Abstract
The COVID‐19 pandemic has placed an extraordinary demand on the United States health care system. Many institutions have canceled elective and non‐urgent procedures to conserve resources and limit exposure. While operational definitions of elective and urgent categories exist, there is a degree of surgeon judgment in designation. In the present commentary, we provide a framework for prioritizing head and neck surgery during the pandemic. Unique considerations for the head and neck patient are examined including risk to the oncology patient, outcomes following delay in head and neck cancer therapy, and risk of transmission during otolaryngologic surgery. Our case prioritization criteria consist of four categories: urgent—proceed with surgery, less urgent—consider postpone > 30 days, less urgent—consider postpone 30 to 90 days, and case‐by‐case basis. Finally, we discuss our preoperative clinical pathway for transmission mitigation including defining low‐risk and high‐risk surgery for transmission and role of preoperative COVID‐19 testing.
Keywords: clinical practice guidelines, COVID‐19, head and neck cancer, SARS‐CoV‐2, surgical oncology
1. INTRODUCTION
Since its initial identification in Wuhan, China, in late 2019, the novel coronavirus 2019 disease (COVID‐19) has rapidly spread across the world. In recognition, the World Health Organization (WHO) officially designated the COVID‐19 outbreak a pandemic on March 11, 2020. 1 The rapid rise in COVID‐19 cases has caused a demand surge on the United States health care system. Hospitals are already reporting shortages of necessary equipment and resources required to care for COVID‐19 patients including personal protective equipment (PPE) for frontline health care workers, ventilators, intensive care unit (ICU) beds, and transfusion capacity.
Surgical procedures increase demands on an already taxed system through the consumption of a large amount of PPE, use of inpatient beds postoperatively, and elevated risk of transmission of SARS‐CoV‐2 to other patients and staff.2, 3 The CDC recommended cancellation of all elective and non‐urgent procedures for Santa Clara County, California, on March 13, 2020. 2 Subsequent guidelines were released by the American College of Surgeons (ACS) to curtail the performance of “elective” surgical procedures 4 and the American Academy of Otolaryngology‐Head and Neck Surgery to provide only “time‐sensitive” or “emergent” care. 5 While the ACS 6 and the Centers for Medicare & Medicaid Services (CMS) 3 have published general guidelines on priority classification of cases, it is ultimately the responsibility of the surgeon to define “elective” and “urgent” surgery. The ACS, working together with specialty societies, has put forth more specific definitions of procedural classifications for other surgical specialties, 4 including cardiac, colorectal, metabolic and bariatric, pediatric, and thoracic surgery; however, to date, no otolaryngology case priority designations exist.
In response to this pandemic, the Division of Head and Neck Surgery in the Department of Otolaryngology at Stanford University has developed a process for stratifying head and neck cases by urgency. In the present commentary, we discuss considerations for case prioritization during the COVID‐19 pandemic, outline our criteria and workflow, define estimated risk categories of SARS‐CoV‐2 transmission for patients undergoing urgent head and neck surgery, and discuss the role of preoperative COVID‐19 screening.
2. HISTORICAL PERSPECTIVE
During the severe acute respiratory syndrome (SARS) pandemic of 2003 in Guangzhou, China, surgical care was dramatically impacted around the world. 7 , 8 , 9 In Toronto, a global hotspot of the pandemic, policies enacted to reduce elective operations and conserve resources were highly effective: ambulatory and elective inpatient operations declined 70% and 57% year‐over‐year, respectively, while nonelective operations requiring inpatient admission postoperatively declined less than 10%. 9 Similar declines were seen in Hong Kong, where one academic otolaryngology department had 79% lower surgical volume and 59% lower outpatient clinic visits. 8 Oncologic surgery was not delineated in these reports specifically. In less severe viral epidemics, such as the H1N1 influenza epidemic in 2009, oncologic surgery has rarely been targeted for cancellation. The Japanese experience during the H1N1 epidemic revealed only a 0.4% increase in cancellation rates. 10
Head and neck oncologic surgery will often be classified as “urgent” surgery with limited decrease in volume expected under the current policy restrictions. However, pandemic preparedness plans from the United States' Institute of Medicine and the Canadian National Advisory Committee on SARS and Public Health emphasize adherence to the three‐stage pandemic triage plan with surgical care de‐escalation dictated by the current pandemic stage.9, 11 Cancer surgical care typically would be impacted upon reaching triage level 3 (Table 1). The pandemic plans also recommend use of centralized committees within healthcare institutions to continually review and make decisions on de‐escalation of services, taking into consideration (a) consequences to patients, (b) resource requirements, and (c) ability to provide the necessary resources given altered standards of care. 11 Professional societies are recognized as critical to guide recommendations within individual surgical specialties. 11 As some head and neck surgical cases are inevitably canceled, it will also be important to monitor for growing surgical backlogs, which posed significant financial and resource hardships on the Canadian system during their recovery from the SARS pandemic. 9
TABLE 1.
