Since 21 February 2020, Italy has developed an outbreak of coronavirus disease 2019 (COVID‐19) by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), with 159 516 confirmed cases until 13 April, mostly concentrated in the Northern part of the country. 1
This situation represents a massive stress for the Italian healthcare system, forcing health authorities to take urgent measures to limit disease spread and potentiate territorial Emergency systems to intercept novel cases. 2 , 3 Public hospitals are subjected to overflow of SARS‐CoV‐2‐infected patients rapidly saturating the bed capacity of Infectious Disease units and ICUs. 2 , 4
To face this challenge, Parma University Hospital, a 1200‐bed facility with a catchment area of >400 000 inhabitants around the city of Parma, Emilia‐Romagna region, has implemented an algorithm, based on the current disease knowledge, 3 to manage the flow of suspected COVID‐19 cases that are triaged at the Emergency Department (ED) (Figure 1). A clinical bed manager, a skilled internist with long clinical expertise and managerial training, is in charge of coordinating the hospital COVID‐19 crisis unit and managing patient flows.
Figure 1.
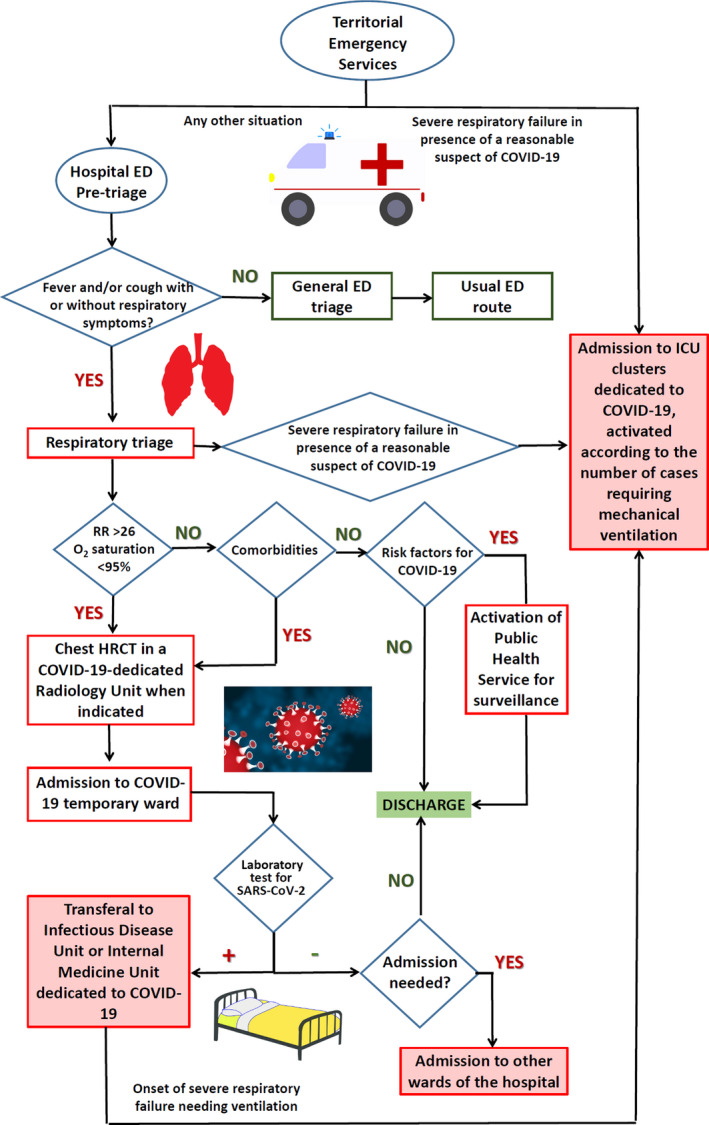
Algorithm of management and flows of suspect COVID‐19 cases adopted in Parma University Hospital. The whole algorithm is superintended by a hospital COVID‐19 crisis unit. Patient flows are managed by a clinician in charge of the crisis unit, with strong expertise in hospital organization and bed managing. COVID‐19‐dedicated wards have been obtained by reconversion of internal medicine, geriatric and rehabilitation wards, whose patients have been transferred to community hospitals or territorial facilities. The involved radiology service is dedicated exclusively to COVID‐19 diagnostics and available 24/7 for the needs of ED, ICU, Infectious Disease or COVID‐19‐dedicated wards. COVID‐19 wards are jointly managed by internal medicine, emergency medicine, geriatrics, intensive care and infectious disease specialists. ED, Emergency Department; HRCT, High‐Resolution Computed Tomography; RR, Respiratory Rate
Pre‐triage is performed in a dedicated area of the ED, one person at a time and immediately at arrival, to avoid possible contacts between positive and negative subjects. Patients with fever and/or respiratory symptoms are addressed to respiratory triage route, separated from the usual ED route, for rapid COVID‐19 screening. Patients with moderate‐severe alterations of respiratory rate and/or O2 saturation are addressed to a COVID‐19‐dedicated radiology unit to perform chest CT. In case of positive or intermediate radiology, patients are admitted to a temporary ward, where laboratory tests for SARS‐CoV‐2 are performed. If positive, patients are transferred either to infectious disease unit or to internal medicine ward clusters exclusively dedicated to COVID‐19 management.
