Abstract
Background
Acute viral upper respiratory tract infections are the most common cause of chronic olfactory dysfunction. In light of the seasonality of numerous viruses, the question arises as to whether the frequency and magnitude of postviral olfactory disorders (PVODs) are similarly seasonal. We sought to determine whether olfactory deficits due to influenza and non–influenza‐related viruses (I‐PVODs and NI‐PVODs) vary in frequency or magnitude across seasons in a North American population and whether they are more prevalent or produce more severe olfactory dysfunction during colder months when host susceptibility may be increased.
Methods
This was a retrospective study of 587 patients presenting to an academic smell and taste center with either I‐PVOD–related or NI‐PVOD–related olfactory deficits. Chi‐square and analysis of covariance (age = covariate) compared dysfunction prevalence frequencies and scores on the University of Pennsylvania Smell Identification Test (UPSIT) across calendar months and between months with the coldest and warmest air temperatures.
Results
For I‐PVOD–related cases, both the prevalence and magnitude of smell dysfunction were highest in the colder months. However, for NI‐PVOD–related cases, prevalence was higher in warmer months but, paradoxically, the magnitude of dysfunction was higher in colder months.
Conclusion
This study shows that seasonal variations occur in both the prevalence and magnitude of PVOD‐related olfactory deficits in a North American population, and that such variations differ between NI‐PVOD and I‐PVOD cases. The findings suggest multiple viruses are involved in producing PVOD‐related olfactory deficits.
Keywords: olfaction, influenza, viruses, UPSIT, seasonality, postviral olfactory disorder, upper respiratory infections
Olfactory loss can be devastating to patients, significantly altering the flavor of foods and beverages, their nutrition, and their safety. Although loss of smell function can arise from head trauma, 1 exposures to toxic agents, 2 and a number of diseases, 3 including Alzheimer's and Parkinson's, 4 acute viral upper respiratory infections that damage the olfactory neuroepithelium are the major cause of chronic olfactory dysfunction, a condition termed postviral olfactory disorder (PVOD). 5 , 6 , 7 Importantly, a number of viruses have the propensity to invade the brain via the olfactory fila. 8 , 9
PVOD joins a chorus of other disorders with seasonal patterns, including tuberculosis, measles, diphtheria, chickenpox, and cholera. 10 Among the multiple hypotheses proposed to explain such seasonal variations are alterations in immune system reactivity, spreading of germs via winter indoor crowding, changes in weather (including humidity), and variations in the presence of specific pathogens. Based on seasonality and antibody titers, Sugiura et al., 11 in a pioneering study, implicated parainfluenza virus type 3 (PIV‐3) as the primary, if not sole, cause of PVOD. These investigators measured antibody titers of adenoviruses, PIV‐3, herpes (simplex, zoster) and parainfluenza type 1, 2, and 3 viruses in 127 patients with PVOD, as well as in 28 patients with head trauma and in 218 patients with rhinosinusitis. The vast majority of PVOD patients had contracted their illness in the warmer months and all exhibited elevated PIV‐3 titers, unlike other viruses that were elevated only in some patients. However, despite the fact that the PIV‐3 titers of the PVOD patients were higher than those in the posttraumatic and rhinosinusitis groups, they were “not significantly so” (p. 192), 11 throwing into question the issue of causality. Surprisingly, influenza and respiratory syncytial virus were ruled out as major causes of PVOD because they were “isolated only in winter, and their seasonal pattern of prevalence is thus opposite to that of PVOD” (p. 192). 11
Two subsequent studies have similarly noted seasonal patterns in the frequency of PVOD, again suggesting primary involvement of viruses present during warmer months, although the patterns vary somewhat between studies, and viruses other than PIV‐3 have been implicated. 12 In most countries, parainfluenza and rhinoviruses are more prevalent in warmer months, whereas coronaviruses, influenza viruses, and respiratory syncytial viruses are more common in colder months. Like Sugiura et al. 11 in Japan, Wang et al. 13 noted peaks in PVOD in June and July for 25 patients in Korea, whereas Konstantinidis et al. 14 found, in a study of 457 German patients, that such peaks occurred in March and May. Relatively few cases were observed in winter months, and no study has differentiated between patients with PVOD due to influenza and PVOD due to non‐influenza causes. Because, at least in North America, influenza is most prevalent in winter months, one might expect to see influenza‐related PVOD peaks in winter, rather than spring and summer. However, this has never been documented.