Pandemic triage levels and impact on cancer surgical care
| Triage level 1 | Triage level 2 | Triage level 3 | |
|---|---|---|---|
| Early in the pandemic | Worsening pandemic | Worst‐case scenario | |
| Key signs of this stage |
|
|
|
| Modifications to hospital care |
|
|
|
| Impact on cancer surgical care |
|
|
|
Note: Adapted from Utah Pandemic Influenza Hospital and ICU Triage Guidelines. 48
Abbreviation: ED, emergency department.
3. COVID‐19 IN THE CANCER PATIENT
Patients with cancer may be at higher risk for COVID‐19 disease. Oncology patients are often recalled to the hospital and health care facilities for both treatment and monitoring. They are also more susceptible to infection because of systemic immunosuppression caused by the malignancy and anticancer therapies, such as surgery, radiotherapy, chemotherapy, and immunotherapy. A retrospective review of oncology patients admitted to a hospital in Wuhan, China from December 30, 2019 to February 17, 2020 found that patients with cancer harbored a significantly higher risk of COVID‐19 (OR, 2.31; 95% CI 1.89‐3.02) compared with the community. 12 Although current case numbers within our head and neck oncology patients remain low, ongoing community transmission and the vulnerability of our patient population suggests that this may not remain static. Not only are cancer patients more likely to become infected, but they are also more likely to have severe complications from COVID‐19. Early published reports from China on outcomes of oncology patients with the disease indicated a 3.5 times higher risk of requiring mechanical ventilation, ICU admission, or death compared to patients without cancer. 13 A review of over 72 000 COVID‐19 cases in Wuhan showed a case fatality rate of 5.6% for cancer patients compared to 2.3% for the overall population. 14
4. DELAY IN HEAD AND NECK CANCER THERAPY
The postponement of head and neck oncologic surgical cases must be weighed against potential morbidity associated with delay. Head and neck squamous cell carcinoma (HNSCC) can progress and upstage during a prolonged time to treatment initiation (TTI). 15 This may lead to an increase in mortality and likelihood of recurrence whether treated with a surgical or nonsurgical approach.15, 16, 17, 18, 19, 20, 21, 22 In addition, delayed TTI can evoke patient anxiety as the patient may feel that not enough is being done to address their cancer. 23 To establish a benchmark for quality of care and for determining what constitutes a tolerable amount of delay, prior studies have used 21 days from clinic evaluation to definitive surgery as a quality metric cutoff,24, 25 though reported threshold for delayed TTI has ranged from 20 to 120 days using different selection methods. 17
Some argue that biasing toward a nonsurgical approach for the treatment of HNSCC is indicated to conserve hospital resources, especially PPE, particularly for oropharyngeal, laryngeal, and hypopharyngeal cancers. While this certainly warrants discussion, the potential to acquire SARS‐CoV‐2 while immunocompromised, undergoing daily radiation treatments and frequent infusions would appear to present additional patient risks and increase total use of PPE. We have elected to continue a primary surgical approach when recommended at our multidisciplinary head and neck tumor board. We feel that a nonsurgical approach may actually result in increased cumulative exposure for the patient and health care system. Furthermore, at our institution, radiation oncology has been equally affected by the COVID‐19 pandemic and has experienced difficulty with resources and staffing, resulting in a delay in radiation therapy for less urgent patients. The American Society for Radiation Oncology (ASTRO) has released guidelines for the treatment of patients during the COVID‐19 pandemic which does include striving for the shortest possible course of radiotherapy including hypofractionation when appropriate. 26
