The Centers for Disease Control and Prevention (CDC) recently released a list of risk factors for Coronavirus Disease 2019 (COVID‐19). Among those at greatest risk in the COVID‐19 pandemic are people aged 65 and older, 1 severely obese people (BMI ≥ 40), 1 those who are immunocompromised, 1 and those who smoke or use e‐cigarettes. 2 People with other underlying medical conditions like diabetes, 1 high blood pressure, 1 and heart conditions 1 are also at greater risk. Given the novel nature of the virus, 3 its median incubation period of 5.1 days, 3 its temporal overlap with seasonal influenza, and its basic reproduction number (R0) of 2.2 (each infected individual is expected to infect 2.2 other individuals 4 , 5 ), large‐scale testing is of the utmost importance to mitigate its spread.
COVID‐19 appeared in late December 2019 in Wuhan, Hubei Province, China, 5 and in the United States in January 2020 in the State of Washington. 6 , 7 As of this writing, COVID‐19 has spread to nearly all countries, been confirmed in all 50 US states, and been declared a pandemic. 8 Given that the virus is expected to be more infectious than the season flu and its other clinical features, the rate of reproduction is likely higher in large, urban areas due to greater reproductive opportunities afforded by denser populations. 4 Currently, New York City, NY; Seattle, WA; and New Orleans, LA are “hot spots” that are experiencing large case growth rates. However, little attention is being given to more rural areas of the country. 8
Testing began early on in Washington State, neighboring states, and generally urban areas. 8 , 9 By far, the largest number of tests have been performed in the earliest infected states, but there remains something to be examined about the states’ rates of testing. As of March 29, 2020, more than 890,000 tests have been performed in the United States, yielding—using US Census Bureau data 10 —approximately 2,711 tests per 1,000,000 population. Monnat showed that statewide rates of testing were inversely related to all‐cause mortality rates and to percent rurality, suggesting that the least healthy, rural states have the poorest rates of COVID‐19 testing. 12 We offer a complementary commentary on the surveillance of COVID‐19 and its risk factors in rural populations. Our analyses suggest that rural states—ranked higher in specific risk factors like hypertension, 1 obesity, 1 diabetes, 1 lung cancer, 1 and e‐cigarette use 2 —are performing tests at lower rates. Moreover, we find that despite these vulnerabilities, rural states are detecting disproportionately fewer cases of COVID‐19.
Testing count and result data have been compiled and aggregated at the state level by the COVID Tracking Project daily. 11 Rate of testing per 100,000 population and percent of tests positive were calculated for each state using the total number of tests performed since testing data first became available to March 29, 2020. Estimated 2019 US Census Bureau population values 10 were used to report on a per capita basis and normalize by population size. State‐level risk factor data were obtained from the 2018 Behavioral Risk Factor Surveillance Survey (BRFSS) dataset. 13 Given the fact that testing rates must be a positive integer and lag in test availability—yielding lower rates at a greater frequency than higher ones—a large positive skew (1.47) was observed in the distribution of testing rates per 100,000 and a non‐parametric approach was deemed appropriate for further analyses. Spearman's Rho (ρ) correlation transforms all values into ranks and is robust to outliers and violations of normality. 14 Therefore, the interpretation of the data is always in the context of ordinality. All analyses were performed in JMP Pro 14. 15
There were several significant bivariate inverse correlations between ranks of state‐level COVID‐19 testing rates per 100,000 and COVID‐19 risk factors including hypertension prevalence (ρ = −0.6158, P < .0001), obesity prevalence (ρ = −0.6165, P < .0001), diabetes prevalence (ρ = −0.5654, P < .0001), lung cancer prevalence (ρ = −0.3912, P = .0045), and e‐cigarette use (ρ = −0.4167, P = .0024) (Table 1). However, the percent positive tests were found to have significant positive bivariate correlations with hypertension prevalence (ρ = 0.4218, P = .0021), diabetes prevalence (ρ = .3469, P = .0126), and lung cancer prevalence (ρ = 0.3545, P = .0107). Figure 1 shows the scatterplot matrix of all aforementioned correlations with lines of best fit. It should be emphasized that despite the inclusion of the line of best fit, this does not indicate a linear relationship 14 ; rather it suggests there is a significant tendency for the testing rates per 100,000 to change monotonically with the risk factors and warrants further analyses. States ranked higher in prevalence of specific COVID‐19 risk factors (hypertension, diabetes, and lung cancer) are ranked significantly higher in percent positive tests and simultaneously ranked lower in overall testing rates. Taken together, these results suggest that current COVID‐19 surveillance is not capturing medically vulnerable populations effectively. Testing is vital in rural areas as it is clear that the population there will be more susceptible to the virus, its symptoms, and its fatal outcomes.
Table 1.
Spearman Correlations for Test Rate per 100,000, percent positive tests, and risk factors
| Hypertension | Obesity | Diabetes | Lung cancer | E‐Cigarette use | |
|---|---|---|---|---|---|
| Percent positive tests | 0.4218 ** | 0.1093 | 0.3469 * | 0.3545 * | 0.1270 |
| Test rate per 100,000 | −0.6158 ** * | −0.6165 *** | −0.5464 *** | −0.3912 ** | −0.4167 ** |
*P < .05, ** P < .01, *** P < .001
Figure 1.
