1.
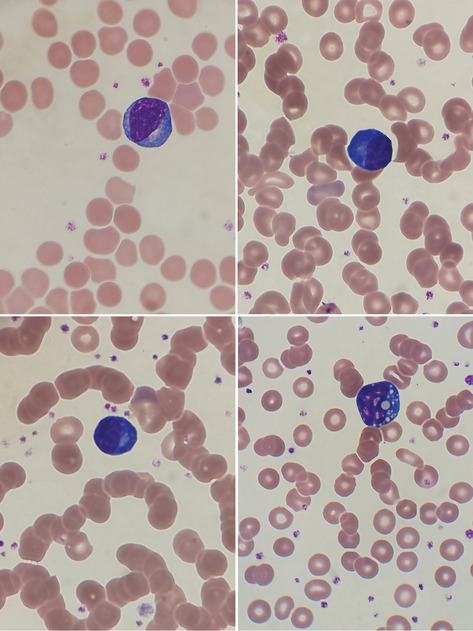 A 59‐year‐old man with no known past medical history presented to the emergency department with dyspnea, abdominal pain and malaise. Clinical assessment revealed hypoxia with bibasal crepitations on chest auscultation. A chest radiograph showed extensive bilateral air space opacification involving all zones. He was hospitalized with suspicion of infection with the novel coronavirus, SARS‐CoV‐2, later proven by positive RT‐PCR. Blood tests showed multi‐organ failure with deranged liver function tests (alkaline phosphatase 611 IU/L, alanine aminotransferase 208 IU/L, gamma‐glutamyl transferase 435 IU/L), acute kidney injury (serum creatinine 197 μmol/L), and raised inflammatory markers (C‐reactive protein 137 mg/L, ferritin 3303 μg/L). His blood count showed a hemoglobin concentration of 109 g/L, platelet count of 921 × 109/L and total white cell count of 9.8 × 109/L with a neutrophil count of 8.5 × 109/L, and a lymphopenia of 0.9 × 109/L. His blood film showed atypical lymphocytes that appeared reactive. Prominent among these were lymphoplasmacytoid lymphocytes with an eccentric nucleus, deeply basophilic cytoplasm and a prominent paranuclear hof (top and bottom left, ×100 objective). Lymphocytes with prominent cytoplasmic inclusions (Mott cells) were also seen (bottom right).
A 59‐year‐old man with no known past medical history presented to the emergency department with dyspnea, abdominal pain and malaise. Clinical assessment revealed hypoxia with bibasal crepitations on chest auscultation. A chest radiograph showed extensive bilateral air space opacification involving all zones. He was hospitalized with suspicion of infection with the novel coronavirus, SARS‐CoV‐2, later proven by positive RT‐PCR. Blood tests showed multi‐organ failure with deranged liver function tests (alkaline phosphatase 611 IU/L, alanine aminotransferase 208 IU/L, gamma‐glutamyl transferase 435 IU/L), acute kidney injury (serum creatinine 197 μmol/L), and raised inflammatory markers (C‐reactive protein 137 mg/L, ferritin 3303 μg/L). His blood count showed a hemoglobin concentration of 109 g/L, platelet count of 921 × 109/L and total white cell count of 9.8 × 109/L with a neutrophil count of 8.5 × 109/L, and a lymphopenia of 0.9 × 109/L. His blood film showed atypical lymphocytes that appeared reactive. Prominent among these were lymphoplasmacytoid lymphocytes with an eccentric nucleus, deeply basophilic cytoplasm and a prominent paranuclear hof (top and bottom left, ×100 objective). Lymphocytes with prominent cytoplasmic inclusions (Mott cells) were also seen (bottom right).
The patient was treated with supplementary high‐flow oxygen, intravenous antibiotics and intravenous fluids. He recovered and became oxygen‐independent on day 9 post‐admission, and was discharged on day 10.
The newly emerged pandemic caused by this novel coronavirus presents a challenge to health services across the world. In studies reported from China, lymphopenia was observed in 72 and 85% of patients1, 2 with reduced numbers of T cells (CD4‐positive and CD8‐positive), B cells and natural killer (NK) cells. 1 A favorable clinical course correlated with an increasing lymphocyte count and improvements in B cell numbers and CD8‐positive T cell numbers; multivariate analysis showed an adverse significance of reduced B cells, reduced CD8‐positive T cells and an increased CD4/CD8 ratio during the course of the illness. 1
Northwick Park Hospital has so far admitted more than 300 patients with Covid‐19. In our experience, the lymphocyte features illustrated above are common in blood films of patients presenting to hospital with clinically significant Covid‐19. The observation of plasmacytoid lymphocytes supports a provisional clinical diagnosis of this condition.
2. CONFLICT OF INTERESTS
The authors state there are no conflicts of interest.
Foldes D, Hinton R, Arami S, Bain BJ. Plasmacytoid lymphocytes in SARS‐CoV‐2 infection (Covid‐19). Am J Hematol. 2020;95:861–862. 10.1002/ajh.25834
REFERENCES
- 1. Wang F, Nie J, Wang H, et al. Characteristics of peripheral lymphocyte subset alteration in COVID‐19 pneumonia. J Infect Dis. 2020;221(11):1762‐1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]


