Abstract
From a large medical center in Wuhan, the epicenter of the 2019 novel coronavirus disease (COVID‐19), we report clinical features and prognosis for three women diagnosed with COVID‐19 after gynecologic oncology surgery and hospitalized in January 2020. The incidence of COVID‐19 was 0.77% (3 of 389) of total hospitalizations and 1.59% (3 of 189) of patients undergoing surgeries in the ward. The infection of severe acute respiratory syndrome coronavirus 2 may be related to the older age, comorbidities, malignant tumor, and surgery in gynecologic hospitalizations. By February 20, 2020, only two of the three patients had met the clinical discharge criteria. Given the long and uncertain incubation period of COVID‐19, screening for the virus infection should be carried out for all patients, both preoperatively and postoperatively. Postponement of scheduled gynecologic surgery for patients in the epidemic area should be considered.
Short abstract
Because of their systemic immunosuppressive status, patients with cancer are more susceptible to viral infection than healthy individuals. This article reports results of a review of medical records of three women diagnosed with COVID‐19 after gynecological surgery at a large medical center in Wuhan, China, ground zero of the 2019 novel coronavirus outbreak.
Introduction
China and the rest of the world are experiencing an outbreak of the 2019 novel coronavirus disease (COVID‐19). By February 22, 2020, the rapid spread of the virus had caused 77,041 infections and 2,445 deaths in China, and emerging cases have been reported in more than 30 countries, including the U.S., Japan, and South Korea. More than two thirds of cases and deaths from the infection occurred in Wuhan, China. On January 31, 2020, the World Health Organization declared COVID‐19, caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), a public health emergency of international concern.
Patients with cancer are more susceptible to viral infection than healthy individuals because of their systemic immunosuppressive status caused by the malignancy and anticancer treatments, such as surgery or chemotherapy; therefore, these patients might be at increased risk for COVID‐19 and have a poorer prognosis 1.
As one of the largest medical centers in Wuhan, ground zero of the outbreak, our hospital encountered patients with COVID‐19 with various medical conditions. Here, we report the results of a retrospective review of medical records from three women diagnosed with COVID‐19 after gynecologic surgery in our Gynecologic Oncology ward in January 2020; each had met the diagnostic criteria of the New Coronavirus Pneumonia Prevention and Control Program (6th edition), published by the National Health Commission of China 2.
Results
From January 1, 2020, to January 31, 2020, three women were postoperatively diagnosed with COVID‐19 in our Gynecologic Oncology ward (Union Hospital, Tongji Medical College, Huazhong University of Science and Technology). The incidence of COVID‐19 was 0.77% (3 of 389) of the total hospitalizations and 1.59% (3 of 189) among the patients undergoing surgeries in the ward and hospitalized during the same time period. There were no COVID‐19 diagnoses in the 200 patients without surgery. Among the 189 patients with gynecologic tumors who had received surgery, COVID‐19 occurred predominantly in those with malignant diseases, with comorbidities (hypertension, diabetes, and cardiovascular disease), aged >45 years, and with postoperative fever persisting for 3 days or longer (Table 1).
Table 1.
The incidence of COVID‐19 in different subgroups of patients hospitalized after gynecologic oncology surgery
| n | COVID‐19, n (%) | p valuea | |
|---|---|---|---|
| Tumor type | |||
| Malignant | 33 | 2 (6.1) | .0236 |
| Benign | 156 | 1 (0.6) | |
| Comorbiditiesb | |||
| Yes | 40 | 3 (7.5) | .0075 |
| No | 149 | 0 | |
| Age, year | |||
| >45 | 69 | 3 (4.3) | .0213 |
| ≤45 | 120 | 0 | |
| Fever ≥3 days | |||
| Yes | 9 | 3 (33.3) | <.0001 |
| No | 180 | 0 |
Fisher's exact test.
Hypertension, diabetes, and cardiovascular disease.