The involved radiology service and the medical wards initially involved in the path are located in the same building. The COVID‐19‐dedicated ward clusters have been activated gradually by progressive reconversion of general medical, geriatric, rehabilitation wards and outpatient areas (total capacity 260 beds). Reconversion of other medical wards of the hospital, located in other buildings, with activation of a dedicated mobile CT, has then been performed with increasing patient flows (final capacity >600 beds).
ICU transferal is possible at every step. COVID‐19‐dedicated ICU clusters have been progressively activated by reconversion of post‐surgical and specialist ICU services (60 beds).
This model shares some common features, including pre‐triaging and reconversion of wards, with models implemented in other hospitals of Northern Italy. 5 However, the inclusion of chest CT at an early stage of patient management and clusterization of medical and ICU beds represent the main points of strength and novelty of the present model, ameliorating clinical management of patients and facilitating hospital organization in a moment of evolving crisis.
COVID‐19 outbreak is challenging for hospital care. Development of lean, adaptable and multidisciplinary algorithms for managing patient flows may be pivotal for the local governance of COVID‐19 pandemic.
CONFLICT OF INTEREST
All the authors report no competing interests.
AUTHOR CONTRIBUTIONS
Dr Ticinesi had full access to all of the data in the study and takes the responsibility for the integrity of data. Concept and design: Meschi, Rossi, Volpi, Brianti, Fabi. Drafting of the manuscript and literature review: Ticinesi. Critical revision of the manuscript for important intellectual content: Nouvenne.
ACKNOWLEDGEMENTS
Part of the images are distributed under Creative Commons Licence and can be freely available at the following links: https://smart.servier.com/ and https://pixabay.com.
Tiziana Meschi and Sandra Rossi share first authorship.
REFERENCES
- 1. Italian Ministry of Health Covid‐19 Bulletin, April 13th 2020. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=italiano%26id=5351%26area=nuovoCoronavirus%26menu=vuoto. Accessed April 14, 2020.
- 2. Carinci F. Covid‐19: decentralisation, and the hunt for patient zero. BMJ. 2020;19(368):bmj.m799. [DOI] [PubMed] [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spina S, Marrazzo F, Migliari M, et al. The response of Milan's Emergency Medical System to the COVID‐19 outbreak in Italy. Lancet. 2020;395(10227):e49‐e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zangrillo A, Beretta L, Silvani P, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID‐19 pandemic emergency. Crit Care Resusc. 2020; In press April 1. [DOI] [PMC free article] [PubMed] [Google Scholar]


