Abstract
Among the various rare complications that occur in the treatment of urolithiasis procedures, stent migration is rare, and most of them are into the renal veins or inferior vena cava (IVC). In this report, we describe one case of PCNL stent misplacement into the heart, causing arrhythmia. After identifying the stent migration, based on the location, the DJS was taken out through supraclavicular vein.
1. Introduction
Since its introduction by Ferstrom in 1976,1 nephrolithotripsy (PCNL) has been recognized as one of the most effective surgical methods for the treatment of renal calculi, with the advantages of less trauma, rapid recovery, and high efficiency. However, many complications can occur due to inexperience of the operator. Common complications were bleeding, infection, renal collecting system injury, and vascular injury (only 0.5%).2 At present, there are still very few reports in the literature on the misplacement of indwelling DJS into the vein during PCNL at home and abroad, and there are no reports on the cases of complete entry into the heart. Two cases of double J tube entry into IVC and heart during PCNL admitted to our hospital are reported as follows.
1.1. Case presentation
A 32-year-old male patient was treated with PCNL at our hospital for staghorn calculi in the right kidney. Preoperative routine examinations such as blood routine, biochemistry, and coagulation function showed no abnormalities. Urinary ultrasound, abdominal film, and urinary CT examination showed staghorn calculi in the right kidney. The patient was placed in the prone position. Under the guidance of B- ultrasound, the area between the 11th intercostal space, the right posterior axillary line and the right shoulder line was punctured with a F17.5 puncture needle at 15° - 20° through the right middle calyx. Clear urine outflow was observed after removing the needle core. The zebra guide wire was placed, and the puncture channel was sequentially dilated with an F10–F18 fascial dilator, leaving an F18 sheath. The channel was successfully established, with more bleeding and blurred vision during lithotripsy. The DJS was indwelled immediately after stone removal, without significant resistance when the DJS was inserted, and a 14F balloon catheter was indwelled for drainage.
The patient's condition was stable on the first postoperative day. Vital signs were unremarkable. The drainage liquid of urinary catheter and nephrostomy tube was reddish. On the second postoperative day, the patient complained of palpitation and pain in both lower limbs. Blood pressure was 81/64 mmHg and body temperature was 36.1 °C. ECG monitoring revealed arrhythmia, and the drainage fluid of the urinary catheter and nephrostomy tube was bright red in color. CT revealed that the right renal calculus had been removed and the DJS was located in the right atrium (Fig. 1). Ultrasonography of the deep veins of the lower extremities revealed venous thrombosis of both lower limbs. After removing the thrombus of both lower limbs through the femoral vein under intervention, the DJS was then removed with a snare from the subclavian vein (Fig. 2). The patient's heart rhythm immediately returned to normal, and after symptomatic and supportive treatment. He was recovered and discharged 4 days after surgery.
Fig. 1.
CT finding DJs entering right atrium completely.
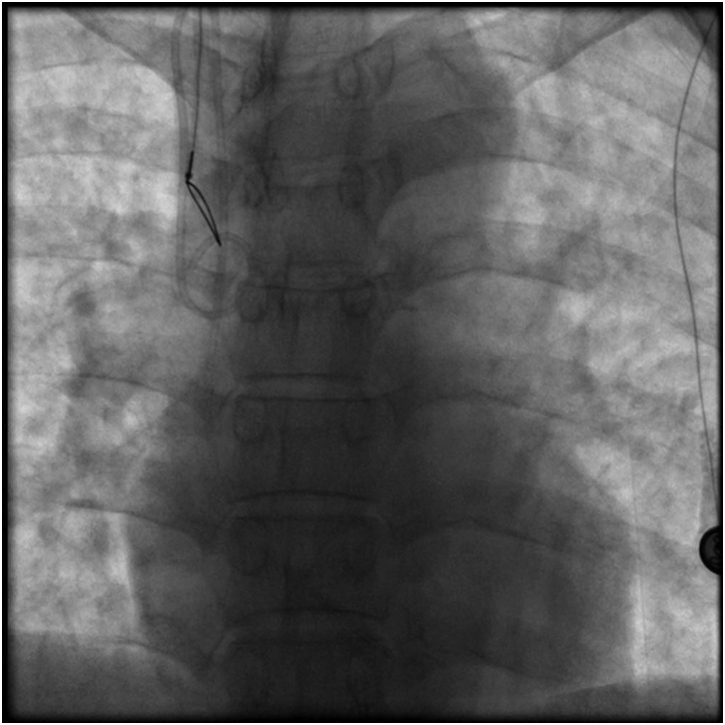
Fig. 2.