5. THE RISK OF TRANSMISSION DURING OTOLARYNGOLOGIC SURGERY
SARS‐CoV‐2 is characterized by rapid human‐to‐human transmission from droplet contamination arising from the upper aerodigestive tract. 27 Early reports also suggest the possibility of aerosol transmission in the setting of aerosol‐generating procedures, such as any instrumentation of the upper aerodigestive tract. 28 Otolaryngologists, with frequent contact with the upper aerodigestive tract, are at particularly high risk for nosocomial transmission, as seen during the Wuhan outbreak. 29 Any transmucosal head and neck procedure, including flexible fiberoptic nasolaryngoscopy, should be considered high‐risk and appropriate PPE must be worn by all team members in the clinic exam room or operative suite. A thorough discussion of what constitutes appropriate PPE for these procedures is out of the scope of this commentary; however, in the authors' opinion, PPE should include N95 respirator, face shield, surgical gown, and gloves. Additional safety recommendations for the otolaryngologist have recently been made available. 30 There is debate regarding the viral load in the nasal cavity, pharynx and lower respiratory tract. A report with 17 patients suggested higher loads in the nasal cavity compared to the throat. 31 However, in a series with 82 patients, a close correlation was seen between viral load in throat swabs and sputum. 32 Further research will be required to determine variable transmission‐risk of SARS‐CoV‐2 across the head and neck surgical procedures. 33
6. CRITERIA FOR PRIORITIZING PATIENTS REQUIRING HEAD AND NECK SURGERY
Our division's case priority estimation criteria for head and neck surgery during the COVID‐19 pandemic is shown in Table 2. Cases have been classified into four major categories: urgent—proceed with surgery, less urgent—consider postpone >30 days, less urgent—consider postpone 30 to 90 days, and case‐by‐case basis.
TABLE 2.
Stratification of common head and neck surgery cases by urgency
| Urgent—Proceed with surgery |
|
HPV‐negative HNSCC (especially those with airway concerns) HPV‐positive HNSCC with significant disease burden or delay in diagnosis HNSCC patients with complications of cancer treatment Recurrent HNSCC Thyroid
Parathyroidectomy with renal function declining Skull base malignancy Salivary cancer
Skin cancer
|
| Less urgent—Consider postpone > 30 days |
|
Low‐risk PTC without metastasis Low‐grade salivary carcinoma |
| Less urgent—Consider postpone 30 to 90 days; reassess after pandemic appears to be resolving |
|
Thyroid
Parathyroidectomy with stable renal function Benign salivary lesions Skin cancer
|
| Case‐by‐case basis |
|
Rare histology with uncertain rate of progression Diagnostic procedures, such as direct laryngoscopy with biopsy |
Abbreviations: HPV, human papillomavirus; HNSCC, head and neck squamous cell carcinoma; PTC, papillary thyroid carcinoma.
6.1. Urgent—Proceed with surgery
The majority of the cases that fall into this category are mucosal HNSCC. As previously mentioned, there is evidence to suggest that delayed time to treatment initiation in HNSCC patients may result in poorer oncologic outcomes.15, 16, 17, 18, 19, 20, 21, 22 In our opinion, during triage levels 1 and 2 of the pandemic, it is reasonable to proceed with these oncologic cases to avoid delay in treatment. There is some evidence to suggest that time from diagnosis to surgery may be more significant in HPV‐negative than HPV‐positive disease. 21 Therefore, if necessary, HPV‐negative patients should be prioritized.