The detailed clinical features and disease courses of the three COVID‐19 cases are summarized in Table 2. The three patients did not report any direct contact with infected individuals, and their x‐rays and computed tomography (CT) scans of the chest did not show any abnormality preoperatively. The patients developed fever within 2 days after surgery, which persisted (highest temperatures of 38.7°C–39.4°C) despite the administration of anti‐inflammatory drugs (cephalosporin, meropenem, and moxifloxacin). One patient had a cough and significantly decreased blood oxygen. Positive CT findings showed signs of a viral pneumonia approximately 10 days after surgery in all three patients (Fig. 1), whereas two of them had a negative chest x‐ray or CT on days 4–6 postoperatively. All patients had negative results from tests of blood and throat swab samples for seven common respiratory pathogens, including respiratory syncytial virus, adenovirus, mycoplasma pneumoniae, chlamydia pneumoniae, coxsackievirus group B, the influenza B virus, and the influenza A virus. Finally, the viral DNA of SARS‐CoV‐2 was detected in the throat swab samples from the patients by using assays based on the real‐time reverse transcriptase polymerase chain reaction technique.
Table 2.
Clinical features of the three women diagnosed with COVID‐19 after gynecological oncology surgery
| Feature | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age, years | 47 | 48 | 59 |
| Residence | Wuhan | Huanggang (90 km from Wuhan) | Zhumadian (260 km from Wuhan) |
| Comorbidities | Diabetes and hypertension | Diabetes and hypertension | Hypertension |
| Known contact historya | No | No | No |
| Preoperative chest imagingb | X‐ray (−) | X‐ray (−), CT (−) | X‐ray (−) |
| Gynecologic condition | Endometrial atypical hyperplasia | Squamous cervical cancer, stage I B1 | Epithelial ovarian cancer, stage III C |
| Surgery | Hysterectomy | Radical hysterectomy | Cytoreductive surgery |
| Timing of fever onset (days after hospitalization) | 5 days | 9 days | 5 days |
| Timing of fever onset (days after surgery) | 1 day | 2 days | 1 days |
| Fever peak | 39.4°C | 38.8°C | 38.7°C |
| Cough | Yes | No | No |
| Shortness of breath or fatigue | No | No | No |
| Lowest SpO2 | 90% | 97% | 98% |
| Postoperative chest imaging, days after surgeryb | X‐ray (−), 6 days; CT (+), 9 days | CT (+), 10 days | CT (−), 4 days; CT (+), 10 days |
| White blood cells | 6.57 g/L | 3.96 g/L | 2.97 g/L |
| Lymphocytes | 0.53 g/L | 0.85 g/L | 0.67 g/L |
| CRP | 37.50 mg/L | 36.36 mg/L | 9.44 mg/L |
| ESR | 81 mm/h | 57 mm/h | NA |
| D‐dimer | 1.16 ng/mL | 9.41 ng/mL | 12.49 ng/mL |
| Procalcitonin | <0.13 μg/L | <0.13 μg/L | 0.28 μg/L |
| SARS‐CoV‐2 | Positive | Positive | Positive |
| Blood culture for bacteria | Negative | Negative | Negative |
| AST | 38 U/L | 192 U/Lc | 27 U/L |
| ALT | 29 U/L | 106 U/Lc | 20 U/L |
| Prognosis by Feb. 20 | Discharged | Discharged | In hospital |
History of direct contact with other individuals infected with SARS‐CoV‐2.
(−), no signs of a viral pneumonia; (+), images of viral pneumonia.
This patient had undergone chemotherapy for three cycles before surgery. The elevated AST and ALT may be caused by the drugs.
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C‐reactive protein; CT, computed tomography; ESR, erythrocyte sedimentation rate; NA, Not applicable; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2; SpO2, peripheral oxygen saturation.
Figure 1.
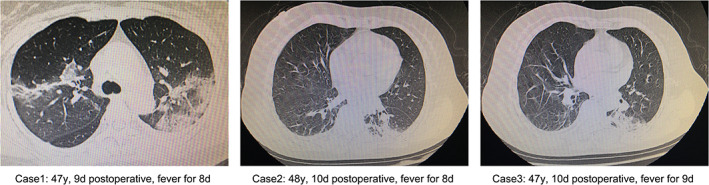
Representative chest computed tomography images of COVID‐19 in three women after gynecologic surgery: multiple regions of patchy consolidation and ground‐glass opacities in bilateral lungs, coupled with scattered lesions along the bronchial bundles or the subpleural lungs.
