To the Editor,
Coronavirus disease 2019 (COVID‐19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and currently considered by the World Health Organization to be a pandemic with more than one million of confirmed cases and almost 57 000 deaths worldwide. 1 , 2 Cytokines are important mediators of the inflammatory response. While some cytokines promote inflammation such as IL‐6, IL‐8, TNF‐α, IL‐1, IFN‐γ, and TGF‐β, others such as IL‐4 and IL‐10 have an anti‐inflammatory effect. It has been suggested that patients with severe COVID‐19, resembling SARS and MERS patients, may have a cytokine storm syndrome characterized by an increase in IL‐2, IL‐7, G‐CSF, CXCL10, MCP‐1, MIP‐1α, TNF‐α, and IL‐6, suggesting that mortality could be due to viral hyperinflammation that exacerbates lung damage. 3 In this study, a meta‐analysis was performed to investigate whether the IL‐6/IFN‐γ ratio can help predict clinical severity in patients with COVID‐19.
We conducted an electronic search in different search engines that included Medline (PubMed interface), Scopus, and Google Scholar, using the keywords "INF‐gamma+COVID‐19" OR "IL‐6+ COVID‐19" OR "Severe 2019‐nCoV" OR "Severe COVID‐19" without date (until 5 April 2020) or language restrictions. The title, abstract and full text of all the articles identified according to these search criteria were analyzed, considering for our meta‐analysis only those that reported data from both parameters, IL‐6 and IFN‐γ, in COVID‐19 patients with or without the severe disease.
Only three studies were considered for our analysis. 4 , 5 , 6 The mean and standard deviation were calculated from the median, range, and sample size as previously described. 7 For all studies, cytokines were measured using cytometric bead arrays and the units used for both parameters were pg/mL. Meta‐analysis was performed using Comprehensive Meta‐Analysis Software version 3 (Biostat, Englewood, NJ 2013) calculating the standardized mean difference (SMD) and the 95% confidence interval (95% CI) of IL‐6/INF‐γ ratio in COVID‐19 patients with or without the severe disease.
All studies were carried out in Chinese hospital centers and included a total number of 264 patients, of whom 123 had severe disease (46.59%) and the sample size ranged from 43 to 148 patients. Because heterogeneity (I 2 statistics) exceeded 50%, a random‐effects model was used. The IL‐6/IFN‐γ ratio was found to be significantly increased in COVID‐19 patients with severe disease (SMD = 0.739; 95% CI = 0.131‐1.383). More details of our meta‐analysis are presented in Figure 1.
Figure 1.
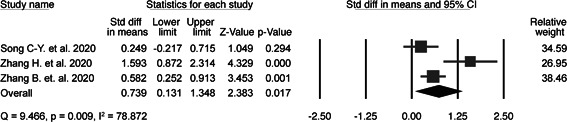
Forest plot of standardized mean difference (SMD) and 95% confidence interval (95% CI) in IL‐6/IFN‐γ ratio between COVID‐19 patients with or without severe disease
During SARS‐CoV‐2 infection, both the innate and adaptive immune responses are required for successful virus clearance and must be adequately controlled to minimize immunopathological damage. The interaction between IFN‐γ and IL‐6/sIL‐6R signaling contributes to rapid recruitment and timely neutrophil clearance, thereby controlling infection and resolution of acute inflammation as well as the transition between innate and acquired immunity. 8 Here, we find that severe COVID‐19 patients have a higher IL‐6/IFN‐γ ratio than moderate patients, which could be related to an enhanced cytokine storm favoring lung damage. Thus, this clinical tool can provide valuable information for the prognosis of severe disease in COVID‐19 cases. Furthermore, some studies have associated higher IL‐6 levels with severe patients and patients who died, 9 , 10 whereas the expression of IFN‐γ tends to be slightly lower in severe cases than in moderate cases, mainly due to the decrease in CD4+, CD8+, and NK lymphocytes. 11
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENTS
Francisco Alejandro Lagunas‐Rangel is the recipient of a doctoral scholarship (application number 2018‐000012‐01NACF‐07226) from the National Council of Science and Technology, CONACyT.
REFERENCES
- 1. Coronavirus Disease 2019. (COVID‐19) Situation Report‐75. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200404‐sitrep‐75‐covid‐19.pdf?sfvrsn=99251b2b_2. Accessed April 5, 2020.
- 2. Zhang W, Zhao Y, Zhang F, et al. The use of anti‐inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID‐19): the perspectives of clinical immunologists from China. Clin Immunol. 2020;214:108393. 10.1016/j.clim.2020.108393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;6736(20):19‐20. 10.1016/S0140-6736(20)30628-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Song C‐Y, Xu J, He J‐Q, Lu Y‐Q. COVID‐19 early warning score: a multi‐parameter screening tool to identify highly suspected patients. medRxiv. 2020. 10.1101/2020.03.05.20031906 [DOI] [Google Scholar]
- 5. Zhang H, Wang X, Fu Z, et al. Potential factors for prediction of disease severity of COVID‐19 patients. medRxiv. 2020. 10.1101/2020.03.20.20039818 [DOI] [Google Scholar]
- 6. Zhang B, Zhou X, Zhu C, et al. Immune phenotyping based on neutrophil‐to‐lymphocyte ratio and IgG predicts disease severity and outcome for patients with COVID‐19. medRxiv. 2020. 10.1101/2020.03.12.20035048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13. 10.1186/1471-2288-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McLoughlin RM, Witowski J, Robson RL, et al. Interplay between IFN‐γ and IL‐6 signaling governs neutrophil trafficking and apoptosis during acute inflammation. J Clin Invest. 2003;112(4):598‐607. 10.1172/JCI200317129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020:1‐10. 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen G, Wu D, Guo W, et al. Clinical and immunologic features in severe and moderate Coronavirus Disease 2019. J Clin Invest. 2020;130(5):2620–2629. 10.1172/JCI137244 [DOI] [PMC free article] [PubMed] [Google Scholar]