Additionally, we identified high‐risk thyroid cancers including anaplastic thyroid carcinoma, medullary thyroid carcinoma, metastatic papillary thyroid carcinoma (PTC), locally aggressive PTC, revision PTC with active progression of disease, and greater than 4 cm follicular lesions as urgent cases. Skull base cancers should proceed with surgery with additional precautions and PPE consideration as mentioned previously. We consider melanoma greater than 1 mm thick, Merkel cell carcinoma, advanced‐stage high‐risk cutaneous squamous cell carcinoma, as well as basal cell carcinoma in close proximity to critical areas as urgent. High‐risk cutaneous squamous cell carcinomas include those greater than 4 cm, having deep invasion beyond subcutaneous structures, perineural invasion, or poor differentiation. 34 Additional urgent cases include surgery for high‐grade salivary tumors and parathyroidectomy in patients with nephrologist or endocrinologist documentation of declining renal function.
6.2. Less urgent—Consider postpone > 30 days
We identified low‐risk PTC without metastasis and low‐grade salivary cancers as less urgent with consideration of postponement for greater than 30 days. There is strong evidence to support the surveillance of small, low‐risk PTC with low risk for tumor growth and metastasis.35, 36 Furthermore, patients with delay in diagnosis 37 and delay in surgery38, 39 of well‐differentiated thyroid carcinomas may still have excellent outcomes. Finally, the delay of thyroid surgery is often safely delayed until after delivery in pregnant patients without compromising oncologic outcomes. 40 Among salivary cancer (all histologies and grades), a national retrospective review found that TTI had no impact on 5‐year overall survival. 41
6.3. Less urgent—Consider postpone 30 to 90 days
We identified benign thyroid surgery, including goiter without airway/respiratory symptoms, benign thyroid nodules, and thyroiditis as less urgent with consideration to postpone for 30 to 90 days. Additionally, revision PTC surgery with documented stable or slow rate of progression is reasonable to postpone. Parathyroidectomy with stable renal function, benign salivary lesions, and low‐risk non‐melanoma skin cancers where cosmetic impact and morbidity is likely low with further growth should also be postponed. Recently published National Comprehensive Cancer Network (NCCN) guidelines on the management of cutaneous melanoma during the COVID‐19 pandemic recommend delaying wide local excision of melanoma up to 1 mm thickness for up to 3 months as long as the biopsy removed a majority of the lesion. 42 These cases should be reassessed and rescheduled once the pandemic appears to be resolving.
6.4. Case‐by‐case basis
In the short timeframe that case prioritization has been in place at our institution, there have already been multiple patients that do not fit any of the above designations. We recommend that these cases be discussed at either a multidisciplinary head and neck tumor board and/or divisional surgical case planning meetings so that a consensus can be reached. In addition, diagnostic procedures, such as direct laryngoscopy with biopsy, should also be discussed as many of these cases can be avoided or delayed to the day of ablative surgery.
7. SURGICAL CASE PRIORITIZATION PROCESS
The surgical case prioritization process during the COVID‐19 pandemic for the entire otolaryngology department is shown in Figure 1. All divisions, including head and neck oncology, facial plastics and reconstructive surgery, laryngology, otology and neurotology, pediatric otolaryngology, rhinology and skull base surgery, and sleep surgery follow a similar process. Each division has created case prioritization criteria for their specific sub‐specialty.
FIGURE 1.

Surgical case prioritization process during COVID‐19 pandemic [Color figure can be viewed at http://wileyonlinelibrary.com]
The process begins with the surgeon identifying a patient with an urgent clinical need requiring surgical intervention. The surgeon will then refer to the priority criteria for head and neck surgery during the COVID‐19 pandemic (Table 2) and classify the case accordingly. All patients are discussed at the weekly head and neck oncology division case review conference, which is remotely attended by all head and neck faculty. If there is lack of agreement within the division on whether the case is urgent, the patient will be discussed at our head and neck tumor board, where a multidisciplinary recommendation is rendered. For urgent cases that are recommended to proceed, the surgeon will provide documentation of urgency in the patient's electronic medical record, to be shared with anesthesia or any provider taking care of the patient to access. A summary paragraph documenting urgency is also sent to the division chief and the department chair, who reviews the request and submits all cases to the preoperative anesthesia team for screening.