The present study employed a large university‐based smell and taste center database to retrospectively assess the monthly prevalence and degree of PVOD in patients whose smell dysfunction was secondary to influenza‐related PVODs (I‐PVODs) or non–influenza‐related PVODs (NI‐PVODs). The goals were to determine whether seasonal fluctuations in both prevalence and the magnitude of dysfunction were evident in this olfactory‐compromised patient population and whether such fluctuations, if present, differed between patients with influenza and non‐influenza viral etiologies. Specific attention was paid to deficits occurring during the coldest and warmest months. Gender was of interest because the intensity and prevalence of viral infections are typically higher in men than in women, whereas disease outcome is often worse for women. 15
Patients and methods
Study population
Data from 587 patients who had presented to the University of Pennsylvania Smell and Taste Center with chronic smell problems attributed to either an I‐PVOD or a NI‐PVOD were included in the study. These cases were identified in a chart review of 4950 Center patients as having PVOD‐related deficits, as defined by Sugiura et al. 11 and in having the month and year of the viral contraction clearly indicated. I‐PVOD was differentiated from NI‐PVOD based upon the patient reports of diagnoses at the time of symptom onset, including such factors as fever, muscle aches, fatigue, symptom severity, and congestion. 16 In addition to the olfactory testing described in the following section, information regarding each person's current health, medical history, and chemosensory complaint was obtained from the patient's intake interview, physician reports, and a 270‐item intake questionnaire completed by the patient prior to their visit to the Center. Details of this intake questionnaire can be found in Deems et al. 5 Medical information included a history of physician visits and physical examinations, as well as, in some cases, specific test results. The age and gender distributions of the study group are listed in Table 1. This research was approved by the Institutional Review Board of the University of Pennsylvania's Office of Regulatory Affairs and was performed in accordance with the ethical principles of the Declaration of Helsinki. 17
TABLE 1.
Patient demographics*
| Characteristic | Total | NI‐PVOD | NI‐PVOD (cold) | NI‐PVOD (warm) | I‐PVOD | I‐PVOD (cold) | I‐PVOD (warm) |
|---|---|---|---|---|---|---|---|
| Patient (n) | 587 | 511 | 271 | 240 | 76 | 55 | 21 |
| Age (years), mean ± SD | 56.03 ± 12.61 | 55.80 ± 12.61 | 56.64 ± 12.07 | 54.85 ± 13.14 | 57.61 ± 12.58 | 59.07 ± 12.06 | 53.76 ± 13.36 |
| Gender, n (%) | |||||||
| Male | 199 (33.9) | 178 (34.8) | 179 (66.1) | 154 (64.2) | 21 (27.6) | 16 (29.1) | 5 (23.8) |
| Female | 388 (66.1) | 333 (65.2) | 92 (33.9) | 86 (35.8) | 55 (72.4) | 39 (70.9) | 16 (76.2) |
*See “Procedure” section of text for definition of cold and warm seasons.
I‐PVOD = influenza‐related postviral olfactory disorder; NI‐PVOD = non–influenza‐related postviral olfactory disorder; SD = standard deviation.