The patients were transferred to a quarantine hospital and treated with antiviral drugs (oseltamivir or umifenovir) combined with supportive care. As of February 20, 2020, two of the three patients had been discharged from the hospital because they had met the discharge criteria (i.e., they had neither fever nor cough for at least 3 days, the lesions of lung had become much smaller according to chest CT imaging, and repeated negative results had been obtained in at least two consecutive viral DNA tests on different days 2); at this writing, the third patient was still being treated at the quarantine hospital.
Discussion
In previous studies, nearly half of patients with COVID‐19 had underlying chronic diseases, such as diabetes, hypertension, and cardiovascular disease, and the common symptoms at onset of illness included fever, cough, shortness of breath, and fatigue. Most patients had lymphopenia, and nearly all patients had pneumonia with abnormal findings on chest CT. Some patients developed acute respiratory distress syndrome, and some of these patients worsened in a short period of time and died of multiple organ failure 3, 4. Generally, the incubation period for COVID‐19 can last 2 weeks, or longer 2, 5 considering that CT scan rather than x‐ray of the chest plays an essential role in the diagnosis of COVID‐19 and that the viral detection assays are not always available or accurate 6. In the epidemic area, it would be helpful to use CT scans to screen patients preoperatively. For patients with persisting fever after surgery, a lung CT scan needs to be done in a timely manner.
Data suggest that men are more susceptible than women, but in fact all populations are susceptible, including women 2, 3. Some studies reported that, with the rapid spread of the disease, many COVID‐19 diagnoses were made in people who had not had direct contact with other individuals infected with SARS‐CoV‐19 7. In the current study, only one of three affected persons was from metropolitan Wuhan, and the others were from nearby. In an epidemic area of COVID‐19, more intensive surveillance for SARS‐CoV‐2 should be done before surgery. After surgery, if a patient's fever lasts for more than 3 days or is accompanied by respiratory symptoms, then COVID‐19 testing should be performed, even if the patient has had no contact with other verified cases. In the present case report, the patients were older than the average age of the patients in the ward during the same time period, suggesting that age also may be a risk factor for COVID‐19 after gynecologic tumor surgery. It was also observed, in all three cases, that the white blood cell count was not high and the lymphocyte count was reduced. One important finding was that there were no COVID‐19 diagnoses in the no‐surgery group, including 200 hospitalizations. It is suggested that only emergency gynecologic operations should be scheduled in an epidemic area.
Conclusion
We found that patients undergoing gynecological surgery were at risk for clinical manifestations of COVID‐19 after surgery in a gynecologic oncology ward. Postponement of scheduled gynecologic surgery for patients in the epidemic area is important and should be considered. More intensive surveillance for SARS‐CoV‐2 should be considered for patients undergoing gynecologic surgery, especially for patients with fever for more than 3 days, older patients, and patients with comorbidities.
Disclosures
The authors indicated no financial relationships.
Disclosures of potential conflicts of interest may be found at the end of this article.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact Commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. Liang W, Guan W, Chen R et al. Cancer patients in SARS‐CoV‐2 infection: A nationwide analysis in China. Lancet Oncol 2020;21:335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Health Commission of the People's Republic of China . New Coronavirus Pneumonia Prevention and Control Program [in Chinese]. 6th ed. Beijing, China: National Health Commission of the People's Republic of China, February 19, 2020. Available at http://www.nhc.gov.cn/xcs/fkdt/202002/54e1ad5c2aac45c19eb541799bf637e9.shtml. Accessed February 20, 2020. [Google Scholar]
- 3. Chen N, Zhou M, Dong X et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guan WJ, Ni ZY, Hu Y et al.; China Medical Treatment Expert Group for Covid‐19 . Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shi H, Han X, Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019‐nCoV) pneumonia in Wuhan, China. Radiology 2020;295:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li Q, Guan X, Wu P et al. Early transmission dynamics in Wuhan, China, of novel coronavirus‐infected pneumonia. N Engl J Med 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