8. PREOPERATIVE CLINICAL SCREENING FOR COVID‐19
Screening for and testing of SARS‐CoV‐2 may be implemented at multiple points in the patient's cancer journey. Already many outpatient clinics and preoperative anesthesia care settings are screening patients via symptom questionnaires and checking for active fever.33, 43, 44 It must be recognized that confounding symptom overlap can exist between respiratory viral pathogens and cancer, which may create additional hurdles in the screening process. 45 Patients who screen positive in the outpatient setting are immediately referred for testing as capacity exists. In recognition of the increased risk of nosocomial transmission of SARS‐CoV‐2 to health care providers during aerosol generating procedures, multiple organizations including the American Head and Neck Society, the American Academy of Otolaryngology‐Head and Neck Surgery, and the American Colleges of Surgeons are advocating for preoperative testing for all patients undergoing these high‐risk procedures.4, 12, 46, 47 Testing availability, timing of testing relative to the date of surgery, whether one or multiple negative tests are needed, and how to triage patients when found to test positive all remain important, and as yet unanswered, questions. Many local factors will thus impact decision making around preoperative testing.
Our preoperative clinical screening for COVID‐19 pathway is shown in Figure 2. Within the past week, preoperative clinical testing for selected, high‐risk procedures, has become available at our institution. If a patient is confirmed to require urgent head and neck surgery they are sent to preoperative anesthesia clinic, just as they were prior to the pandemic. Patients are then dichotomized based on surgical risk of SARS‐CoV‐2 transmission (Table 3). If no mucosa is involved during surgery, the procedure is deemed low‐risk and the patient will only be tested for SARS‐CoV‐2 (using standard polymerase chain reaction [PCR] testing) if their COVID‐19 clinical screening is positive (Table 4). If SARS‐CoV‐2 PCR testing is negative, then the surgeon may proceed with low‐risk surgery.
FIGURE 2.
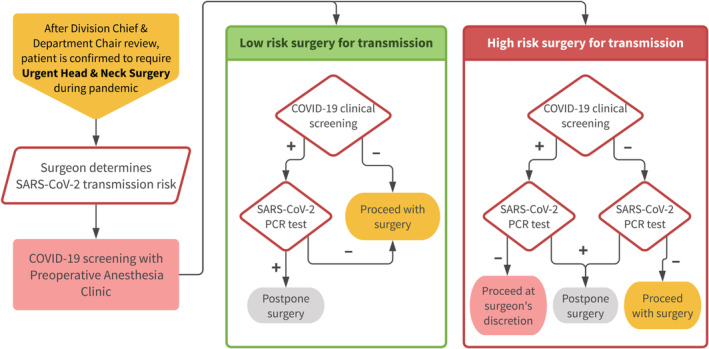
Preoperative clinical screening pathway for COVID‐19 [Color figure can be viewed at http://wileyonlinelibrary.com]
TABLE 3.
Estimated transmission risk categories for patients undergoing urgent head and neck surgery
| Low‐risk: no mucosa involved in surgery | High‐risk: transmucosal surgery |
|---|---|
|
Thyroidectomy Parathyroidectomy Neck dissection Wide local excision of skin cancers (that does not involve eye, nose, mouth, sinus) Parotidectomy Branchial cleft excision |
Any transoral procedure Glossectomy, buccal resection, floor of mouth, etc. Lateral oropharyngectomy Composite resection of the mandible Palatectomy Maxillectomy Rhinectomy Laryngeal surgery Vocal cord procedures Partial/total laryngectomy Transoral robotic surgery Direct laryngoscopy |
TABLE 4.