Olfactory test
Olfaction was assessed using the University of Pennsylvania Smell Identification Test (UPSIT). 18 This widely‐employed 40‐odorant test focuses on the comparative ability of subjects to identify odorants at the suprathreshold level. It is comprised of 4 envelope‐sized booklets, each containing 10 “scratch and sniff” odorants embedded in microcapsules individually positioned on brown strips at the bottom of each booklet page. The test‐retest reliability is high (r = 0.94), 18 , 19 and the test has been shown to be sensitive to a wide range of diseases and disorders. 20 The specifics and criteria for item selection and standardization of this test are described elsewhere. 18
Procedure
The patient files were reviewed to identify persons whose olfactory dysfunction was clearly attributed to an I‐PVOD or a NI‐PVOD infection. The monthly frequencies and UPSIT scores were recorded and analyzed, as were the frequencies and UPSIT scores for the coldest and warmest months, as defined by the National Oceanic and Atmospheric Administration (NOAA) average air temperature for Philadelphia, PA (ie, November through April vs May through October, respectively). 21 Differences in prevalence rates among the months were assessed using chi‐square analysis. Differences in UPSIT scores were examined using analysis of covariance (ANCOVA) separately performed on the data for the I‐PVOD and NI‐PVOD cases. In these analyses, the within subject factor was viral onset month (or warm/cold months) and the between subject factor was subject gender. 22 Age served as the covariate to control for the well‐established influences of age on olfactory test scores. 23
Results
Seasonal fluctuations in reported infections
Figure 1 presents the cumulative reported monthly frequencies for the I‐PVOD and NI‐PVOD groups. For these groups, onset years ranged from 1973 to 2018, although data collection began in 1980. A peak in prevalence of I‐PVOD was found to occur during colder, not warmer, months, with the highest frequencies occurring during December, January, February, and March. Despite the small sample size (n = 76), the frequencies of these months were significantly higher than those of the remaining months, accounting for over one‐half (49/76; 65%) of all of the frequencies (χ2 [1] = 13.93; p = 0.0002).
FIGURE 1.
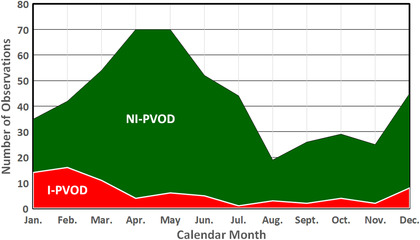
Monthly cumulative cases of I‐PVOD and NI‐PVOD. Cases reflect frequencies from 1973 to 2018. I‐PVOD = influenza‐related postviral olfactory disorder; NI‐PVOD = non–influenza‐related postviral olfactory disorder.
For the NI‐PVOD group, the highest frequencies consistently occurred in March through June, peaking in April and May for both men and women. It is noteworthy that nearly one‐half (246/511; 48%) of the cases occurred within these 4 months (compared to all other months, χ2 [1] = 22.80; p < 0.0001), and that each of these months’ frequencies differed significantly from those of August, September, October, and November (all ps < 0.01). In contrast to the I‐PVOD study group, the frequencies did not differ significantly between those who contracted their NI‐PVOD during the coldest 6 months (n = 271) and those who contracted their NI‐PVOD during the warmer 6 months (n = 240) (p = 0.17).
Seasonal fluctuations in UPSIT scores
In the I‐PVOD group, no significant differences were apparent in UPSIT scores between the colder and warmer months (p = 0.67) (Table 2). Unfortunately, the small monthly sample sizes precluded meaningful comparisons among the individual months. In contrast, the UPSIT scores of the NI‐PVOD group were 6.56% lower during the colder than during the warmer months (respective means ± SDs = 23.20 ± 8.34 and 24.83 ± 8.08; F [1, 506] = 4.415; p = 0.036; η2 = 0.018). In this analysis, the covariate of age was significant (p = 0.002; 95% CI, 54.70 to 56.89), but the factor of gender was not (p > 0.15). The lowest UPSIT scores occurred in December and January, in marked contrast to the high incident frequencies that occurred from March through June (Table 2). Post hoc analyses found December UPSIT scores differed significantly from those of February, May, June, July, and September. January UPSIT scores followed suit, significantly differing from February, May, June, July, and September UPSIT scores. The p values and 95% CIs for these comparisons are shown in Table 3.
TABLE 2.
Monthly UPSIT scores*
| Parameter | January | February | March | April | May | June | July | August | September | October | November | December | Cold | Warm |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NI‐PVOD | ||||||||||||||
| n | 35 | 42 | 54 | 70 | 70 | 52 | 44 | 19 | 26 | 29 | 25 | 45 | 271 | 240 |
| UPSIT score, mean ± SD | 20.54 ± 9.68 | 25.24 ± 8.26 | 24.02 ± 7.41 | 23.51 ± 7.91 | 24.96 ± 8.29 | 25.23 ± 7.00 | 25.39 ± 8.90 | 24.63 ± 8.12 | 25.69 ± 8.25 | 22.41 ± 8.19 | 24.56 ± 10.07 | 21.16 ± 7.144 | 23.20 ± 8.34 | 24.83 ± 8.08 |
| I‐PVOD | ||||||||||||||
| n | 14 | 16 | 11 | 4 | 6 | 5 | 1 | 3 | 2 | 4 | 2 | 8 | 55 | 21 |
| UPSIT score, mean ± SD | 22.86 ± 9.29 | 25.50 ± 8.21 | 25.36 ± 6.59 | 21.25 ± 1.26 | 26.83 ± 7.63 | 21.60 ± 5.03 | 30 ± – | 18.67 ± 7.51 | 30.50 ± 13.44 | 28.25 ± 4.11 | 27.50 ± 0.71 | 23.88 ± 10.43 | 24.33 ± 8.00 | 25.19 ± 7.28 |
*Also included are cold and warm month averages. See “Procedure” section of text for definition of cold and warm seasons.