Removal of DJs from right atrium through supraclavicular vein.
2. Discussion/conclusion
The DJS is also known as the “JJ stent” and aims to maintain a low-pressure urine flow from the kidney to the bladder. Vascular migration into the IVC in DJS often occurs in URS and is a very rare case in PCNL. Migration to the pulmonary vasculature or heart is considered the most serious complication. There are currently three methods to remove migrated DJS: endovascular, open or endoscopic. The surgical approach depends on the location of the distal coil and the formation of thrombus at the stent and the general condition of the patient.
Tilborghs et al.3 presented a case of misplacement of an indwelling DJS in the URS into the IVC. The stent was removed endoscopically when the distal end of the DJS was determined to be located in the ureter or bladder lumen, thrombosis was ruled out, abdominal CT excluded retroperitoneal bleeding or active bleeding foci (huge trauma of wall is excluded) and no adhesions were present, and the patient's vital signs were stable. The venous valves prevent retrograde flow, while the low pressure in the veins prevents excessive bleeding and allows spontaneous restoration of the damaged vessel wall.
Hajji et al.4 presented the complete entry of DJS into the vessel, respectively. When the patient's condition was stable and retroperitoneal bleeding was excluded by abdominal CT, it was entered from the femoral vein and the case of DJS was removed.
Hastaoglu et al.5 also reported a case of DJS migration to the right ventricle during URS, which was removed by exploration with the establishment of extracorporeal circulation. Because endovascular removal of DJS can lead to tricuspid valve rupture, standard median sternotomy and central cannulation were performed using the dual chamber method, followed by the right atrioventricular resection. With clear dissection, adhesions between DJS and the tricuspid valve are separated.
In the case we treated, DJS had completely entered the right atrium. However, instead of an open procedure, we assessed that the endovascular graft did not damage the heart valve. After the location of the thrombus has been determined, the thrombus is removed and then entered through the supraclavicular vein and the DJS is removed with a snare. In contrast to the above two cases, the harm caused to the patient by the operation was minimized.
There is no single, generally accepted, or recommended modality for removal of displaced DJS. When intravascular migration occurs, the position of the stent should be assessed and thrombosis ruled out by venography. Renal vein and IVC injury are characterized by active bleeding, progressive decrease in blood pressure, and decrease in hemoglobin and saturation through the fistulization channel during and after surgery. The occurrence of the above conditions should be highly suspected. Early intervention is the key to avoid complications.
CRediT authorship contribution statement
Longyuhe Yang: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. Xuede Qiu: Writing - original draft, Writing - review & editing.
Declaration of competing interest
There was no conflict of interest in this article.
Acknowledgements
The authors are grateful to the department of Urology, The Second Affiliated Hospital of Kunming Medical University for their support in this research.
Contributor Information
Longyuhe Yang, Email: 394774084@qq.com.
Xuede Qiu, Email: scottqiucn@126.com.
References
- 1.Ferström I., Johansson B. Percutaneous pyelolithotomy: a new extraction technique. Scand J Urol Nephrol. 1976;10:257–259. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 2.Reynard J., Brewstor S., Biers S. third ed. 2013. Oxford Hand Book of Urology; pp. 774–778. [Google Scholar]
- 3.Tilborghs S., Vaganée D., De Wachter S., Hoekx L. Intravascular double J stent migration: a case report, review, and management algorithm. Urol Ann. 2019;11:93–97. doi: 10.4103/UA.UA_52_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hajji M., Bennani M.S., Bekkali S., Jroundi L. Intracaval migration of ureteral stent. J Belg Soc Radiol. 2015;99:28–30. doi: 10.5334/jbr-btr.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hastaoglu I.O., Tokoz H., Kavlak E., Bilgen F. Double J ureteral stent displaced through the right ventricle. Interact Cardiovasc Thorac Surg. 2014;18:853–854. doi: 10.1093/icvts/ivu037. [DOI] [PubMed] [Google Scholar]