Preoperative COVID‐19 clinical screening
|
In the past 2 weeks, have you: 1. Traveled outside the United States? 2. Had direct contact with a COVID‐19 positive patient? 3. Had influenza‐like symptoms? 4. Fever (subjective or temp ≥ 100)? 5. Sore throat? 6. Cough? 7. Shortness of breath? |
Any trans‐mucosal surgery is considered high‐risk. For these patients, PCR testing for SARS‐CoV‐2 will be performed regardless of clinical screening status. If the patient's clinical screening is positive but SARS‐CoV‐2 PCR testing is negative, then the case may proceed at the discretion of the surgeon, given the possibility of a false negative test result. Any patient that tests positive for SARS‐CoV‐2 will have their surgery delayed, unless there is imminent threat to life (eg, impending airway compromise). We recommend retesting prior to proceeding with surgery. The patient can be considered for retesting 7 days after symptoms have receded, or 14 days after the date of the initial test, whichever is longer. The timing of oncologic surgery after positive PCR testing should be carefully considered by the patient, surgeon, and critical care team managing this potentially life‐threatening infection. PCR testing for SARS‐CoV‐2 may be associated with false negative results (without publicly available data at the time of article submission), therefore universal PPE precautions are still recommended during high‐risk procedures.
9. DISCUSSION
The recent surge in COVID‐19 cases in the United States has caused an extraordinary demand on its health care system. Many institutions have canceled all elective and non‐urgent procedures to conserve PPE, free up inpatient beds, and limit exposure of patients and staff. While operational definitions of elective and urgent categories of surgery exist, there is a degree of surgeon judgment in these designations. To ensure that our identification of a surgical patient as “urgent” is both consistent and evidence‐based, we have established a framework to prioritize patients for the operating room, risk categories for transmission, and clinical pathways for preoperative evaluation and transmission mitigation. We employ sequential reviews by division faculty (±multidisciplinary head and neck tumor board), division chief, and department chair. The classifications and pathways put forth in the current paper are meant to be a general guideline for others to use. Every institution will have its own unique considerations.
As surgeons, we bear the heavy responsibility that our decisions put the entire operating room team at risk. When a surgeon schedules an urgent case, the justification for adding it on has to be genuine. Justifications should not be hypothetical, but rather clearly documented in the patient's electronic medical record as a substantial health threat to the patient over the next 30 days. The surgeon must always consider each patient's oncologic situation, comorbid conditions, social circumstances, and needs. Given the high risk of SARS‐CoV‐2 nosocomial transmission in a majority of head and neck procedures, as head and neck surgeons we have a unique obligation to employ a conservative operational definition of “urgent.”
At times it is difficult to determine where we are on the “curve” of the pandemic. During the current exponential growth phase, we need to be relatively stringent, but we hope that these criteria will gradually liberalize over time. In the meantime, it is our responsibility to be thoughtful with our case selection and promote stewardship of health care resources.
CONFLICT OF INTEREST
The authors have no funding, financial relationships, or conflicts of interest to disclose. The content contained within the manuscript has not been presented or published in any other venue.
Topf MC, Shenson JA, Holsinger FC, et al. Framework for prioritizing head and neck surgery during the COVID‐19 pandemic. Head & Neck. 2020;42:1159–1167. 10.1002/hed.26184
REFERENCES
- 1. World Health Organization . Rolling Updates on Coronavirus Disease (COVID‐19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed March 29, 2020.
- 2.CDC's Recommendations for 30 day Mitigation Strategies for Santa Clara County, California, based on Current Situation with COVID‐19 Transmission and Affected Health Care Facilities. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/california-santa-clara-county.html.
- 3.CMS Adult Elective Surgery and Procedures Recommendations: Limit All Non‐essential Planned Surgeries and Procedures, Including Dental, Until Further Notice. https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf. Accessed March 29, 2020.
- 4.COVID‐19: Elective Case Triage Guidelines for Surgical Care. https://www.facs.org/covid-19/clinical-guidance/elective-case. Accessed March 24, 2020.
- 5.New Recommendations Regarding Urgent and Nonurgent Patient Care. https://www.entnet.org/content/new-recommendations-regarding-urgent-and-nonurgent-patient-care-0. Accessed March 20, 2020.