I‐PVOD = influenza‐related postviral olfactory disorder; NI‐PVOD = non–influenza‐related postviral olfactory disorder; SD = standard deviation; UPSIT = University of Pennsylvania Smell Identification Test.
TABLE 3.
Post hoc comparisons among months for UPSIT scores including CIs and p values*
| Parameter | Difference | 95% CI | p | η2 |
|---|---|---|---|---|
| NI‐PVOD | ||||
| December vs | ||||
| February | 4.08 | 0.73–7.43 | 0.018 | 0.037 |
| May | 3.74 | 0.72–6.76 | 0.016 | 0.036 |
| June | 4.07 | 1.16–6.98 | 0.007 | 0.025 |
| July | 4.23 | 0.78–7.68 | 0.017 | 0.034 |
| September | 4.53 | 0.72–8.34 | 0.020 | 0.049 |
| January vs | ||||
| February | 4.70 | 0.63–8.77 | 0.024 | 0.052 |
| May | 4.36 | 0.76–7.96 | 0.018 | 0.050 |
| June | 4.69 | 1.13–8.25 | 0.010 | 0.038 |
| July | 4.85 | 0.68–9.02 | 0.023 | 0.052 |
| September | 5.15 | 0.43–9.87 | 0.033 | 0.071 |
| Cold vs | ||||
| Warm | 1.63 | 0.20–3.06 | 0.026 | 0.018 |
| I‐PVOD | ||||
| April vs | ||||
| October | 6.74 | 1.48–12.00 | 0.020 | 0.003 |
| November | 5.99 | 3.23–8.75 | 0.004 | 0.004 |
| Cold vs | ||||
| Warm | 0.86 | −3.13 to 4.85 | 0.67 | <0.001 |
*Means are presented in Table 2.
η2 = ratio of effect to total variance; CI = confidence interval; I‐PVOD = influenza‐related postviral olfactory disorder; NI‐PVOD = non–influenza‐related postviral olfactory disorder; UPSIT = University of Pennsylvania Smell Identification Test.
Relationship between time of symptom onset and olfactory testing
To determine whether the time between symptom onset and the time of UPSIT testing might be meaningfully associated and therefore could conceivably confound comparability among patients, we computed both Pearson and Spearman correlation coefficients between these variables. No significant associations were evident, suggesting such confounding was not present (whole group Pearson and Spearman r values = 0.053 and −0.052, ps > 0.2; influenza group r values = −0.01 and 0.001; ps > 0.2; non‐influenza group r values = −0.07 and −0.06, ps > 0.2).
Discussion
This study is the largest to date to assess seasonal variations in the prevalence and magnitude of viral‐induced olfactory deficits. In addition to demonstrating such variations in a North American population, it is the first study to determine whether seasonal differences exist between I‐PVODs and NI‐PVODs. Most notably, it found that I‐PVOD prevalence peaks in January and February, not in March through June, as is the case with NI‐PVOD. Remarkably, greater dysfunction was also observed for those NI‐PVOD cases that occur in the winter months. The NI‐PVOD frequency peaks we found in March through June overlap with the PVOD frequencies reported by Konstantinidis et al. 14 in Germany (March and May) and Sugiura et al. 11 in Japan (June), and partially overlap the months of highest prevalence reported by Wang et al. 13 in Korea (June and July). Given that these studies did not distinguish between I‐PVOD and NI‐PVOD cases, their data likely reflect a combination of these 2 types of PVOD.
