 0.84–1.29 | 0.703 | 1.029 | 0.80–1.31 | 0.854 | |
| Atrial fibrillation | 1.39 | 1.12–1.71 | 0.003 | 1.09 | 0.78–1.52 | 0.617 | |
| Coronary artery disease | 1.42 | 1.13–1.79 | 0.002 | 1.37 | 1.06–1.76 | 0.015 | |
| Initial NIHSS | 1.04 | 1.02–1.05 | < 0.001 | 1.03 | 1.02–1.05 | < 0.001 | |
| Pre-stroke mRS 1–5 | 1.44 | 1.15–1.83 | 0.002 | 1.22 | 0.95–1.58 | 0.125 | |
| Thrombolytic therapy | 0.86 | 0.70–1.07 | 0.180 | 0.79 | 0.63–1.00 | 0.049 | |
| Without neurointensivists | 1.58 | 1.22–2.05 | < 0.001 | 1.48 | 1.12–1.95 | 0.005 | |
OR = odds ratio, CI = confidence interval, TIA = transient ischemic attack, NIHSS = National Institute of Health Stroke Scale, mRS = modified Rankin scale.
Adjusting for without neurointensivist, age, gender, previous stroke/TIA, hyperlipidemia, diabetes mellitus, hypertension, smoking, atrial fibrillation, coronary artery disease, initial NIHSS, previous mRS, thrombolytic therapy, and stroke subtypes.
Fig. 1. Association between neurointensivists care and outcomes according to subgroups in critically ill patients with acute ischemic stroke. (A) Adjusted for in-hospital mortality. (B) Adjusted for 3-months mortality.
ORs with corresponding 95% CIs for dedicated neurointensivists care within subgroups. Adjusting for without neurointensivist, age, gender, previous stroke/transient ischemic attacks, hyperlipidemia, diabetes mellitus, hypertension, smoking, atrial fibrillation, coronary artery disease, initial NIHSS, previous modified Rankin scale, thrombolytic therapy, and stroke subtypes
OR = odds ratio, CI = confidence interval, NIHSS = National Institutes of Health Stroke Scale.
DISCUSSION
Using the linked big data for stroke, this study showed that treatment with dedicated neurointensivists was associated with lower in-hospital and 3 months mortality in patients with severe ischemic stroke and respiratory failure. Moreover, the lower rate of in-hospital mortality and 3-months mortality after ischemic stroke was consistent across multiple subgroups, which shows that neurointensivists care could decrease mortality rate in broad range of severe ischemic stroke patients, regardless age, stroke severity, and thrombolytic therapy.
Dedicated neurointensivists with organized neurocritical care positively impacted the quality of outcomes including a decrease in mortality and a reduction in hospital length of stay with fewer complications.1,2,5,6,8,17,18 In line with this, care with dedicated neurointensivists was associated with better outcome compared to historical controls previous literature using a single-center registry in Korea. Therefore, it is not clear whether the difference was simply due to the differences in the level of care over time, management protocols, or the role of neurointensivists in the NICU. Using the linked big data for Stroke, we showed that treatment with dedicated neurointensivists was associated with lower in-hospital mortality as well as lower mortality at 3 months, which reiterated the importance of care by dedicated neurointensivists.
In this analysis, we found out that each institution had its own ICU admission criteria for stroke patients. For example, some institutions without neurointensivists usually do not have stroke units and admit minor stroke patients to the ICU seeking for close monitoring. By contrast, three institutions with dedicated neurointensivisits already had stroke units for stroke patients, and the patients who need real ICU care were admitted to the NICU. Therefore, the baseline characteristics of the patients admitted to the ICU (using only AJ code) (n = 7,410) were not comparable, and more severe patients are in the NICU at the institutions with dedicated neurointensivists (initial NIHSS 14 IQR [5–20] in centers with neurointensivists [n = 473, 6.4%] vs. 6 IQR [2–13] in centers without neurointensivists [n = 6,937, 93.6%]) (Supplementary Table 1). Given that respiratory failure is the most common, but important complication in patients with NICU, we selected 1,045 patients with the support of mechanical ventilator among acute ischemic stroke (with neurointensivists group, n = 303 [64.1%, 303 out of 473] and without neurointensitivsts group, n = 1,102 [15.9%, 1,102 out of 6,937]), and then the baseline characteristics were comparable between the two groups (Table 1). Based on the analysis, age and stroke severity as measured by the NIHSS were also independently associated with higher mortality, which was consistent with previous studies.19,20,21 Indeed, our finding also showed that acute ischemic stroke patients requiring mechanical ventilation have high mortality rate.22,23,24
Despite the increasing importance of critical care, organized multidisciplinary critical care units in Korea are not adequate when compared to those in other countries. In Korea, only 20%–30% of the ICUs have specialized neurointensivists.6,10,11,25 The lower number of neurointensivists and neurocritical care teams in Korea is particularly alarming because many of the neurocritically ill ischemic stroke patients receive a lower level of critical care, and this may adversely affect their outcomes. A neurocritical care team with a specialized neurointensivist is required for the best organized management of patients with severe ischemic stroke.26
This study has several limitations. First, this is a retrospective study based on the linked big data for stroke. Therefore, a certain degree of bias is inevitable. Second, the linked dataset do not contain laboratory, clinical or radiological information during the ICU care. Therefore, important information related to mortality in the ICU was not available including several scoring systems for the severity of illness such as the acute physiology and chronic health evaluation II, the simplified acute physiology score II, and several medical complications including sepsis.27,28 Moreover, the association between stroke severity and the location of the lesions, whether they are in the anterior or posterior circulation territories, were not evaluated.29 Third, we analyzed the results using the linked claim data. Therefore, we did not have detailed information on the reasons for mechanical ventilation or ICU admission in the study population. Fourth, this study was performed using the linked stroke registry data, and we cannot prove a cause and effect relationship to explain how multidisciplinary neurocritical care team facilitates the implementation of the best clinical practices such as evidence-based treatments.