- 6.COVID‐19: Guidance for Triage of Non‐Emergent Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/triage. Accessed March 29, 2020.
- 7. Schull MJ, Stukel TA, Vermeulen MJ, et al. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. 2007;176(13):1827‐1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vlantis AC, Tsang RK, Wong DK, Woo JK, van Hasselt CA. The impact of severe acute respiratory syndrome on otorhinolaryngological services at the Prince of Wales Hospital in Hong Kong. Laryngoscope. 2004;114(1):171‐174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Health NACoSaP . Learning from SARS: Renewal of Public Health in Canada 2003.
- 10. Nakada HT, Matsumura T, Kodama Y, Kami M, Nishimoto H. Impact of the H1N1 influenza A virus epidemic on cancer treatment in Hyogo, Japan. Int J Infect Control. 2011;7(4). 10.3396/ijic.v7i4.8154. [DOI] [Google Scholar]
- 11. Institute of Medicine . Guidance for establishing crisis standards of care for use in disaster situations: A letter report. [PubMed] [Google Scholar]
- 12. Yu J, Ouyang W, Chua MLK, Xie C. SARS‐CoV‐2 transmission in patients with cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020. 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liang W, Guan W, Chen R, et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335‐337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239. [DOI] [PubMed] [Google Scholar]
- 15. Xiao R, Ward MC, Yang K, et al. Increased pathologic upstaging with rising time to treatment initiation for head and neck cancer: a mechanism for increased mortality. Cancer. 2018;124(7):1400‐1414. [DOI] [PubMed] [Google Scholar]
- 16. Chen MM, Harris JP, Orosco RK, Sirjani D, Hara W, Divi V. Association of time between surgery and adjuvant therapy with survival in oral cavity cancer. Otolaryngol Head Neck Surg. 2018;158(6):1051‐1056. [DOI] [PubMed] [Google Scholar]
- 17. Graboyes EM, Kompelli AR, Neskey DM, et al. Association of treatment delays with survival for patients with head and neck cancer: a systematic review. JAMA Otolaryngol Head Neck Surg. 2019;145(2):166‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Morse E, Judson B, Husain Z, et al. National treatment times in oropharyngeal cancer treated with primary radiation or chemoradiation. Oral Oncol. 2018;82:122‐130. [DOI] [PubMed] [Google Scholar]
- 19. Morse E, Judson B, Husain Z, et al. Treatment delays in primarily resected oropharyngeal squamous cell carcinoma: National Benchmarks and Survival Associations. Otolaryngol Head Neck Surg. 2018. 10.1177/0194599818779052. [DOI] [PubMed] [Google Scholar]
- 20. Morse E, Fujiwara RJT, Judson B, Mehra S. Treatment delays in laryngeal squamous cell carcinoma: a national cancer database analysis. Laryngoscope. 2018;128(12):2751‐2758. [DOI] [PubMed] [Google Scholar]
- 21. Goel AN, Frangos M, Raghavan G, et al. Survival impact of treatment delays in surgically managed oropharyngeal cancer and the role of human papillomavirus status. Head Neck. 2019;41(6):1756‐1769. [DOI] [PubMed] [Google Scholar]
- 22. Fujiwara RJ, Judson BL, Yarbrough WG, Husain Z, Mehra S. Treatment delays in oral cavity squamous cell carcinoma and association with survival. Head Neck. 2017;39(4):639‐646. [DOI] [PubMed] [Google Scholar]
- 23. Rapoport Y, Kreitler S, Chaitchik S, Algor R, Weissler K. Psychosocial problems in head‐and‐neck cancer patients and their change with time since diagnosis. Ann Oncol. 1993;4(1):69‐73. [DOI] [PubMed] [Google Scholar]
- 24. Graboyes EM, Townsend ME, Kallogjeri D, Piccirillo JF, Nussenbaum B. Evaluation of quality metrics for surgically treated laryngeal squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2016;142(12):1154‐1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Graboyes EM, Gross J, Kallogjeri D, et al. Association of compliance with process‐related quality metrics and improved survival in oral cavity squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2016;142(5):430‐437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ASTRO: COVID‐19 Recommendations and Information – Summary. https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Summary. Accessed March 30, 2020.