Our finding of the disassociation between the months in which NI‐PVOD is most frequent and the months in which the greatest NI‐PVOD olfactory dysfunction occurs raises several questions. Are some viruses that are more common in warmer months more potent or virulent in their ability to damage the olfactory system in colder months? Is the olfactory neuroepithelium more susceptible to greater viral damage during colder months? With regard to the latter, host susceptibility may well play a role. It is well established that even short‐term inspiration of cold air dries the nasal epithelium (and presumably the olfactory epithelium) and decreases its temperature. 24 Electrophysiological studies show that olfactory receptor cells are sensitive to temperature and can be damaged by desiccation. 25 , 26 Moreover, within the nasal epithelium, decreased temperature adversely alters mucociliary clearance, phagocytic activity, and immune responses, thereby prolonging viral residence. 27 , 28 , 29 That being said, it must be acknowledged that the reasons for seasonal fluctuations in viral activity are likely multifactorial and enigmatic. 30
Several investigators have suggested that the PIV‐3 virus is the primary or even sole cause of PVOD. As noted in the Introduction, Sugiura et al. 11 concluded, on the basis of the study of 127 persons with olfactory loss following a viral infection, that PIV‐3 was the cause of the olfactory loss, and that influenza, respiratory syncytial virus (RSV), or herpes viruses were not involved. The majority of cases occurred during warmer months. Following up on this work, Wang et al. 13 identified PIV‐3 in 88% of cases of PVOD, again largely sampled during warmer months. Based on these observations, Tian et al. 31 used the Sendai virus, a murine virus analogous to PIV, as a model to study PVOD in mice. However, despite such observations, the role of PIV‐3 remains unclear. Indeed, in contrast to the findings of Sugiura et al. 11 findings, Suzuki et al. 12 did not find PIV‐3 in a study examining the nasal discharge of 24 patients with PVOD. Instead, they detected rhinoviruses, coronaviruses, parainfluenza virus (PIV‐2), and Epstein‐Barr virus. Moreover, PIV‐3 only accounts for ∼5% of all patients suffering from upper respiratory infections, 32 and Sugiura et al. 11 did not examine rhinoviruses or coronaviruses—viruses that are estimated to cause anywhere from 40% to 75% of all upper respiratory infections. 32 According to Heikkinen and Jãrvinen, 32 an additional 5% to 15% of upper respiratory infections are caused by influenza viruses and 5% to 10% by RSV and parainfluenza viruses. The remaining 20% to 30% are unknown. Although PIV‐3 peaks in warmer months, in accord with our higher observed frequency of NI‐PVOD–related smell deficits, this peak does not correlate with our observed increase in the magnitude of NI‐PVOD–related olfactory dysfunction during the colder months, nor does it explain the increased frequency of I‐PVOD we observed during the colder months.
No differences were found in this study between the male and female patients for either the frequency or the magnitude of the virus‐related olfactory disturbances. Although exposure rates to a number of viruses, notably influenza A viruses, are commonly higher in men than in women, women are twice as likely than men to die from such exposures. 15 Additionally, women generally perform better than men on a variety of olfactory tests. 33 From such observations, one might have expected to see differences in UPSIT scores between the men and women of this study, but this did not occur. It is possible that the significant damage induced by the viruses diminished any gender differences present prior to the viral infections. Another possibility is that the better initial olfactory function of women was protective to some extent and therefore mitigated any demonstrable gender differences related to differential involvement of the viruses.
Our study has both strengths and weaknesses. Among its strengths are its large sample size, questionnaire‐based information regarding symptom nature and onset, and the use of a very reliable and sensitive test of olfactory function. With a sample size of 587, this is the largest study to date to examine the seasonality of PVOD and its effect on olfactory function. Another strength is the distinction that was made between PVODs caused by influenza and PVODs caused by other viruses, given their different frequency patterns throughout the year. This is also the first study to assess whether gender might impact either the frequency or the magnitude of seasonal changes in smell function of persons whose smell has been compromised by a PVOD. Among the study's weaknesses are its reliance on self‐report, no isolation of any virus, and the relatively small sample size of the I‐PVOD group. It should be pointed out, however, that careful selection was made of patients whose dates of onset and nature of their upper respiratory infections were evident in their written intake questionnaires and medical records. The intake questionnaires were filled out in advance to their arrival to the clinic, allowing the patients time to consult their personal and medical records and thereby reducing the chance of misreporting. Additionally, during the initial intake interview, a detailed exploration of potential causes is made and discrepancies corrected. Nonetheless it is noteworthy that some studies suggest that using such symptoms as cough and fever to differentiate between influenza and non‐influenza viral cases has at best only a positive predictive value of ∼80%. 16 That being said, the accuracy of our assigning patients to the I‐PVOD and NI‐PVOD classes is supported by the fact that the proportion of I‐PVOD cases in our sample (76/587; 12.9%) is essentially the same as that estimated in the general population. 34 Although there were no attempts to isolate potential causative viruses in this retrospective study, such isolations would be expensive, time consuming, and best completed by the clinician who is initially consulted at the time of the infection. Because most Center patients have been referred weeks, months, or even years after their problem onset, collection of such data would be generally futile.