In conclusion, our study suggests that specialized care with a dedicated neurointensivist was associated with less mortality in patients with severe stroke patients. This result provides a basis for the establishment of the NICU and could encourage the development of a more multidisciplinary neurocritical care team that can provide specialized and standardized critical care for the neurocritically ill patients in Korea. Further large-scale investigations should be conducted to confirm the true relationship between specialized neurointensivist care and the outcomes in neurocritically ill patients.
Footnotes
Funding: This study was supported by Grants from Korean Neurocritical Care Society (2016) (SBK) and the Ministry of Health and Welfare (HI 16C1078), Korea (BWY). The funding organization had no role in the study or in the preparation of this report.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim TJ, Ko SB, Lee BC, Yu KH, Yoon BW.
- Data curation: Kim TJ, Kim JW, Oh MS, Lee JS.
- Formal analysis: Kim TJ, Lee JS, Yoon JS.
- Investigation: Kim TJ, Oh MS, Jung KH.
- Methodology: Kim TJ, Kim JW, Lee JS.
- Software: Kim JW, Lee JS.
- Supervision: Oh MS, Jung KH, Ko SB, Yu KH, Lee BC, Yoon BW.
- Validation: Yoon JS, Lee JS.
- Writing - original draft: Kim TJ, Ko SB.
- Writing - review & editing: Ko SB, Yu KH, Lee BC, Yoon BW.
SUPPLEMENTARY MATERIAL
Baseline characteristics of patients with intensive care unit admission (using AJ code)
References
- 1.Soliman I, Aletreby WT, Faqihi F, Mahmood NN, Ramadan OE, Mady AF, et al. Improved outcomes following the establishment of a neurocritical care unit in saudi arabia. Crit Care Res Pract. 2018;2018:2764907. doi: 10.1155/2018/2764907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarpong Y, Nattanmai P, Schelp G, Bell R, Premkumar K, Stapleton E, et al. Improvement in quality metrics outcomes and patient and family satisfaction in a neurosciences intensive care unit after creation of a dedicated neurocritical care team. Crit Care Res Pract. 2017;2017:6394105. doi: 10.1155/2017/6394105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suarez JI. Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med. 2006;34(9) Suppl:S232–S238. doi: 10.1097/01.CCM.0000231881.29040.25. [DOI] [PubMed] [Google Scholar]
- 4.Moheet AM, Livesay SL, Abdelhak T, Bleck TP, Human T, Karanjia N, et al. Standards for neurologic critical care units: a statement for healthcare professionals from the neurocritical care society. Neurocrit Care. 2018;29(2):145–160. doi: 10.1007/s12028-018-0601-1. [DOI] [PubMed] [Google Scholar]
- 5.Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29(3):635–640. doi: 10.1097/00003246-200103000-00031. [DOI] [PubMed] [Google Scholar]
- 6.Jeong JH, Bang J, Jeong W, Yum K, Chang J, Hong JH, et al. A dedicated neurological intensive care unit offers improved outcomes for patients with brain and spine injuries. J Intensive Care Med. 2019;34(2):104–108. doi: 10.1177/0885066617706675. [DOI] [PubMed] [Google Scholar]
- 7.Josephson SA, Douglas VC, Lawton MT, English JD, Smith WS, Ko NU. Improvement in intensive care unit outcomes in patients with subarachnoid hemorrhage after initiation of neurointensivist co-management. J Neurosurg. 2010;112(3):626–630. doi: 10.3171/2009.8.JNS09441. [DOI] [PubMed] [Google Scholar]
- 8.Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32(11):2311–2317. doi: 10.1097/01.ccm.0000146132.29042.4c. [DOI] [PubMed] [Google Scholar]
- 9.Varelas PN, Schultz L, Conti M, Spanaki M, Genarrelli T, Hacein-Bey L. The impact of a neuro-intensivist on patients with stroke admitted to a neurosciences intensive care unit. Neurocrit Care. 2008;9(3):293–299. doi: 10.1007/s12028-008-9050-6. [DOI] [PubMed] [Google Scholar]
- 10.Lim CM, Kwak SH, Suh GY, Koh Y. Critical care in Korea: present and future. J Korean Med Sci. 2015;30(11):1540–1544. doi: 10.3346/jkms.2015.30.11.1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryu JA, Yang JH, Chung CR, Suh GY, Hong SC. Impact of neurointensivist co-management on the clinical outcomes of patients admitted to a neurosurgical intensive care unit. J Korean Med Sci. 2017;32(6):1024–1030. doi: 10.3346/jkms.2017.32.6.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim TJ, Lee JS, Kim JW, Oh MS, Mo H, Lee CH, et al. Building linked big data for stroke in Korea: linkage of stroke registry and national health insurance claims data. J Korean Med Sci. 2018;33(53):e343. doi: 10.3346/jkms.2018.33.e343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pelosi P, Ferguson ND, Frutos-Vivar F, Anzueto A, Putensen C, Raymondos K, et al. Management and outcome of mechanically ventilated neurologic patients. Crit Care Med. 2011;39(6):1482–1492. doi: 10.1097/CCM.0b013e31821209a8. [DOI] [PubMed] [Google Scholar]