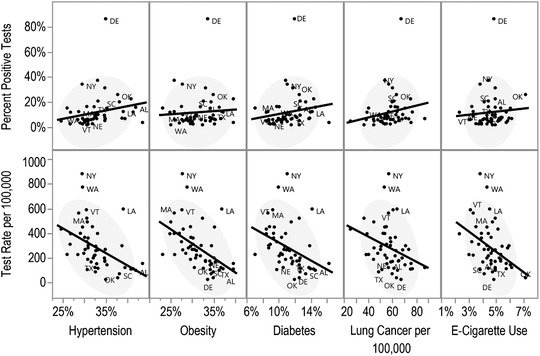
Testing and Positive Testing Rates Correlated with Health Risk Factors
Source. The Covid Tracking Project, 11 BRFSS 2018, 13 and the US Census Bureau. 10 Testing rates reflect data collected until March 29, 2020. Only states at the 1st and 9th decile of testing rate per 100,000 are labeled for sake of visual clarity.
Rural‐urban disparities in COVID‐19 testing rates only exacerbate the surveillance of an already clinically evasive, 3 , 5 novel virus. 8 Considering the greater travel distance and diminishing capacities of rural hospitals 16 —and that rural physicians tend to be older 17 and at greater risk themselves—residents of rural areas face unique and complex challenges beyond those experienced in urban areas. Given our analyses we advocate for expanded testing in rural areas. Currently, testing availability and screening criteria vary widely by state. 9 , 17 Large discrepancies in percent positive tests suggest that specific states with higher rates of positive tests may require a greater degree of screening certainty before tests are performed. Considering the clinical features of the virus and its incubation period, 1 , 2 , 3 , 4 current testing policies may be failing to detect asymptomatic cases at an effective rate. Underreporting of the incidence of COVID‐19 could lead to a false sense of security among rural populations and lead to neglect of safety guidelines recommended by the CDC. 18 Granted, case counts are expected to be lower in rural areas due to lower population density, but there is greater potential for the medically vulnerable among rural populations to succumb to the virus at the burdensome nexus of underlying conditions, 1 lack of access to care, 16 and dwindling resources and then ultimately contribute to significant disparities in COVID‐19 mortality. Finally, more complete knowledge about the size and scope of the pandemic is vital to ensure an effective allocation of resources and assistance. A continued lack of effective surveillance in rural areas has the potential to allow the virus to be transmitted among asymptomatic individuals within the incubation period 3 and spread the virus into surrounding urban areas and hinder broader mitigation efforts. 17 , 18
Acknowledgment: We would like to thank Julia Wolf, MA, for her feedback on an earlier draft.
References
- 1. CDC . People who are at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html. Updated March 26, 2020. Accessed March 30, 2020.
- 2. NIDA . COVID‐19: potential implications for individuals with substance use disorders. National Institute on Drug Abuse website. https://www.drugabuse.gov/about-nida/noras-blog/2020/03/covid-19-potential-implications-individuals-substance-use-disorders. March 24, 2020. Accessed March 31, 2020.
- 3. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID‐19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020. 10.7326/M20-050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Delamater PL, Street EJ, Leslie TF, Yang YT, Jacobsen KH. Complexity of the basic reproduction number (R0). Emerging Infect Dis J. 2019;25(1). 10.3201/eid2501.171901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Eng J Med. 2020;382:1199‐1207. https://www.nejm.org/doi/full/10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Eng J Med. 2020;382:929‐936. https://www.nejm.org/doi/full/10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coronavirus in the U.S.: Latest map and case count . Nytimes.com. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html. Published 2020. Accessed March 29, 2020.
- 8. World Health Organization . WHO announces COVID‐19 outbreak a pandemic. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic. Published March 12, 2020. Accessed March 29, 2020.
- 9. Achenbach J. Three months into the pandemic, here's how likely the coronavirus is to infect people. The Washington Post. https://www.washingtonpost.com/health/three-months-into-the-pandemic-here-is-what-we-know-about-the-coronavirus/2020/03/28/6646f502-6eab-11ea-b148-e4ce3fbd85b5_story.html. Accessed March 28, 2020. [Google Scholar]
- 10. U.S. Census Bureau QuickFacts: United States . https://www.census.gov/quickfacts/fact/table/US/PST045219. Accessed March 28, 2020.
- 11. The COVID Tracking Project . https://covidtracking.com/. Accessed March 26, 2020.
- 12. Monnat SM. Why coronavirus could hit rural areas harder. 2020. https://lernercenter.syr.edu/2020/03/24/why-coronavirus-could-hit-rural-areas-harder/. Accessed March 26, 2020.
- 13. CDC . Behavioral risk factor surveillance system: about BRFSS. https://www.cdc.gov/brfss/about/index.htm. Accessed March 29, 2020.
- 14. Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69‐71. [PMC free article] [PubMed] [Google Scholar]
- 15. JMP Pro 14 [computer program]. Version 14. Cary, NC: SAS 1989–2019.
- 16. Skinner L, Staiger DO, Auerbach DI, Buerhaus PI. Implications of an aging rural physician workforce. N Eng J Med. 2019;381(4):299‐301. [DOI] [PubMed] [Google Scholar]
- 17. Gamio L, Cai W, Hassan A. Where the U.S. Stands Now on Coronavirus Testing. The New York Times. https://www.nytimes.com/interactive/2020/03/26/us/coronavirus-testing-states.html. Published March 26, 2020. Accessed March 28, 2020.
- 18. CDC . Implementation of mitigation strategies for communities with local covid‐19 transmission.; 2020:1‐10. https://www.cdc.gov/coronavirus/2019-ncov/downloads/community-mitigation-strategy.pdf. Accessed March 30, 2020.