Conclusion
Olfaction is frequently damaged, sometimes permanently, by virus‐related infections. This study has shown that seasonal variations occur in both the prevalence and the magnitude of PVOD‐related olfactory deficits in a North American population. Additionally, it shows that such variations differ between NI‐PVOD and I‐PVOD cases. Overall, the findings suggest that multiple viruses are involved in producing PVOD‐related olfactory deficits.
Acknowledgments
The development of the database upon which analyses of this study were dependent was initially supported by PO1 DC 00161 from the National Institute on Deafness and Other Communication Disorders as well as funds from the Department of Otorhinolaryngology: Head and Neck Surgery. We thank Ms. Crystal Wylie for her help in the preparation of the manuscript.
How to Cite this Article:Potter MR, Chen JH, Lobban N‐S, Doty RL. Olfactory dysfunction from acute upper respiratory infections: relationship to season of onset. Int Forum Allergy Rhinol. 2020;10:706–712.
Funding sources for the study: National Institutes of Health (NIH) (National Institute on Deafness and Other Communication Disorders [NIDCD] PO1 DC 00161); Department of Otorhinolaryngology: Head and Neck Surgery.
Potential conflict of interest: R.L.D. is a major shareholder in Sensonics International, the manufacturer and distributor of the olfactory test employed in this study. The other authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Schofield P, Doty RL. The influence of head injury on olfactory and gustatory function. Handb Clin Neurol. 2019;164:409‐429. [DOI] [PubMed] [Google Scholar]
- 2. Genter MB, Doty RL. Toxic exposures and the senses of taste and smell. Handb Clin Neurol. 2019;164:389‐408. [DOI] [PubMed] [Google Scholar]
- 3. Doty RL. Systemic diseases and disorders. Handb Clin Neurol. 2019;164:361‐387. [DOI] [PubMed] [Google Scholar]
- 4. Doty RL, Hawkes CH. Chemosensory dysfunction in neurodegenerative diseases. Handb Clin Neurol. 2019;164:325‐360. [DOI] [PubMed] [Google Scholar]
- 5. Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991;117:519‐528. [DOI] [PubMed] [Google Scholar]
- 6. Harris R, Davidson TM, Murphy C, Gilbert PE, Chen M. Clinical evaluation and symptoms of chemosensory impairment: one thousand consecutive cases from the Nasal Dysfunction Clinic in San Diego. Amer J Rhinol. 2006;20:101‐108. [PubMed] [Google Scholar]
- 7. Pellegrino R, Sinding C, de Wijk RA, Hummel T. Habituation and adaptation to odors in humans. Physiol Behav. 2017;177:13‐19. [DOI] [PubMed] [Google Scholar]
- 8. Jang H, Boltz D, Sturm‐Ramirez K, et al. Highly pathogenic H5N1 influenza virus can enter the central nervous system and induce neuroinflammation and neurodegeneration. Proc Natl Acad Sci U S A. 2009;106:14063‐14068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Doty RL. The olfactory vector hypothesis of neurodegenerative disease: is it viable? Ann Neurol. 2008;63:7‐15. [DOI] [PubMed] [Google Scholar]
- 10. Grassly NC, Fraser C. Seasonal infectious disease epidemiology. Proc Biol Sci. 2006;273:2541‐2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sugiura M, Aiba T, Mori J, Nakai Y. An epidemiological study of postviral olfactory disorder. Acta Otolaryngol. 1998;191‐196. [DOI] [PubMed] [Google Scholar]
- 12. Suzuki M, Saito K, Min WP, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117:272‐277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang JH, Kwon HJ, Jang YJ. Detection of parainfluenza virus 3 in turbinate epithelial cells of postviral olfactory dysfunction patients. Laryngoscope. 2007;117:1445‐1449. [DOI] [PubMed] [Google Scholar]