- 14.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 15.Fonarow GC, Saver JL, Smith EE, Broderick JP, Kleindorfer DO, Sacco RL, et al. Relationship of national institutes of health stroke scale to 30-day mortality in medicare beneficiaries with acute ischemic stroke. J Am Heart Assoc. 2012;1(1):42–50. doi: 10.1161/JAHA.111.000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubin G, Firlik AD, Levy EI, Pindzola RR, Yonas H. Relationship between cerebral blood flow and clinical outcome in acute stroke. Cerebrovasc Dis. 2000;10(4):298–306. doi: 10.1159/000016074. [DOI] [PubMed] [Google Scholar]
- 17.Knopf L, Staff I, Gomes J, McCullough L. Impact of a neurointensivist on outcomes in critically ill stroke patients. Neurocrit Care. 2012;16(1):63–71. doi: 10.1007/s12028-011-9620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bershad EM, Feen ES, Hernandez OH, Suri MF, Suarez JI. Impact of a specialized neurointensive care team on outcomes of critically ill acute ischemic stroke patients. Neurocrit Care. 2008;9(3):287–292. doi: 10.1007/s12028-008-9051-5. [DOI] [PubMed] [Google Scholar]
- 19.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45(1):315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seminog OO, Scarborough P, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute stroke in England: linked national database study of 795 869 adults. BMJ. 2019;365:l1778. doi: 10.1136/bmj.l1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaartjes I, O'Flaherty M, Capewell S, Kappelle J, Bots M. Remarkable decline in ischemic stroke mortality is not matched by changes in incidence. Stroke. 2013;44(3):591–597. doi: 10.1161/STROKEAHA.112.677724. [DOI] [PubMed] [Google Scholar]
- 22.Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007;6(3):215–222. doi: 10.1016/S1474-4422(07)70036-4. [DOI] [PubMed] [Google Scholar]
- 23.Kwan J, Hand P. Early neurological deterioration in acute stroke: clinical characteristics and impact on outcome. QJM. 2006;99(9):625–633. doi: 10.1093/qjmed/hcl082. [DOI] [PubMed] [Google Scholar]
- 24.Rieke K, Schwab S, Krieger D, von Kummer R, Aschoff A, Schuchardt V, et al. Decompressive surgery in space-occupying hemispheric infarction: results of an open, prospective trial. Crit Care Med. 1995;23(9):1576–1587. doi: 10.1097/00003246-199509000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Kim JH, Hong SK, Kim KC, Lee MG, Lee KM, Jung SS, et al. Influence of full-time intensivist and the nurse-to-patient ratio on the implementation of severe sepsis bundles in Korean intensive care units. J Crit Care. 2012;27(4):414.e11–414.e21. doi: 10.1016/j.jcrc.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 26.Barnato AE, Kahn JM, Rubenfeld GD, McCauley K, Fontaine D, Frassica JJ, et al. Prioritizing the organization and management of intensive care services in the United States: the PrOMIS Conference. Crit Care Med. 2007;35(4):1003–1011. doi: 10.1097/01.CCM.0000259535.06205.B4. [DOI] [PubMed] [Google Scholar]
- 27.Khwannimit B, Geater A. A comparison of APACHE II and SAPS II scoring systems in predicting hospital mortality in Thai adult intensive care units. J Med Assoc Thai. 2007;90(4):643–652. [PubMed] [Google Scholar]
- 28.Sakr Y, Krauss C, Amaral AC, Réa-Neto A, Specht M, Reinhart K, et al. Comparison of the performance of SAPS II, SAPS 3, APACHE II, and their customized prognostic models in a surgical intensive care unit. Br J Anaesth. 2008;101(6):798–803. doi: 10.1093/bja/aen291. [DOI] [PubMed] [Google Scholar]
- 29.Kim JT, Park MS, Choi KH, Kim BJ, Han MK, Park TH, et al. Clinical outcomes of posterior versus anterior circulation infarction with low national institutes of health stroke scale scores. Stroke. 2017;48(1):55–62. doi: 10.1161/STROKEAHA.116.013432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Baseline characteristics of patients with intensive care unit admission (using AJ code)