Authors contribution
SRA, AD, MMM, PBA, RRN, JJG, AIR contributed to the analysis of the data and the writing of the manuscript.
To the Editor,
Coronavirus disease 2019 (COVID‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) is a pandemic that is evolving rapidly at present with unprecedented global health and societal implications. Herein, we report a case of successful treatment of SARS‐CoV‐2 induced inflammatory syndrome by utilization of the interleukin‐6 receptor antagonist (IL‐6Ra) tocilizumab.
The patient is a 65‐year‐old Hispanic female with history of end‐stage renal disease secondary to long‐standing diabetes and hypertension who received a deceased donor renal transplant four years prior. She had uneventful post‐transplant course with a baseline serum creatinine (SCr) of 1.2 mg/dL and maintained on triple immunosuppressive regimen of tacrolimus, mycophenolate, and prednisone. She presented to the hospital with a 1‐week history of worsening cough and shortness of breath. Upon presentation, patient was hypoxic with oxygen saturation of 91% on room air. Her examination was significant for crackles in both lung fields. Laboratory findings revealed WBC 4.9 k/mm3 with lymphopenia (0.6 k/mm3), procalcitonin 0.17 ng/mL, troponin‐I <0.040 ng/mL, BNP 68 pg/mL, SCr 1.3 mg/dL, AST 39 units/L, and tacrolimus trough level 7.0 ng/mL. Chest X‐ray (CXR) showed bilateral reticulonodular pulmonary opacities. Supplemental oxygen of 2 L/min by nasal cannula and an empiric antibiotic regimen of ceftriaxone and azithromycin were initiated. A nasal swab multiplex viral PCR panel and blood cultures were negative. On hospital day 2, upon the COVID‐19 nasal swab PCR resulting positive, hydroxychloroquine was initiated. Mycophenolate was discontinued, and dosing of tacrolimus was lowered to target trough levels of 3‐5 ng/mL. Despite remaining afebrile and normotensive throughout hospitalization, she had progressively increasing oxygen requirements. Inflammatory markers collected on hospital day 5 including CRP and ferritin were noted to be significantly elevated at 16.4 mg/dL and 2671 ng/mL, respectively. Intravenous methylprednisolone 1 mg/kg daily was then initiated but no improvement was noted. She also developed acute kidney injury (AKI) with SCr of 1.7 mg/dL and mild transaminitis (AST 73 units/L, ALT 47 units/L). With increasing oxygen requirement to 15 L/min, worsening of inflammatory markers and CXR infiltrates, tocilizumab 400 mg (5 mg/kg) was administered on hospital day 7. An IL‐6 level obtained prior to tocilizumab administration was 241 pg/mL. Subsequently by hospital day 9, oxygen requirements improved to 6 L/min along with improvements in inflammatory markers and CXR infiltrates. On hospital day 11, patient again had increasing oxygen requirements to 11 L/min with up‐trending LDH and worsening CXR infiltrates. Given this, a second dose of tocilizumab 400 mg was administered. Following this dose, patient had progressive improvement in hypoxia, inflammatory markers, as well as infiltrates on CXR. Patient was discharged on day 17 of hospitalization on 4 L/min of supplemental oxygen with resolved AKI and transaminitis. Figure 1 summarizes treatment therapies, oxygen requirement, and inflammatory markers during hospital course.
FIGURE 1.
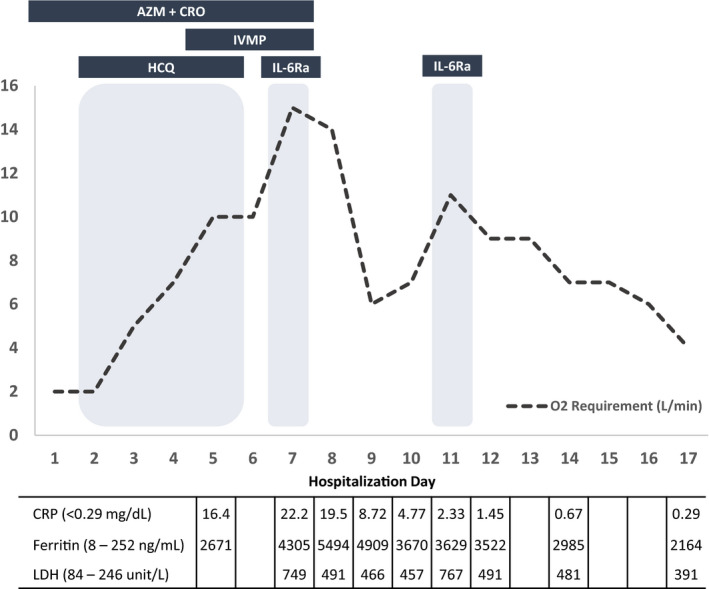
Treatment therapies, oxygen (O2) requirement, and inflammatory markers during hospital course. AZM + CRO = azithromycin and ceftriaxone. IVMP = IV methylprednisolone 1 mg/kg daily. HCQ = hydroxychloroquine 400 mg daily. IL‐6Ra = tocilizumab 400 mg (5 mg/kg)
Our case illustrated the utility of tocilizumab in treating SARS‐CoV‐2 induced inflammatory syndrome in a transplant recipient. Further randomized studies are necessary to confirm the benefit, optimal dosing, and timing of administration of IL‐6Ra therapies in the management of COVID‐19 in transplant recipients.