- 27. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization: Modes of transmission of virus causing COVID‐19: implications for IPC precaution recommendations. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed April 1, 2020.
- 29. Lu D, Wang H, Yu R, Yang H, Zhao Y. Integrated infection control strategy to minimize nosocomial infection of coronavirus disease 2019 among ENT healthcare workers. J Hosp Infect. 2020;104(4):454‐455. 10.1016/j.jhin.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Givi BS, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID‐19 pandemic. JAMA‐Otolaryngol‐Head Neck Surg. 2020. 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 31. Zou L, Ruan F, Huang M, et al. SARS‐CoV‐2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177‐1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pan Y, Zhang D, Yang P, et al. Viral load of SARS‐CoV‐2 in clinical samples. Lancet Infect Dis. 2020;20(4):411‐412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E. COVID‐19 and the otolaryngologist – preliminary evidence‐based review. Laryngoscope. 2020. 10.1002/lary.28672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Clayman GL, Lee JJ, Holsinger FC, et al. Mortality risk from squamous cell skin cancer. J Clin Oncol. 2005;23(4):759‐765. [DOI] [PubMed] [Google Scholar]
- 35. Tuttle RM, Fagin JA, Minkowitz G, et al. Natural history and tumor volume kinetics of papillary thyroid cancers during active surveillance. JAMA Otolaryngol Head Neck Surg. 2017;143(10):1015‐1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ito Y, Miyauchi A, Oda H. Low‐risk papillary microcarcinoma of the thyroid: a review of active surveillance trials. Eur J Surg Oncol. 2018;44(3):307‐315. [DOI] [PubMed] [Google Scholar]
- 37. Amit M, Rudnicki Y, Binenbaum Y, Trejo‐Leider L, Cohen JT, Gil Z. Defining the outcome of patients with delayed diagnosis of differentiated thyroid cancer. Laryngoscope. 2014;124(12):2837‐2840. [DOI] [PubMed] [Google Scholar]
- 38. Jeon MJ, Kim WG, Kwon H, et al. Clinical outcomes after delayed thyroid surgery in patients with papillary thyroid microcarcinoma. Eur J Endocrinol. 2017;177(1):25‐31. [DOI] [PubMed] [Google Scholar]
- 39. Shin DW, Cho J, Kim SY, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20(8):2468‐2476. [DOI] [PubMed] [Google Scholar]
- 40. Alexander EK, Pearce EN, Brent GA, et al. 2017 guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017;27(3):315‐389. [DOI] [PubMed] [Google Scholar]
- 41. Morse E, Fujiwara RJT, Judson B, Mehra S. Treatment times in salivary gland cancer: National Patterns and association with survival. Otolaryngol Head Neck Surg. 2018;159(2):283‐292. [DOI] [PubMed] [Google Scholar]
- 42.Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. John's Hopkins Coronavirus Center. https://coronavirus.jhu.edu/map.html Accessed March 21, 2020.
- 43. Wong J, Goh QY, Tan Z, et al. Preparing for a COVID‐19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020. 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the COVID‐19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020. 10.6004/jnccn.2020.7560. [DOI] [PubMed] [Google Scholar]
- 45. Gu J, Wu A, Li J, et al. An assessment of World Health Organization criteria for severe acute respiratory syndrome in patients with cancer. Cancer. 2004;100(7):1374‐1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.How COVID‐19 is Affecting our Head and Neck Community: AHNS COVID‐19 Bulletin. https://www.ahns.info/covid-19-2020/. Accessed March 30, 2020.
- 47.AAO‐HNS Position Statement: Otolaryngologists and the COVID‐19 Pandemic. Accessed March 30, 2020.
- 48.Utah Pandemic Influenza Hospital and ICU Triage Guidelines. In: Health UDo, ed. 2009.