- 14. Konstantinidis I, Haehner A, Frasnelli J, et al. Post‐infectious olfactory dysfunction exhibits a seasonal pattern. Rhinology. 2006;44:135‐139. [PubMed] [Google Scholar]
- 15. Klein SL. Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. Bioessays. 2012;34:1050‐1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Eccles R. Understanding the symptoms of the common cold and influenza. Lancet Infect Dis. 2005;5:718‐725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191‐2194. [DOI] [PubMed] [Google Scholar]
- 18. Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav. 1984;32:489‐502. [DOI] [PubMed] [Google Scholar]
- 19. Doty RL, Newhouse MG, Azzalina JD. Internal consistency and short‐term test‐retest reliability of the University of Pennsylvania Smell Identification Test. Chem Senses. 1985;10:297‐300. [Google Scholar]
- 20. Hawkes CH, Doty RL. Smell and Taste Disorders. Cambridge: Cambridge University Press; 2018. [Google Scholar]
- 21. National Oceanic and Atmospheric Administration (NOAA). National Weather Service . NOWData. NOAA Online Weather Data. Washington, DC: National Weather Service Office, NOAA; 2018. https://w2.weather.gov/climate/xmacis.php?wfo=phi. Accessed February 22, 2019. [Google Scholar]
- 22. Wilkinson L. SYSTAT: the System for Statistics. Evanston, IL: SYSTAT, Inc.; 1990. [Google Scholar]
- 23. Doty RL, Shaman P, Applebaum SL, Giberson R, Siksorski L, Rosenberg L. Smell identification ability: changes with age. Science. 1984;226:1441‐1443. [DOI] [PubMed] [Google Scholar]
- 24. Koskela HO. Cold air‐provoked respiratory symptoms: the mechanisms and management. Int J Circumpolar Health. 2007;66:91‐100. [DOI] [PubMed] [Google Scholar]
- 25. Kashiwayanagi M, Horiuchi M, Kurihara K. Differential ion dependence of frog olfactory responses to various odorants. Comp Biochem Physiol A Comp Physiol. 1991;100:287‐292. [DOI] [PubMed] [Google Scholar]
- 26. Grubb BR, Rogers TD, Kulaga HM, et al. Olfactory epithelia exhibit progressive functional and morphological defects in CF mice. Am J Physiol Cell Physiol. 2007;293:C574‐C583. [DOI] [PubMed] [Google Scholar]
- 27. Eccles R, Wilkinson JE. Exposure to cold and acute upper respiratory tract infection. Rhinology. 2015;53:99‐106. [DOI] [PubMed] [Google Scholar]
- 28. Proctor DF. The mucociliary system. In: Proctor DF, ed. The Nose, Upper Airway Physiology and the Atmospheric Environment. New York: Elsevier; 1982:245‐278. [Google Scholar]
- 29. Djaldetti M, Salman H, Bergman M, Djaldetti R, Bessler H. Phagocytosis—the mighty weapon of the silent warriors. Microsc Res Tech. 2002;57:421‐431. [DOI] [PubMed] [Google Scholar]
- 30. Lofgren E, Fefferman NH, Naumov YN, Gorski J, Naumova EN. Influenza seasonality: underlying causes and modeling theories. J Virol. 2007;81:5429‐5436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tian J, Pinto JM, Cui X, et al. Sendai virus induces persistent olfactory dysfunction in a murine model of PVOD via effects on apoptosis, cell proliferation, and response to odorants. PLoS One. 2016;11:e0159033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Heikkinen T, Jãrvinen A. The common cold. Lancet. 2003;361:51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Doty RL, Cameron EL. Sex differences and reproductive hormone influences on human odor perception. Physiol Behav. 2009;97:213‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis. 2018;66:1511‐1518. [DOI] [PMC free article] [PubMed] [Google Scholar]


